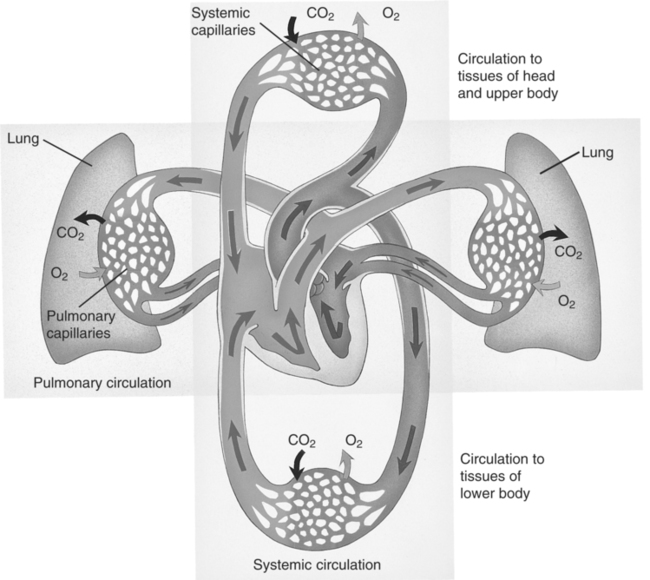
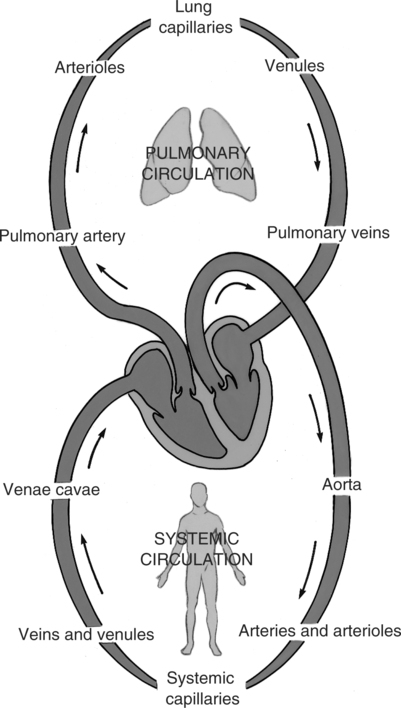
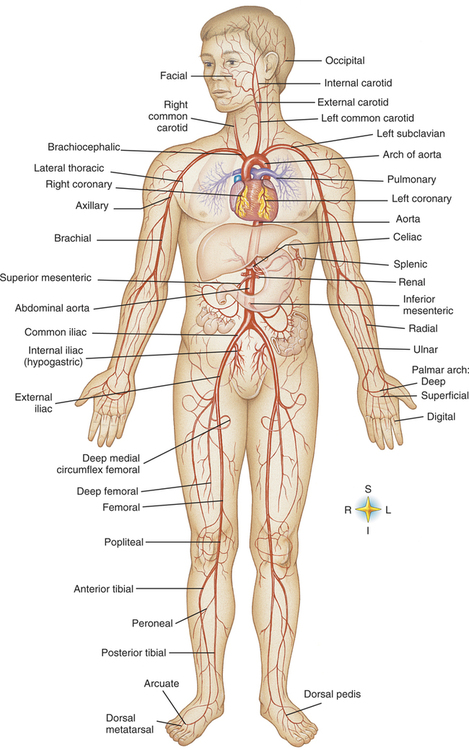
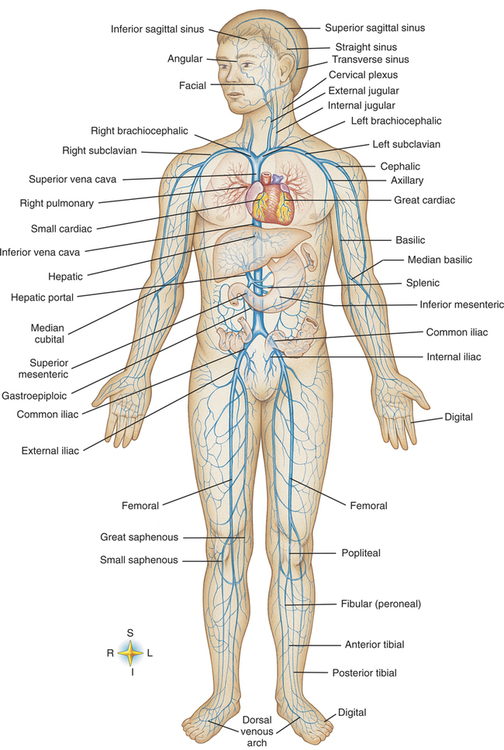
Chapter 2 Upon successful completion of this chapter, the student will be able to: • Identify and discuss an overview of anatomy and physiology of the entire circulatory system • Identify and discuss the blood vessels in the upper extremity that are used for therapy • Discuss homeostasis as it applies to IV therapy • Identify and discuss the lymphatic system as it pertains to IV therapy • Discuss peripheral nerves in the arms as they pertain to IV therapy the main trunk arterial vessel (artery) that leaves the left ventricle and carries blood to systemic arteries. heart valve between left ventricle and aorta. very small arteries at the distal end of the arterial network that carry blood to the capillaries. blood vessel that carries blood away from the heart that in most cases is oxygenated. minute blood vessels that connect the smallest arterioles to the smallest venules. The walls of capillaries are a single layer of epithelial cells enabling blood and tissue fluid the ability to exchange various substances (gases, fluids, electrolytes, salts, and nutrients). movement of particles or molecules from an area of higher concentration in fluids to one of lower concentration to achieve more equal distribution of particles/molecules in the fluid or liquid. outside the cell. process in which particles are removed from solution by passing the liquid through a membrane or filter. state of dynamic balance in the body. pressure exerted on a liquid. large vein that collects blood from parts of the body below (inferior to) the heart for return to right atrium. pertaining to space between cells. extracellular fluid in the spaces between body cells providing a substantial portion of liquid environment of the body. within the cell. fluids within the blood vessels. left upper chamber of the heart; receives blood from the pulmonary veins. left lower chamber of the heart; receives blood from the left atrium. valve between the left atrium and left ventricle. passage of solvent (fluid) through semipermeable membrane that separates different concentrations of solutions. Movement is from an area where there is a lower concentration of solute into an area where there is an area of higher concentration of solute to equalize the concentration of the two solutions. serum, proteins, and chemical substances found in the aqueous portion of blood. circulation of blood through the lungs for exchange of oxygen and carbon dioxide. valve between the right ventricle and the pulmonary artery. right upper chamber of the heart; receives blood returning to the heart from the inferior and superior vena cava. right lower chamber of the heart; receives blood from the right atrium. substance dissolved in a solution. solution holding the solute. large vein that collects blood from parts of the body above (superior to) the heart for its return to the right atrium. total parenteral nutrition (TPN) nutritional support via central access IV therapy to provide glucose, proteins, vitamins, electrolytes, sometimes fats, and so on to maintain the body’s growth, development, and tissue repair. valve between the right atrium and right ventricle. vessels that return blood toward the heart. puncture of a vein for any purpose; related to IV therapy, puncture of the vein to place an administration device for infusion of IV fluids. very small veins that carry blood from the capillaries to the veins. Refer to Figures 2-1 and 2-2 for primary routes of the circulation system. The chamber of the heart first receiving carbon dioxide (CO2)-laden blood from the superior and inferior vena cava is the right atrium. The blood, moving primarily by gravity as the valves open, travels through the tricuspid valve into the right ventricle. The walls of the atria are thinner than the walls of the ventricles because they do not have to pump the blood into the next area against gravity and to more distant areas of the body as the ventricles do. The right ventricle pumps blood through the pulmonary (semilunar) valve into the pulmonary artery and then into the lungs, or through pulmonary circulation. The blood travels through pulmonary circulation where gases CO2 and oxygen (O2) are exchanged at the cellular level of the alveoli of the lungs. The oxygen-laden blood leaves the pulmonary circulation via the pulmonary veins to return to the heart into the left atrium. The blood then passes through the mitral or bicuspid valve into the left ventricle. Here, the forceful contraction of the cardiac muscle accelerates the blood through the aortic valve into the aorta and into the cardiac and general body or systemic circulation. The oxygenated blood travels through the systemic circulation to the body via the aorta, which branches to form arteries to the myocardium (or coronary circulation through coronary arteries), brain (through the carotid and cerebral arteries), upper limbs (through brachiocephalic and subclavian arteries), and trunk and lower limbs (via thoracic aorta and femoral arteries) (Figure 2-3 and color insert). As the aorta descends into the body, it divides into arteries to supply circulation to the major organ systems and to the peripheral regions of the body. As the arteries branch out, they gradually become smaller and are termed arterioles. At the terminal branches of the arterioles, capillaries with permeable membranes are formed to allow transfer of nutrients and oxygen into the tissues and absorption of CO2 and metabolic waste products for return to the heart. The distal end of capillaries become very small veins, called venules, and as they progress back to the heart, they turn into progressively larger veins (Figure 2-4 and color insert). The veins terminate in the superior and inferior vena cava to complete the circulatory circuit as they empty deoxygenated blood into the right atrium of the heart. Fluid containing solutes leaves the capillaries to surround tissue cells as extracellular fluid.
Review of Anatomy and Physiology
CIRCULATORY SYSTEM
Route of Blood Flow
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine