Repair of Distal Biceps Tendon Rupture
Bernard F. Morrey
INTRODUCTION
Once thought to be an uncommon injury, the avulsion of the distal biceps tendon from the radial tuberosity is being seen in increasing numbers in those involved with heavy use of the extremities as well as in recreational and competitive athletes. In general, it is of interest that the injury occurs almost exclusively in males, usually those with heavy lifting requirements of work or avocation.
PATHOLOGY
The distal biceps tendon complex may be injured at the musculotendinous junction, by a disruption of the tendon itself “in continuity” or a complete or partial tear or avulsion of the tendon from the radial tuberosity (Fig. 21-1). By far, the most common lesion is the avulsion from the tuberosity, and this is the only lesion that is dealt with in this chapter. Reliable management of the other injuries to the flexor system is less clear.
Of the tears from the radial tuberosity, approximately 95% are complete ruptures whereas about 5% are partial tears. Both conditions along with delayed reconstruction are addressed in this chapter.
DIAGNOSIS
Complete rupture is easy to diagnose in most instances due to retraction of the distal biceps muscle belly with elbow flexion. Partial tears also occur almost exclusively at the tuberosity. However, as with a strained ligament, the biceps does not retract. Unlike a strain, partial tears do not heal. The history is commonly that of eccentric loading during a single flexion event. Hematoma formation is variable, as is the location of the pain (Fig. 21-2).
Imaging
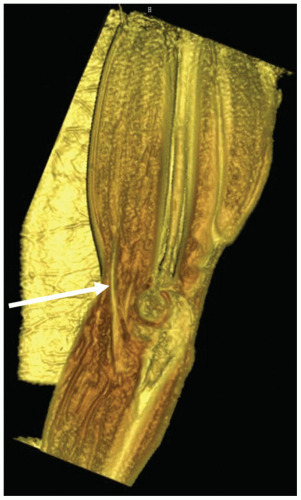
In recent years, there has been a significant improvement in the ability to diagnose the biceps tendon injury, especially incomplete rupture, with MRI. By placing the arm overhead, the course of the biceps tendon may be brought in plane, thus allowing a more accurate assessment of the pathology. This position was described by Giuffre and Moss and is termed the flexion abduction supination, “FABS,” view (Fig. 21-3) (1). In addition three-dimensional reconstructions are also improving our preoperative understanding of the precise location and extent of the pathology present. This is of particular value in instances of partial rupture or other less common injuries (Fig. 21-4).
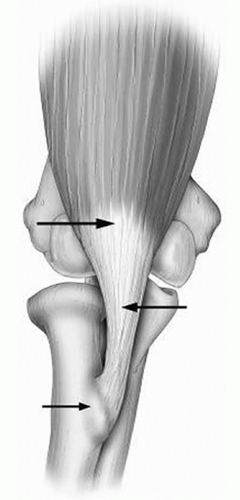 FIGURE 21-1 The biceps mechanism may be injured at the muscle/tendinous junction, at the intratendinous, or at the tuberosity. |
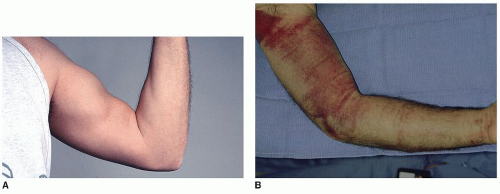 FIGURE 21-2 In most instances, proximal retraction is diagnostic (A). Ecchymosis is uncommon. In this instance, this competitive athlete had been on high-dose aspirin at the time of injury (B). |
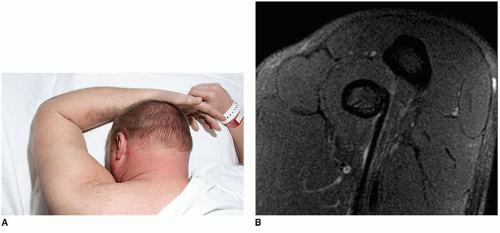 FIGURE 21-3 The flexion abduction supination (FABS) view (A) brings the entire tendon and its attachment into profile with MRI (B). |
INDICATIONS/CONTRAINDICATIONS
Indications
Although some have demonstrated reasonable function without fixing the tendon (2), in my judgment, there is little question that in the active patient, distal biceps tendon rupture should be repaired as soon as possible (3,4,5,6 and 7). There have been several studies including our own (8) attempting to estimate and evaluate both subjective and objective dysfunction following the nonrepaired biceps tendon. These assessments have generally shown reasonable function under most circumstances with minimal pain with repair. However, with excessive exertion, the patients do have pain and lack endurance; hence the need for reconstruction in some patients if the repair is not performed acutely (8). The average age of patients with the injury is approximately 55, and virtually every report has documented the almost exclusive occurrence in the male. In our practice at Mayo, we have treated only two females from among over 200 with this diagnosis, both with partial ruptures. Usually, the patient is involved with heavy labor or athletic activity, which further emphasizes the need of early definitive treatment.
Delayed reattachment is difficult because the tendon retracts. If this has occurred, reattachment or embedding the biceps tendon into the brachialis is easy but not considered acceptable today. We have recently documented effective delayed repair requiring elbow flexion from 60 to 100 degrees (9). However, without question, immediate repair is the treatment of choice. Reconstruction for the selected patients has been effective in recent years, but this is a difficult surgical procedure (10) and typically is referred to those surgeons with experience with this procedure. The author prefers the Achilles allograft for this procedure (see Chapter 22).
Contraindications
Reattachment is contraindicated in patients who do not have significant functional impairment. This is not very applicable in the athlete or laborer but might be considered in a sedentary patient—but rarely does such an individual sustain this injury. Attempts to reattach this tendon if there has been a delay of over 3 weeks require careful thought as the tendon often is retracted into the biceps muscle and the tendon track is scarred. If the delay is prolonged, there may not be adequate length to reach to the radial tuberosity even with elbow flexion and a reconstructive procedure could be required (see Chapter 22) (6). Furthermore, the tract of the tendon to the tuberosity will have scarred and become obliterated, making the surgery much more difficult with a higher complication rate (11). However, if the tendon does reach the tuberosity with up to 90 degrees of elbow flexion, reattachment is an effective and reliable procedure (9).
SURGICAL CONSIDERATIONS
Technical options continue to emerge. The surgeon has two interrelated technical considerations to consider when addressing these patients. The first is the selection of either a one- or two-incision technique. The second is the mode of fixation. In this chapter, we deal with three types of fixation, which with their variations reflect virtually all of the approaches used today: bone tunnel, suture anchor, and Endobutton.
The surgical approach is clearly the preference of the surgeon. Surgical procedures have been described using a modified Henry approach (12,13) or through a two-incision approach described by Boyd and Anderson (14) and modified at Mayo (6). The theoretic advantage of the anterior Henry approach is that it is felt to be less likely to create ectopic bone. The disadvantage is that it puts the radial nerve at jeopardy (8,12,13) and is difficult to identify and replicate the “footprint” of the tendon attachment. Regarding the two-incision approach, it must be emphasized what is currently recommended is NOT that described by Boyd and Anderson. The Mayo modification is a muscle-splitting approach that does not expose the ulna. The advantage of the two-incision technique is that it lessens and virtually eliminates the likelihood of injury to the radial nerve (15). The original Boyd-Anderson approach exposes the ulna and hence can be associated with ectopic bone (16). Through the years, we have employed the Mayo modification of the Boyd-Anderson approach, which does NOT expose the ulna and hence is associated with very little ectopic bone (11). I have not experienced a single instance of cross bridging in my experience to date.
The author continues to use the two-incision technique with excellent results and minimal complications (17). It is recognized that the one-incision technique is also popular with the thought that it possibly lessens the likelihood of ectopic bone formation. This has not been demonstrated to be the case, but it does motivate many to use a single anterior approach. The direct exposure is correlated with the mode of fixation. An anterior approach can be used for the Endobutton or the suture anchor. For bone tunnels, a two-incision technique is required.
PREOPERATIVE PLANNING
If the injury is more than 4 weeks since onset, be prepared to perform a more detailed dissection in the antecubital space. If the tendon has retracted, direct reattachment to the tuberosity with the elbow flexed up to 90 degrees is preferred. If this isn’t possible, restoration of length with an Achilles tendon allograft is performed. The patient must be prepared for these eventualities.
TECHNIQUE
Complete Rupture: Immediate Reattachment
Incision The arm is prepped and draped with the patient supine. A sandbag may be placed under the shoulder to allow the arm to comfortably be brought across the chest. Under a general anesthesia, a single 4-cm transverse incision in the antecubital crease is employed (Fig. 21-5).
Tendon Preparation By digital palpation or limited dissection, the tendon is identified, dissected free of soft tissue, and delivered from the wound (Fig. 21-6). The end of the tendon tends to be bulbous and is trimmed in order to allow it to fit well into the tuberosity. After the tendon has been trimmed, two No. 5 Mersilene sutures are placed through the torn portion entering the end of the tendon. A crisscrossed (Bunnell) suture or locking stitch (Krackow) is employed (Fig. 21-7).
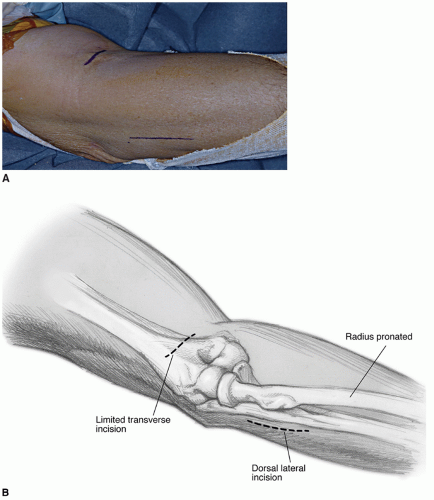 FIGURE 21-5 The two-incision technique employs a simple 4-cm transverse incision in the antecubital space (A) and a 5- to 7-cm incision over the posterior aspect of the proximal forearm (B). |
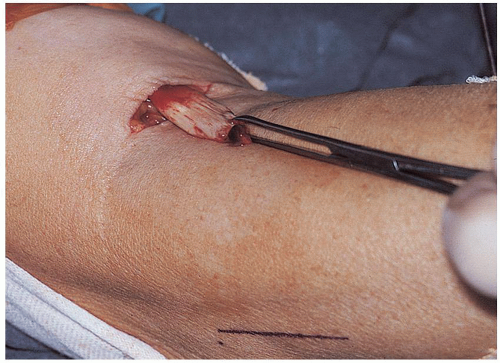 FIGURE 21-6 The tendon is identified by digital palpation and delivered through the skin incision revealing a bulbous degenerative process at the site of disruption. |
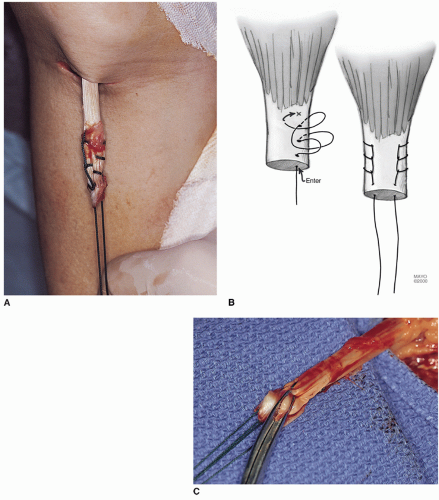 FIGURE 21-7 A,B: Two No. 5 nonabsorbable sutures are inserted by the crisscross Bunnell or Krackow locking technique. The tendon is brought into the surgical field (C). |
Forearm Incision A curved clamp is then introduced into the tunnel previously occupied by the biceps tendon (Fig. 21-8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree