Retrocalcaneal Bursoscopy (Endoscopic Removal of Bone, Bursa, and Paratenon)
Angus M. McBryde
Fred W. Ortmann
DEFINITION AND INTRODUCTION
Patrick Haglund in 1928 described an enlarged posterior border of the os calcis.4
This anatomy (Haglund deformity) becomes very important when external shoeing/heel counter and repeated hyperdorsiflexion causes contact between the Achilles tendon, the posterior vertical surface of the calcaneus, and the interposed retrocalcaneal bursa.
As a result, Haglund syndrome is commonly characterized by inflammation within the retrocalcaneal or Achilles tendon bursa and often secondarily presents as insertional Achilles tendinopathy.
The posterior heel pain and swelling associated with Haglund syndrome is the result of mechanical irritation by the calcaneal prominence on the surrounding soft tissues and the anterior paratenon of the Achilles tendon.
After conservative/nonoperative measures have failed and imaging does not show significance, Achilles tendinopathy,
Haglund deformity, and retrocalcaneal bursitis can be treated surgically using an endoscopic technique. General indications are pain, limp, alteration of workstyle or lifestyle, and, lastly, significant night pain.
The endoscopic technique is an outpatient treatment that is associated with low morbidity and high outpatient satisfaction. There is a short recovery time and a short time to gain prior activity level.
Appropriate visualization of the Achilles tendon and its paratenon and removal of the calcaneal prominence and retrocalcaneal bursa can be effectively accomplished using an endoscopic technique.
PATHOGENESIS
The retrocalcaneal space has been described as a disc space bursa covering the posterior superior angle of the calcaneus.3 The bursa walls may become diseased and hypertrophied with repeated hindfoot movement. Increased pressure can occur and become chronic with secondary calcaneal bone edema and paratenon reactive fibrosis at the insertion.
Achilles tendinopathy is a degenerative process within the tendon substance causing microtears which can progress to macrotears, edema, and reactive fibrosis with scar formation. These changes can cause secondary mechanical irritation of the surrounding tissues and can even stimulate an inflammatory process.9
PATIENT HISTORY AND PHYSICAL FINDINGS
Clinical evaluation may help differentiate between retrocalcaneal bursitis and Achilles tendinopathy, although the two often coexist.
Pathology within the retrocalcaneal space is detected on clinical examination with point tenderness along the anteromedial and anterolateral aspects of the Achilles tendon and an associated prominence of the calcaneus.
Palpation of the affected hindfoot often reveals tenderness at the distal portion of the Achilles tendon proximal to its insertion on the calcaneus. The pain can be reproduced with passive or active dorsiflexion. The retrocalcaneal bursa and the more directly posterior Achilles tendon bursa can become confluent and “wrap around.”
IMAGING AND OTHER DIAGNOSTIC STUDIES
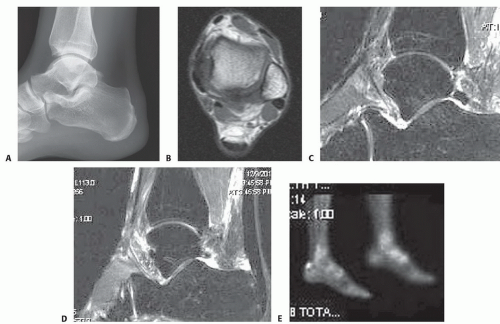
Imaging can assist with documenting the presence or absence of tendinopathy (FIG 1A).
It can be difficult to distinguish whether symptoms are caused by retrocalcaneal bursitis or insertional Achilles tendinosis or tendinitis. These two conditions often coexist.
Magnetic resonance imaging (MRI) should be used preoperatively to better demonstrate or differentiate coexistence of these diagnoses (FIG 1B-D).
Normal-appearing and diseased tendons can usually be distinguished endoscopically.
Ultrasound can help rule out a distal Achilles noninsertional tendinopathy or tendinitis.
Limited bone scan can help with differential diagnosis with its sensitivity (FIG 1E).
NONOPERATIVE MANAGEMENT
Nonoperative measures for the treatment of posterior heel pain include the use of nonsteroidal anti-inflammatory medication, shoe wear modification (such as using backless shoes and avoiding irregular counters), physical therapy for icing or other modalities, stretching exercises, pressure-release inserts, and hands-on friction massage.
Local injections can be given in the retrocalcaneal space for diagnostic purposes. The concomitant use of local anesthesia and corticosteroids can further weaken the substance of the Achilles tendon and risk weakness and further micro- or macrorupture of the tendon.5
SURGICAL MANAGEMENT
The goal of treatment for Haglund deformity and associated inflammation and tendinopathy is to remove the calcaneal prominence and to decompress the inflamed surrounding soft tissues.
Open surgical correction is an alternative for patients who have failed to respond to nonoperative measures and if there is an estimated tendinopathy with ˜25% involvement on axial
Achilles serial images. In that case, augmentation (authors preference) or alternate open Achilles tendon surgery is advisable.
Open procedures generally include the following:
Resection of the calcaneal prominence (Haglund deformity) proximal to the Achilles tendon insertion
Retrocalcaneal bursa removal
Rarely, a dorsal closing wedge osteotomy can rotate the posterior calcaneus to a lesser prominent position.
Achilles tenolysis and partial resection of the diseased portion of the tendon may be necessary, often with augmentation by the flexor hallucis longus or flexor digitorum.
Complete Achilles removal at its insertion with multianchor reinsertion is occasionally necessary.
Complications associated with these procedures can include hematomas, tendon or skin breakdown, nonunion, Achilles tendon avulsion, tenderness around the operative scar, cosmetic problems, altered sensation around the heel, and stiffness.1,7,11,13,14 Rehabilitation following open surgery can be prolonged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree