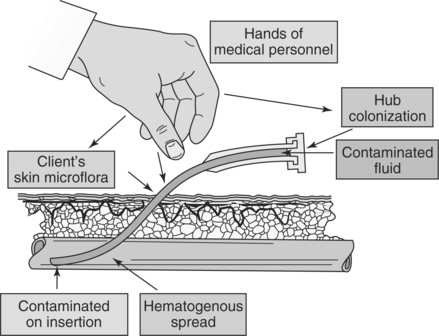
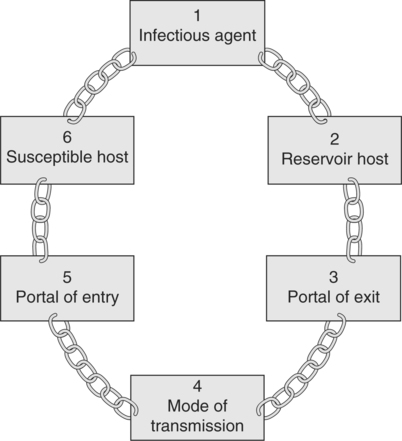
Chapter 3 Upon successful completion of this chapter, the student will be able to: • Explain the importance of quality hand hygiene. • Explain the difference between medical aseptic technique and sterile technique. • Discuss the importance of maintaining sterile technique in the administration of IV fluids. • List and discuss Universal Precautions related to IV therapy. Infection control is a major factor in patient safety with intravenous (IV) therapy. Handwashing/hand hygiene, medical asepsis, and sterile technique all play a part in infection control. Compliance with Occupational Safety and Health Administration (OSHA) guidelines and Universal Precautions also contribute to initiating and maintaining infection control. Other factors that may affect the incidence of infection in a patient include natural defenses against infection such as an intact skin, a functional immune system, and the person’s general state of good health (or homeostasis). Additionally, the type of microorganism and its state of mutation for antibiotic resistance are involved in the progression or arresting of an infection. The presence of normal body flora on the skin is always a factor in the possibility of infection during IV therapy, because the normal flora may be injected under the skin as it is punctured by the needle (Figure 3-1). Proper cleansing of the skin prior to the initiation of the IV therapy is essential to prevent this contamination. Although any of the aforementioned antiseptics may be used to cleanse the skin prior to the insertion of a catheter, cannula, or needle, chlorhexidine gluconate is usually preferred. The skin must be gently and thoroughly scrubbed or cleansed with the selected antiseptic solution and then allowed to air dry for a minimum of 2 minutes. Once the insertion is completed a sterile dressing is applied to the site. Refer to Chapter 8 for additional information on dressings. A factor in the prevention of infection is an understanding of the chain of infection and those factors that encourage the growth of microorganisms (Figure 3-2). For pathogens to be transmitted from one host to another, the following six elements of the chain of infection must be included: • Means of exit from the host (portal of exit from the host) • Means or method of transmission from the first host to the next host (mode of transmission) • Means of entrance into the next host (portal of entry into the susceptible host) Ways to break the chain of infection include the following: 1. For infection to occur, a microorganism with the ability to become a pathogen must be present. Because this pathogen is necessary, breaking the chain of infection before transmission is the best manner to prevent cross-contamination between patients. The growth, reproduction, and survival of causative microorganisms can be halted or impaired by sanitization, sterilization, antiseptics, anti-infectives, or disinfection. The infective agents can be held at bay by depriving them of needed nutrients, thus impairing their potential for growth, reproduction, and survival. Another step in preventing the causative microorganism from surviving and being transmitted to others is to provide appropriate isolation for patients with communicable diseases. 2. The progress of transmission of the microbe from the source host may be blocked, the causative microorganism may be destroyed or reproduction may be prevented, or exposure to the microorganism may be limited. Additionally, it is imperative that health care providers who are ill stay at home rather than appear in the workplace to expose others. Adherence to good hand hygiene and strict sanitization, as well as use of standard precautions and proper disposal of all sharps also is imperative in prevention of the release of the microorganism from the host source. Adhering to the principles of medical and surgical asepsis is an essential method of reducing the incidence of transfer of microorganisms from the source host. 3. In the chain of infection, the causative microorganism requires portal of exit from the reservoir host. Once again, strict adherence to the principles of Standard Precautions, good hand hygiene, use of personal protective equipment (PPE), and proper handling of specimens along with disposal of contaminated articles is helpful in preventing the probability of release of the microorganisms from the reservoir host. Avoiding coughing; sneezing; or talking into another’s face, eyes, open wounds, or lesion reduces the risk of spreading the microorganisms. 4. Another means of breaking the chain of infection is to interfere with the method or mode of transmission. Many of the essential guidelines for infection control apply in this aspect of slowing or preventing the transmission of microorganisms. Included is the practice of hand hygiene, strict sanitization, proper sterilization or disposal of used equipment and supplies, good or proper hygienic practices, and avoidance of direct contact with contaminated articles. Other techniques include not allowing items to touch the floor and not shaking linens. Spills should be cleaned and disinfected promptly. When the microbes have no means of traveling to the susceptible host, the chain of infection is interrupted. 5. A portal of entry into the susceptible host is necessary for the chain of infection to continue. Immunizations of healthy potential hosts and isolation of immunocompromised individuals help to protect from the invasion of potential pathogens. Intact skin and mucous membranes are important in the prevention of entry of pathogens. Once again, hand hygiene, proper handling of specimens, proper sharps disposal, and proper disposal of contaminated articles are important steps in reducing the prevention of pathogens entering the host. Additionally, wounds should be covered and any open possible entry sites should be covered or protected. Taking these precautions is necessary to break the transmission of pathogens. 6. A susceptible host, including the very young, the aging population, and those who may be immunocompromised at higher risk, is necessary for the transmission of the possible pathogen. To interrupt the chain of transmission, these groups of individuals may require extra precaution. Some of the extra precautions include proper nutrition, protective isolation, visitor limitation, and reduction of stress. Proper and frequent hand hygiene, as always, is an excellent tool in preventing the susceptible host from being exposed. Finally, judicious use of antibiotics throughout the years helps to prevent the mutation of antibiotic-resistant pathogens, providing a means of fighting infections that do occur.
Review of Asepsis
TYPES OF PATHOGENS
CHAIN OF INFECTION
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine