CHAPTER 23 Results and Complications
The results of unconstrained shoulder arthroplasty for fracture have been reported by multiple investigators. The overall results have been very disappointing and are not comparable to those obtained for chronic conditions such as primary osteoarthritis. The advances in unconstrained arthroplasty implants and techniques for fracture described in this section have greatly improved the results. To our knowledge, the largest reported database of results of unconstrained shoulder arthroplasty for fracture was presented in Nice, France, in 2001.1 Because of the large number of patients enrolled, this multicenter study has allowed meaningful conclusions to be made about the outcomes and complications of unconstrained shoulder arthroplasty for the treatment of fracture. Our results have largely mirrored those reported in the Nice study. This chapter reports the results of unconstrained shoulder arthroplasty for the treatment of proximal humerus fractures by drawing from information in the Nice database and our arthroplasty database that was prospectively established in 2003. Additionally, the most frequent complications and their treatment are outlined.
RESULTS
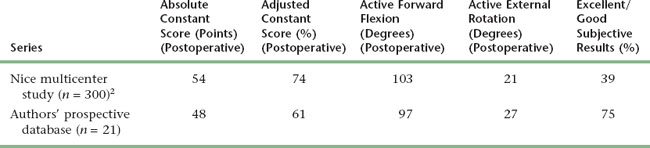
The results of unconstrained shoulder arthroplasty for fracture are largely related to two prognostic factors: age and the presence of tuberosity complications (nonunion, malunion). These two factors are related in that older patients are more likely to have osteopenia of the tuberosities and hence complications with tuberosity healing. Although age-related osteopenia is beyond the surgeon’s control, advances in prosthetic design and tuberosity fixation techniques continue to decrease the rate of tuberosity-related complications. Table 23-1 details the results of unconstrained shoulder arthroplasty in the treatment of proximal humeral fracture.2 This table expresses the results in terms of active mobility; patient satisfaction; the Constant score, a shoulder-specific outcomes device incorporating pain, mobility, activity, and strength; and the age- and gender-adjusted Constant score.3,4
INTRAOPERATIVE COMPLICATIONS
Neurovascular Structures
Catastrophic injury to neurovascular structures around the shoulder, though rare, are more common during performance of shoulder arthroplasty for fracture than for performance of shoulder arthroplasty for nonfracture indications. Many patients with proximal humeral fractures suffer neuropraxic injury to the axillary nerve, and this should be documented on clinical examination before surgery. Additionally, the implications of axillary nerve injury secondary to fracture should be discussed with the patient extensively before surgery. Treatment of axillary nerve injury is observation, with less than 2% of patients sustaining a permanent axillary nerve deficit.5
Vascular injuries during unconstrained shoulder arthroplasty performed for fracture most often involve injury to the axillary artery. Such injury is usually a consequence of overzealous medial dissection or retraction (or both), combined with vasculature that has been compromised by aging (plaques, calcification). Should one of these injuries occur after cross-clamping of the injured structure, emergency intraoperative consultation with a vascular surgeon is required.
Humeral Shaft Fracture
Intraoperative humeral shaft fractures are very rare when performing unconstrained shoulder arthroplasty for the treatment of proximal humeral fractures. Stiffness is rarely a problem in these cases, thus minimizing the torsional stress placed on the humeral shaft during manipulation of the arm. More commonly, humeral injury occurs during reaming of the humeral shaft. The diaphyseal cortex in many elderly patients is very thin and hence has an increased risk of diaphyseal penetration. When this complication occurs, it is often unrecognized (Fig. 23-1).
POSTOPERATIVE COMPLICATIONS
Postoperative complications are much more common than intraoperative complications and occur in more than 50% of cases of unconstrained shoulder arthroplasty performed for fracture.5 Most complications involve the greater or lesser tuberosities (or both) but also may include wound problems (dehiscence, hematoma), glenoid problems, humeral problems, instability, stiffness, and infection.
Tuberosity Complications
Nonunion and malunion of the greater and lesser tuberosities are the most common complications after unconstrained shoulder arthroplasty in fracture cases (Fig. 23-2). The occurrence of a tuberosity complication compromises the outcome significantly in most cases. The best way to handle tuberosity complications is to avoid them by using the techniques described in this section. When tuberosity complications do occur, there is no simple solution that provides a reliable result. Even early recognition and reattachment of a migrated tuberosity yields unsatisfactory results in nearly all cases. Similarly, tuberosity osteotomy produces poor results in cases of malunion. The most predictable results are obtained with revision arthroplasty to a reverse prosthesis in these cases (Fig. 23-3; see Section Six).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree