Revascularization and Replantation of the Digits
L. Scott Levin
DEFINITION
Replantation is the reattachment of a completely amputated body part.
Revascularization is the restoration of circulation and repair of all injured structures in an incompletely amputated, dysvascular body part. Revascularization always includes repair of blood vessels to reestablish blood flow to the part.
Revision amputation is the procedure performed at the site of amputation to gain soft tissue coverage and to address concomitant injuries to the digit.
The decision of whether to perform replantation or revascularization and revision amputation of a digit is multifactorial. The relative indications and contraindications for each are discussed later in the chapter.
ANATOMY
An understanding of the anatomy over the complete length of the digit is essential for successful replantation. The anatomy of the thumb is different from that of the four fingers.
Palmar and dorsal cutaneous ligaments maintain the position of the neurovascular bundle during range of motion of the digit.
Grayson ligament is palmar to the neurovascular bundle, originates from the flexor tendon sheath, and inserts on the skin.
Cleland ligament travels dorsal to the neurovascular bundle from the phalanx to the overlying skin.
A radial and ulnar proper digital artery supplies each digit. Each vessel travels with a respective radial and ulnar proper digital nerve. At the level of the digit, the artery lies dorsal to the nerve.
The ulnar digital artery is typically larger in the thumb and index fingers. The radial digital artery usually is larger in the small finger.
Three major palmar arches arise from the digital arteries. The proximal, middle, and distal arches are consistently located at the level of the C1 pulley, C3 pulley, and just distal to the flexor digitorum profundus (FDP) insertion, respectively.
Four palmar and four dorsal branches usually extend from each digital artery.
Injection studies have demonstrated that the venous system of the digit consists of a series of arcades on the dorsal and palmar surfaces, with connecting oblique and transverse anastomotic veins.10 The dorsal veins have a larger caliber than the palmar veins, which do not consistently travel with the digital artery and nerve.
A radial and ulnar proper digital nerve travels with each proper digital artery. The digital nerve is sensory only and typically contains one to three fascicles. It trifurcates at the level of the distal interphalangeal (DIP) joint.
Each finger has two flexor tendons within the flexor tendon sheath.
The FDP tendon inserts at the proximal base of the distal phalanx.
The flexor digitorum superficialis (FDS) tendon inserts as two slips into the midportion of the middle phalanx. The FDS tendon splits into two slips, and its relative position to the FDP tendon switches from palmar to dorsal at Camper chiasm. This allows the deeper FDP tendon to continue to its more distal insertion.
There are a series of five annular and three cruciform pulleys, which are discrete thickenings of the fibro-osseous sheath. The annular pulleys prevent bowstringing of the flexor tendons during flexion, whereas the cruciate pulleys are collapsible, accommodating flexion.
The odd-numbered annular pulleys are located over the joints of the finger, and the even-numbered annular pulleys are over the proximal and middle phalanx, respectively.
The A2 and A4 pulleys are most important in preventing bowstringing and should be preserved if possible.
Each lesser digit receives a tendon from the extensor digitorum communis (EDC). The index and small fingers each have a second extensor tendon, the extensor indicis proprius (EIP) and extensor digiti minimi (EDM), respectively. Both of these tendons are ulnar to the EDC tendons.
PATHOGENESIS
The mechanism of injury has a considerable effect on the potential for replantation.
Sharp amputations are ideal for replantation because of the narrow zone of injury.
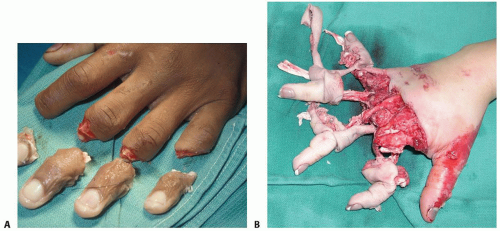
The degree of tissue injury increases substantially with crush and avulsion mechanisms and may prohibit successful replantation (FIG 1).
Most digit amputations occur as an isolated injury. When amputations occur in the multiply injured patient, consideration of other systemic injuries and adherence to advanced trauma life support (ATLS) protocols may prevent replantation.
NATURAL HISTORY
Replantation of an amputated digit results in longer hospital stays and more prolonged rehabilitation than revision amputation. Patient satisfaction, however, usually is higher with replantation than with revision amputation or a prosthesis.8,11,12
Functionally, the expected range of motion in a replanted digit is 50% of normal.
Secondary procedures, such as tenolysis, are common.
The literature reports rates of reoperation ranging from 3% to 93%. In a series of more than 1000 replants and
revascularizations, 35% of patients required at least one secondary surgery.18 The incidence is higher for replantations than for revascularizations.
Expected survival rates of replanted digits are 80% or higher, with even higher survival rates in revascularized digits.
PATIENT HISTORY AND PHYSICAL FINDINGS
The surgeon must evaluate the patient in the emergency room immediately on arrival. A complete history and physical examination are performed.
The history should include specific details regarding the mechanism and timing of the injury. Identification of the specific machinery involved often reveals valuable information about potential contamination and the pattern of injury sustained by the amputated part.
A history of mental instability is relevant because rehabilitation protocols require significant patient compliance to maximize functional outcomes. Furthermore, self-inflicted amputations are unlikely to yield the same functional results after replantation as accidental amputations.
A history of medical comorbidities should be thoroughly evaluated. Conditions such as diabetes, peripheral vascular disease, hypercoaguability, and tobacco use are not absolute contraindications to replantation but must be considered.
Similarly, the surgeon must evaluate for medical conditions that prevent the patient from tolerating the blood volume changes associated with major limb replantation. Revision amputation may be the best choice if the patient has a history of previous trauma or arthritis in the amputated part.
Ischemia time and method of transport should be evaluated for appropriateness. In the digits, a warm ischemia time of less than 6 hours is desired. In more proximal amputations containing muscle, ischemia time is more critical.
Cooling the amputated part reduces metabolic acidosis, bacterial growth, and muscle necrosis. Cold ischemia times of up to 12 hours are tolerated for replantation of digits. There are reports of successful replantation of digits with warm ischemia times of 42 hours and cold ischemia times of 96 hours.2,19
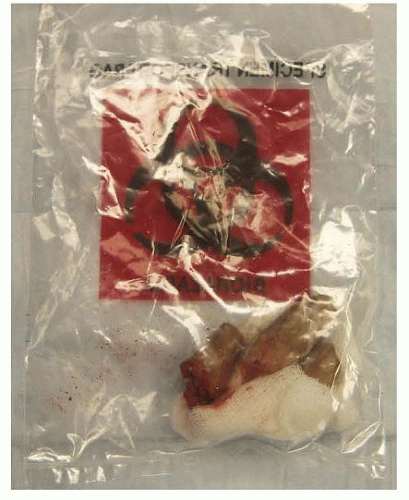
Proper transportation of the amputated part is essential. Never place the part directly on ice. The part should be wrapped in a sterile gauze moistened with Ringer lactate or normal saline. The gauze is then placed in a leakproof plastic bag and the bag is placed on ice (FIG 2). The temperature should be maintained at approximately 4° C.
Alternatively, the part may be immersed in Ringer lactate or normal saline in a plastic bag with the bag then placed on ice.
The surgeon examines the part and the injured extremity to evaluate suitability for replantation. The number of digits, level of injury, and type of injury are assessed.
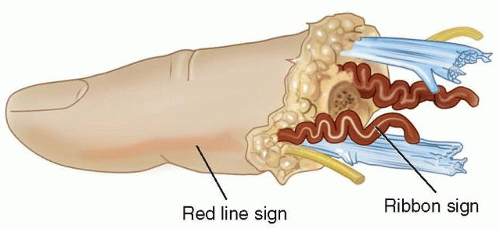
Specifically, the surgeon evaluates the injured parts for the red line sign and the ribbon sign.
The red line sign refers to a red streak of ecchymosis along the lateral border of the digit, which is the result of hemorrhage from avulsed branches of the digital artery after a traction injury (FIG 3).
IMAGING AND OTHER DIAGNOSTIC STUDIES
When the patient arrives in the emergency department, standard radiographs of the amputated parts and the injured limb are obtained (FIG 4).
Laboratory evaluations should include a complete blood count, basic metabolic panel, coagulation panel, drug screen, and blood type and crossmatch. Other preoperative tests are ordered as indicated by the patient’s age and comorbidities.
NONOPERATIVE MANAGEMENT
There is no role for nonoperative management of these injuries.
Some surgeons advocate performing revision amputations in the emergency department under local anesthesia. It has been our experience that these procedures are best performed in the operating room with appropriate anesthesia, hemostasis, sterile conditions, lighting, and equipment.
SURGICAL MANAGEMENT
The decision to replant a digit is predicated on the determination that the anticipated function after replantation will be better than that of a revision amputation. This determination is made after careful consideration of the factors influencing the predicted survival of the replanted digit, morbidity to the patient, and functional outcome.
Specific factors related to the status of the amputated part and the status of the patient include the following:
Mechanism of injury (eg, sharp, crush, avulsion)
Level of amputation
Ischemia time (warm or cold)
Health of patient
Age of patient
Presence of segmental injury
Predicted rehabilitation
Vocation and hobbies
Informed consent for replantation versus revision amputation must reference the postoperative care differences.
Patients undergoing revision amputation typically are discharged from the hospital much quicker and have much shorter, less intensive rehabilitation protocols.
Patients treated by replantation typically require a 5- to 7-day hospital course, avoidance of smoking and caffeine, possible blood transfusions, and prolonged rehabilitation. Furthermore, these patients must be advised about the likelihood of cold intolerance.
The techniques we use for replantation of amputated digits are described in detail in the following sections. The same techniques and sequence of repair are followed for the revascularization of partially amputated parts.
In partial amputations, not all structures will be injured, so it may be that only some structures require repair. For example, if the dorsal skin and its veins remain intact, the procedure does not require venous anastomosis for outflow.
Each case should be examined individually, and all structures should be carefully evaluated for injury.
Preoperative Planning
Broad-spectrum antibiotics and tetanus prophylaxis are administered on presentation in the emergency department.
The patient, hand, and amputated parts are examined to confirm suitability for possible replantation.
A urethral catheter should be placed for long procedures.
Regional anesthesia is preferred to facilitate autonomic blockade, which results in increased peripheral vasodilation. Ideally, an indwelling catheter is placed to allow for continuous postoperative pain relief and sympathetic block. General anesthesia is required for children.
If an attempt at replantation is determined to be appropriate and desired, the parts are brought to the operating room as soon as possible. Initial preparation of the parts can begin while the anesthesia team evaluates the patient.
The operating room and patient must be kept warm to prevent peripheral vasoconstriction.
The sequence of repair is as follows:
Positioning
The patient is positioned supine on a standard operating room table with a hand table attachment. The table is rotated 90 degrees to allow access for the operating microscope and fluoroscopy.
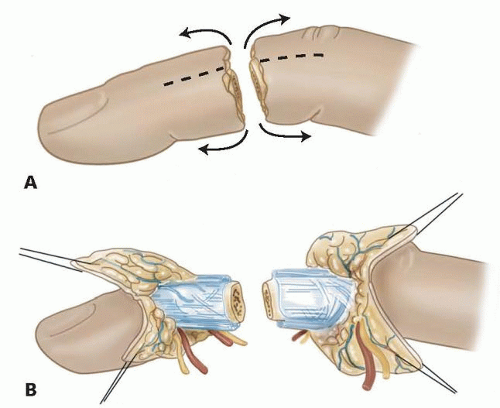
Approach
Slightly dorsal midaxial incisions are made on both the radial and ulnar sides of the digits. These incisions allow for rapid identification of both the neurovascular bundles and the dorsal veins. Both the palmar and dorsal flaps can be reflected as needed (FIG 5).