CHAPTER 16 Results and Complications
The results of unconstrained shoulder arthroplasty have been reported by multiple investigators. The results vary predominantly according to the underlying indication for which the arthroplasty has been performed. To our knowledge, the largest reported database of results of unconstrained shoulder arthroplasty was presented in Nice, France, in 2001.1 Because of the large number of patients enrolled, this multicenter study has allowed meaningful conclusions to be made about the outcomes and complications of unconstrained shoulder arthroplasty. Our results have largely mirrored those reported in the Nice study. This chapter reports the results of unconstrained shoulder arthroplasty for the treatment of nonfracture conditions by drawing from information in the Nice database and our arthroplasty database that was prospectively established in 2003. Additionally, the most frequent complications and their treatment are outlined.
RESULTS
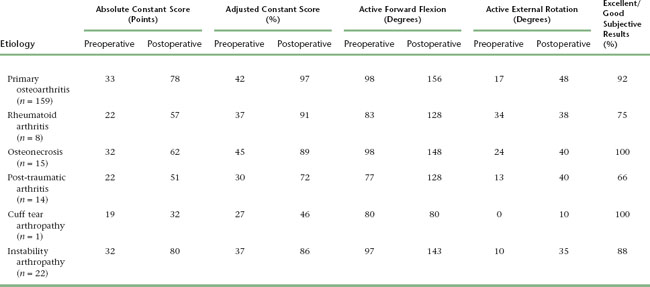
The results of unconstrained shoulder arthroplasty vary mainly with the cause for which the arthroplasty is performed. The best results are obtained in the treatment of primary osteoarthritis and osteonecrosis, whereas results are least satisfactory for post-traumatic arthritis and rotator cuff tear arthropathy. Tables 16-1 and 16-2 detail the results of unconstrained shoulder arthroplasty for the most common indications for which it is performed.2–8 These tables express the results in terms of active mobility; patient satisfaction; the Constant score, a shoulder-specific outcomes device incorporating pain, mobility, activity, and strength; and the age- and gender-adjusted Constant score.9,10
Table 16-1 RESULTS OF UNCONSTRAINED SHOULDER ARTHROPLASTY ACCORDING TO UNDERLYING CAUSE IN THE NICE MULTICENTER STUDY
| Rights were not granted to include this data in electronic media. Please refer to the printed book. |
INTRAOPERATIVE COMPLICATIONS
Humerus
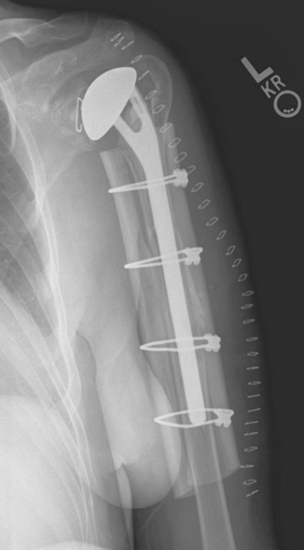
Intraoperative complications involving the humerus are rare. The most common humeral complication is iatrogenic fracture, which usually results from performing an overly aggressive dislocation maneuver without previous adequate soft tissue release. Patients with osteopenia (i.e., inflammatory arthropathy patients) and those with severe preoperative stiffness (i.e., post-traumatic arthritis) are at most risk for this complication. These fractures may occur at the humeral diaphysis or proximally and involve the tuberosities. Fractures involving the humeral diaphysis should be reduced and a long-stem humeral implant placed. Allograft struts and cerclage cables may be added in patients with severe osteopenia (Fig. 16-1).
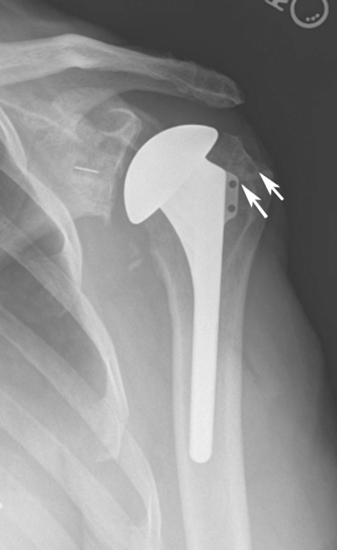
Intraoperative fractures involving the greater or lesser tuberosities (or both) are usually nondisplaced. Many of these fractures are stable or become stable once the humeral implant is placed (Fig. 16-2). If a tuberosity fracture is not satisfactorily stable, suture fixation of the tuberosity is performed and the postoperative rehabilitation adjusted accordingly to allow healing of the tuberosity.
Glenoid
Fractures that involve only a small portion of the peripheral rim usually require no treatment, and the glenoid component can be inserted as planned. Glenoid fractures that extend into the central portion of the glenoid (keel slot or peg holes) should be bone-grafted with the humeral head, and placement of a glenoid component should be avoided. Placement of a glenoid component in a patient with a fracture involving the central portion of the glenoid can result in early glenoid failure (Fig. 16-3).
Rotator Cuff
With proper glenoid exposure, intraoperative injury to the rotator cuff is rare. The key to avoiding rotator cuff injury during unconstrained shoulder arthroplasty is adequate visualization of the rotator cuff before resection of the humeral head (see Chapter 11). If the rotator cuff is adequately visualized, inadvertent damage to the rotator cuff by the saw during humeral head resection can be avoided.
POSTOPERATIVE COMPLICATIONS
Postoperative complications are more common than intraoperative complications and occur in up to 20% of cases of unconstrained shoulder arthroplasty.1 The most common postoperative complications include wound problems (dehiscence, hematoma), glenoid problems, humeral problems, instability, rotator cuff problems, stiffness, and infection.
Wound Problems
Wound problems occur early after unconstrained shoulder arthroplasty. Hematoma is most easily avoided by extensive use of electrocautery during shoulder arthroplasty. Suture ligation, in addition to electrosurgical cauterization, of the anterior humeral circumflex vessels also minimizes the incidence of postoperative wound hematoma. When a hematoma occurs, it is managed by symptomatic nonoperative treatment (warm compresses, pain medication). Operative drainage is reserved for situations in which drainage persists beyond 1 week or infection is suspected (see later) but is rarely necessary.
Wound dehiscence occurs occasionally when susceptible patients have a reaction to dissolving subcutaneous sutures. The presence of minimal serous drainage distinguishes this complication from the more serious deep infection. Superficial wound dehiscence is treated by local wound care, including removal of any residual dissolving suture material and chemical cauterization of any granulating tissue with silver nitrate applicators (Fig. 16-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree