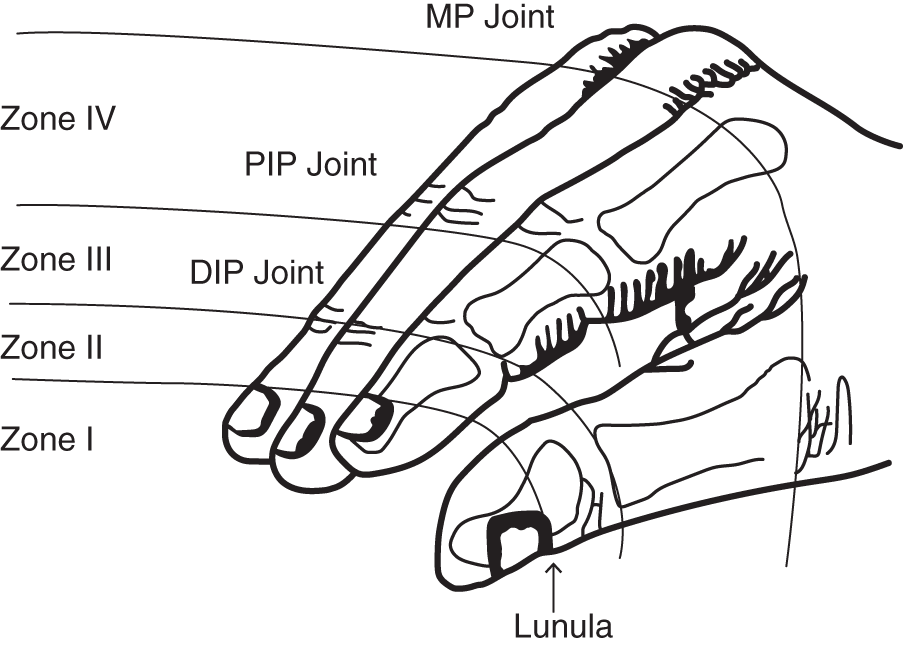
Serge Goekjian MD FRCS (C)1, Lucas Gallo BHSc MD (c)2, and Achilleas Thoma MD MSc3 1 Division of Plastic Surgery, University of Toronto, ON, Canada 2 Michael G. DeGroote School of Medicine, McMaster University, Hamilton, ON, Canada 3 Division of Plastic Surgery, Department of Surgery, McMaster University, Hamilton, ON, Canada Figure 164.1Tamai classification of zones in digital amputation: zone I (distal to lunula), zone II (proximal to lunula, distal to DIP joint), zone III (proximal to DIP joint, distal to insertion of FDS tendon), and zone IV (proximal to FDS tendon insertion, distal to MP joint). DIP, distal interphalangeal; PIP, proximal interphalangeal; MP, metacarpophalangeal. Source: Lee et al.4 In 1978, Tamai et al. reported that two veins should be anastomosed for each artery repaired during digital replantation.1 In contemporary practice, there exists little consensus among microsurgeons regarding the optimal number of veins that must be repaired when performing digital replantation surgery (Table 164.1).2 Though bone, tendon, and nerve repair correlates with long‐term functional outcomes, venous outflow remains the most important factor influencing replantation success in the immediate postoperative period.2,3 While a surgeon may not have a choice on the matter if only one or multiple veins are not present, the question is: what if multiple veins exist? How many should one repair per digit? While it is considered to be favorable to anastomose as many veins as possible, a balance must be achieved between ischemia time, survival rate, and overall operation time.4 At present, the highest‐quality evidence for venous anastomosis in the setting of digital replantation consists of retrospective cohort trials. Seven retrospective cohort studies were identified consisting of 1317 replanted digits (level III evidence).24–9 A retrospective cohort study by Ryu et al. assessed the relationship between the number of venous anastomoses and replantation survival in 143 cases.5 No significant correlation was identified between the number of veins anastomosed and replantation survival (p = 0.689). Efanov et al. reviewed 101 digital replantations and concluded that single vein repair corresponded to an increase in replantation failure when compared to two vein anastomoses (p = 0.032; risk ratio [RR] = 1.27; 95% confidence interval [CI]: 0.991–1.343).2 A significant increase in replantation failure was also demonstrated in cases of no vein repair versus two vein anastomoses (p = 0.008; RR, 1.49; 95% CI: 1.026–1.735). However, no significant difference was identified between one vein versus no vein anastomosis (p = 0.502; RR = 1.179; 95% CI: 0.834–2.102]. Huang and Yeong (n = 31) as well as Neto et al. (n = 50) failed to reach statistical significance when comparing one vein versus no vein anastomosis (p >0.05) and one vein versus multiple vein anastomosis (p = 0.105), respectively.6,7 Lee et al. and Matsuda et al. (n = 847 total digital replantations) provided recommendations for optimal venous anastomosis at each Tamai amputation zone (Figure 164.1).4,8
164 Replantation
Clinical scenario
Top three questions
Question 1: In patients requiring replantation, how many veins should be anastomosed when performing digital replantation to achieve optimal outcomes?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Zone 1
Zone 2
Zone 3
Zone 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





