Revision and Infected Total Knee Arthroplasty
Henry D. Clarke
William J. Casey III
Mark J. Spangehl
Indications/Contraindications
Soft tissue management in revision and infected total knee arthroplasty (TKA) is an extremely important factor in determining the success or failure of the procedure. Without optimal wound healing, complication rates increase and the ultimate benefit of the operation may be diminished. Despite the critical role played by the soft tissues surrounding the knee, very little scientific data exist to help guide the practicing orthopaedic surgeon in this area. Rather, most of the recommendations and guidelines are based on extrapolations from other surgical fields and anecdotal experience from experts in knee arthroplasty. In this chapter, important factors that should be considered in the preoperative, intraoperative, and postoperative settings are reviewed. In addition, surgical techniques that may minimize potential soft tissue problems and help manage complications when they do occur are also presented. The soft tissues about the knee include skin and subcutaneous coverage, as well as the extensor mechanism; therefore, in this chapter management of both of these important components is addressed.
The very circumstances that necessitate revision TKA in the settings of either infection or aseptic failure require that every patient be considered at risk for soft tissue complications. Therefore, every patient in whom revision TKA is being considered should be thoroughly evaluated preoperatively. This allows all necessary plans to be addressed in order to meet individual needs. Indeed, absolute indications and contradictions are difficult to define: rather, all factors should be considered. While any patient who undergoes revision TKA should be considered at risk for soft tissue complications, some patients will have greater risks. A healthy patient with just one prior knee surgery, with aseptic loosening, is at less risk than a patient with diabetes and peripheral vascular disease who has a chronically infected total knee replacement. However, each patient should be carefully assessed. Certainly, once the risks have been evaluated, a decision to proceed with revision TKA surgery should be based on the individual circumstances. In each case, the current symptoms, including pain and disability, presence or absence of prosthetic infection, and age and activity demands of the patient, must be evaluated in the context of the potential risks. The potential increase in symptoms, time frame for deterioration, and additional surgical problems that may be encountered by delaying surgery should also be considered. Absolute contraindications for revision TKA include irreversible medical comorbidities that raise the risk of perioperative mortality to unacceptable levels, an avascular extremity where revascularization options have been exhausted, uncontrolled sepsis, and neurologic injuries with no motor function of the extremity. Relative contraindications include failed prior soft tissue flaps, massive bone loss, recurrent prosthetic infection, extensor mechanism disruption, and unstable medical comorbidities that require optimization. When the potential risks are too great, or when other rare circumstances are encountered, such as life-threatening sepsis or an avascular limb, alternative procedures including permanent resection arthroplasty, knee arthrodesis, or amputation may be required.
Preoperative Planning
Preoperative planning is critical for minimizing soft tissue problems about the knee. Both systemic factors and the characteristics of the knee and leg should be considered before revision knee surgery.
Systemic Factors
Patient-specific medical comorbidities should be assessed and treated before surgery (Table 27-1). While optimization of these conditions appears to reduce the risk of developing wound complications after revision TKA, the increased risk of wound problems in many cases is multi-factorial and does not return to baseline levels even when medical management is optimal. For example, the increased risks of delayed wound healing and infection noted in patients with diabetes appears to be caused by both the hyperglycemia, which has been shown to inhibit collagen synthesis, disrupt fibroblast proliferation, slow capillary in-growth, and deficiencies in polymorphonuclear neutrophil cell function. Furthermore, the increased risk of soft tissue complications in patients with rheumatoid arthritis is likely due to numerous factors including the long-term sequelae of corticosteroid use, which regulates macrophage function, reduces collagen synthesis, and delays vascular in-growth, as well as direct causes of the disease itself such as skin atrophy, decreased albumin, and vasculitis.
Another important risk factor in the pre- and postoperative periods is the use of tobacco products. Nicotine and its metabolites cause vasoconstriction, which interferes with micro-circulation; however, the effects on wound healing are more profound than from vasoconstriction alone. Other constituents of tobacco smoke, such as carbon monoxide, reduce the oxygen carrying capabilities of hemoglobin, which reduces tissue oxygenation. Nicotine also appears to have a direct effect on fibroblast and immune function. The optimal time for smoking cessation appears to be 4 to 8 weeks preoperatively, but even a week of abstinence appears to reduce the risk of complications. Abstinence in the entire postoperative period is also critical. For elective procedures, all patients who smoke and have other risk factors for wound healing must stop smoking before the procedure. In some cases, professional services must be used to achieve this end. The use of nicotine delivery substitutes are controversial, as these do not eliminate the patient’s use of nicotine but do eliminate multiple other toxic substances that are inhaled in tobacco smoke, such as carbon monoxide and hydrogen cyanide. Therefore, while not an optimal solution, in certain circumstances these substitutes may be preferable to reduce the overall risk.
Table 27-1. Complicating Comorbidities | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
The Knee
The local vascular anatomy of the knee can be unforgiving; in comparison to the hip, where wound necrosis is rarely a problem. Most of the perfusion to the skin is derived from perforator vessels that originate below the level of the deep fascia. Little subcutaneous communication occurs; rather, the perforating vessels connect at the level of the sub dermal plexus. Thus, when raising skin flaps about the knee, the dissection should be below the level of the deep fascia, rather than in the sub dermal plane to avoid damaging this superficial plexus. While the peri-patellar plexus formed by the medial and lateral, superior and inferior genicular arteries has been well described, the majority of the inflow to the skin appears to be derived from the medial side of the knee in the distribution of the saphenous and descending genicular arteries. Therefore, laterally based flaps should be avoided and any prior laterally biased vertical incision should be carefully considered when selecting the optimal incision. On the lateral side, the perforators from the superior and inferior genicular arteries are relatively more important, and it has been reported that use of a lateral patellar release with disruption of the superior genicular artery is associated with decreased tissue oxygenation and increased lateral wound problems. Some general guidelines for selection and placement of skin incisions follow.
A single, longitudinal anterior midline incision provides the most extensile exposure and is preferred for all revision and infected total knee replacement cases. Prior incisions about the knee should be carefully evaluated. Factors that are believed to be important, although little scientific data exist to support these suppositions, include age, orientation, length, and placement in relation to other or intended incisions. A single, transverse incision can be crossed by a new perpendicular anterior incision with relatively little concern. When a single, prior longitudinal anterior incision exists, this incision should be used. If placement of this prior incision is not directly midline, the proximal and distal ends of the incision may be extended back toward the midline to reduce tension on the wound. In these cases, subcutaneous dissection should be minimized; it is critical to maintain full-thickness flaps if the subcutaneous tissues must be mobilized to allow adequate exposure of the extensor mechanism. To preserve the sub dermal plexus, these flaps should be raised at the level of the deep fascia. If the prior incision is located far from the midline, and would necessitate creation of a large laterally based subcutaneous flap, one may consider using a new incision. In these circumstances, skin bridges greater than 3 to 5 cm should be maintained between the new and old incisions. When multiple incisions, or a single anterior incision located well away from the midline, are encountered, selection of the optimal incision should be carefully considered. In some circumstances where numerous prior incisions exist, or where the skin and subcutaneous tissues have been severely damaged by prior trauma, radiation exposure, infection, or are atrophic, due to systemic conditions, preoperative soft tissue management techniques that are described in following sections, such as soft tissue expansion or soft tissue flaps, may be required. Again, little definitive data exist to guide the surgeon when these interventions are absolutely required; rather, much of this assessment is subjective.
Surgery
Soft Tissue Procedures
Sham Incision
Technique
The sham incision or delay procedure is reviewed primarily for its historical significance as an early attempt to manage patients considered at risk for wound healing problems after TKA. Approximately 10 to 14 days before the planned knee procedure, the intended skin incision is made and extended to the level of the extensor mechanism. Next, the skin is undermined on both sides of the incision to expose the extensor mechanism, as required for the upcoming knee replacement, and then the incision is closed and observed. If the wound heals without complications, the intended knee procedure is subsequently performed. If skin necrosis occurs, a soft tissue flap is performed before knee replacement. The main advantage in these cases is that the knee joint has not been violated, and there is no prosthesis at risk for infection. Furthermore, increased collateral flow caused by the incision due to the delay phenomenon was felt to reduce the risk of subsequent wound
healing problems. More contemporary soft tissue expansion techniques have, for the most part, eliminated the use of the sham incision.
healing problems. More contemporary soft tissue expansion techniques have, for the most part, eliminated the use of the sham incision.
Results
There is little except anecdotal evidence to support the use of this technique. Rothaus has detailed the outcomes in a small group of 12 patients, with multiple prior incisions, in whom this technique was used. In all 12 patients, the incisions healed and TKA was successfully performed without wound healing problems.
Soft Tissue Expanders
Technique
The concept of tissue expansion is not new and has been successfully used in a variety of soft tissue reconstructive procedures throughout the body. Despite the challenges posed by the unforgiving nature of the vascular supply around the knee, the use of tissue expanders is a relatively new concept with only a limited number of large patient series.
Tissue expansion has three important benefits that aid wound healing in the overlying soft tissues. First, and probably most important, it stimulates neo-vascularization of the overlying soft tissue; this improves the capillary in-flow that directly promotes healing. Second, it physically expands the overlying skin and subcutaneous tissue allowing larger areas, due to correction of malalignment or limb lengthening, to be covered. This also reduces the tension on the wound. This expansion is not simply a stretching and thinning of the overlying soft tissue, which would leave the flap less resilient, but actually a hypertrophy of the dermis and epidermis due to fibroblast stimulation, leading to an increase in the quantity of tissue available. Third, a fibrous capsule develops around the expander, and this thick, robust, vascular tissue is very useful as a “pseudo-fascial” layer to close over the joint and is particularly helpful in the area of the proximal medial tibia where the periosteum and soft tissue layer can be thin.
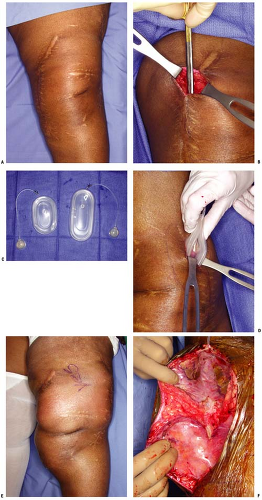
The technique for soft tissue expansion over the knee is begun approximately 6 to 8 weeks prior to the intended TKA (Fig. 27-1). Typically two to four 200 to 300 mL expanders are placed in pockets deep to the subcutaneous layer, just above the fascia (see Fig. 27-1C). These pockets are strategically placed based on the placement of prior incisions and characteristics of the overlying subcutaneous tissue and skin. The first step involves infiltrating the deep subcutaneous layer with a dilute solution composed of 1000 mL Ringer’s lactate, 50 mL 1% lidocaine, and 1 mL 1:1000 epinephrine to create a pocket. Typically, injection of 250 to 300 mL of this solution is sufficient to produce the hydro-dissection that separates the skin and subcutaneous tissue from the underlying fascia to create a pocket. Also, use of the local anesthetic helps with postoperative pain relief. Next, through a short incision placed in one of the prior incisions, scissors are used to bluntly define and enlarge this plane within the deep subcutaneous tissue to create a pocket (see Fig. 27-1B). The un-inflated expander is then inserted through the same incision (see Fig. 27-1D). The access port to the expander is then tunneled through the subcutaneous tissue to an easily accessible site. The port should be accessed prior to skin closure and saline injected to ensure that the port is functional and that the expander was not damaged during the insertion. After this initial expansion, the incision is closed and a sterile dressing applied. Patients are typically placed in a knee immobilizer for a week and allowed to weight bear as tolerated. Most patients are admitted for an overnight stay and treated with 24 hours of intravenous antibiotics. Subsequently each week, about 10% to 15% of the volume of the expander is infused with the patient as an outpatient, via the access port. If at any time the overlying skin blanches and doesn’t recover after a few minutes of observation, or if the patient experiences significant pain, saline must be removed until the problem is alleviated.
At the time of the intended TKA, the expanders are extracted through the incision used for the procedure (see Fig. 27-1F). The subcutaneous tissue and skin flaps should be protected during the TKA. At the end of the procedure, a superficial drain is placed in each individual expander pocket. These drains are removed individually once output is less than 10 mL per 8 hours or 30 mL per 24 hours. This protocol appears to reduce the risk of subcutaneous hematoma formation. Early in the experience of tissue expansion about the knee when subcutaneous drains were not routinely employed, hematomas occurred more frequently and occasionally had to be drained to reduce tension on the overlying tissue. During wound closure, the expansion process may have created excessive amounts of soft tissue that need to be excised. In these cases, the edge of the flap, especially focusing on old widened scars, can be trimmed or removed. However, the tension on the wound should not be increased by resecting too much surplus tissue.
Results
Few large series of tissue expansion in association with TKA have been published, with most reports presenting only a handful of cases. The morbidity associated with the use of tissue expanders has been previously reported and includes infection, hematoma, expander rupture or deflation, and skin necrosis. Two significant papers have reported very favorable results. In an initial study, no significant complications occurred during the expansion process in a small group of 10 patients. In a second larger group of 29 knees, six (21%) minor wound complications occurred during expansion, including mild erythema or skin blistering. These complications were successfully managed by reducing the volume in the expander, and delaying further expansion until the problem resolved. In this same group, one major complication occurred after the insertion of the soft tissue expanders; this involved full-thickness skin necrosis in a patient with a history of radiation to the anterior knee. The knee replacement was subsequently not performed, as the patient declined to accept a prophylactic muscle flap, choosing to endure her arthritic symptoms.
Following the knee replacement, 5 (18%) of 29 patients experienced minor complications; three knees developed persistent drainage, and two knees developed subcutaneous hematomas. The persistent drainage resolved after wound compression and immobilization was initiated. The two subcutaneous hematomas required surgical evacuation, and it was these problems that prompted the use of subcutaneous drains in the expander pockets.
Soft Tissue Flap Coverage Procedures
Soft tissue flap procedures about the knee have been used both prophylactically and for salvage of wound complications about the knee. Although a large number of different techniques have been described, including simple skin grafts, random or axial pattern skin flaps, fasciocutaneous flaps, and rotational or free muscle flaps, the most reliable and most frequently used tissues about the knee include medial gastrocnemius muscle flaps, and free latissimus dorsi or rectus abdominus flaps. In addition
to these techniques, the development of musculocutaneous perforator flaps during the past decade has provided another alternative for coverage about the knee. The principles involved in these three types of techniques are described following in ascending order of the extent of the area that can be adequately managed.
to these techniques, the development of musculocutaneous perforator flaps during the past decade has provided another alternative for coverage about the knee. The principles involved in these three types of techniques are described following in ascending order of the extent of the area that can be adequately managed.
Musculocutaneous Perforator Flaps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree