Physiatrists play a critical role in managing the medical and functional consequences of serious burn injuries. Goals of rehabilitation include wound healing, scar prevention, hypertrophic scarring suppression, full range of motion, strengthening, and independent mobility and activities of daily living. This article is an overview of burn rehabilitation principles and patient management. The ultimate rehabilitation goal is independence in all spheres of an individual’s life. Achievement of independence depends on the commitment of the injured individual and the entire health care team.
Burn injury is not a new problem. Since ancient times, humans have known the tragedy of severe burn injuries. Hippocrates described treatments for burn injury in his early works . During the first century of Rome, Cornelius Celsus described a technique for surgical excision of burn scar .
The economic and human cost of burn injuries is enormous. Excluding the tragedy of September 11, 2001, on average more than 3900 persons die from fire each year. An additional 750 persons die from motor vehicle and airplane crashes, contact with electricity, chemicals, or other causes of burn. In 2005, more individuals died secondary to fire than all natural disasters combined. The direct cost of burn injuries is staggering, exceeding more than $10 billion in the year 2005 alone . Residential fires account for most burn injuries. Cooking fires account for 47% of residential fires, and heating fires account for 19% . The incidence of fires involving persons over age 65 is increasing as the population of the United States ages .
Age impacts survival, with mortality highest in very young and very old persons. Thirty-five percent of burn injuries occur in children. Burns are also the primary cause of accidental death in children younger than age 2 and the second cause of death for children younger than age 4. The most common type of childhood burn is a scald injury, which accounts for 72% of pediatric burns . Most (85%) pediatric burns occur in residential settings. Nationally, approximately 20% of pediatric burn injures are nonaccidental burns and result from abuse or neglect. It is critical for clinicians to differentiate between burn injuries caused by child abuse and those caused by accidental injuries .
Approximately 50,000 persons (4%) who sustain a burn injury each year require hospitalization, and approximately 95% survive a burn injury . In individuals who have equivalent sizes of burn, the presence of an inhalation injury reduces survival rate 30% to 50% . Most victims of fire die of inhalation injury, not burns .
The integument
As the largest organ of the body, the skin provides a mechanical barrier that protects internal organs. The skin also provides an immunologic defense, supports fluid homeostasis, and assists with thermoregulation. Skin is a complex organ composed of two major layers—the epidermis and dermis—and a network of collagen, elastic fibers, blood vessels, and nerve endings. The biomechanical properties of skin allow for normal body motion. Skin demonstrates a complex response to mechanical loading. It elongates with low loads; however, once the limit of extensibility is reached, the tissue tears. This limit is called the yield point. The skin also demonstrates preconditioning. After several repetitive applications of a low load, it demonstrates a variable relationship between stress and strain. After several repetitions, the stress-strain relationship stabilizes, which means that the initial rapid elongation with stretch slows and the tissues become stiffer.
Medical care
Burn injury causes necrosis and damage of tissue secondary to exposure to an external agent. It can result from thermal, electrical, frostbite, chemical, or radiation exposure. Response to injury involves a series of complex physiologic events. In addition to local tissue responses, systemic responses involve the cardiovascular, pulmonary, metabolic, endocrinologic, and immunologic systems.
Most burn injuries (>90%) are thermal in nature ; the rest are secondary to other causes, including chemical, electrical, and radiation burns. In addition to managing the airway, breathing, and circulation, initial management includes removing the source of the burn injury and determining causes, the size/extent, and the body location of the injury. Thermal injury ceases once the source is removed, but chemical reactions continue until the offending agent is neutralized or the chemical reaction with the tissues is complete. The presence of an inhalation injury or other coexisting injuries must be determined because these comorbidities impact medical and surgical management.
Serious burns require care by burn care specialists at a burn center that has multispecialty and multidisciplinary staff who are experienced in managing burn injuries. The criteria established by the American Burn Association for transfer of patients who have burn injuries to a burn center include burns that cover more than 10% of the total body surface area (TBSA), electrical injuries, chemical burns, and injuries to specialized body regions, such as the face and genitalia.
Medical care
Burn injury causes necrosis and damage of tissue secondary to exposure to an external agent. It can result from thermal, electrical, frostbite, chemical, or radiation exposure. Response to injury involves a series of complex physiologic events. In addition to local tissue responses, systemic responses involve the cardiovascular, pulmonary, metabolic, endocrinologic, and immunologic systems.
Most burn injuries (>90%) are thermal in nature ; the rest are secondary to other causes, including chemical, electrical, and radiation burns. In addition to managing the airway, breathing, and circulation, initial management includes removing the source of the burn injury and determining causes, the size/extent, and the body location of the injury. Thermal injury ceases once the source is removed, but chemical reactions continue until the offending agent is neutralized or the chemical reaction with the tissues is complete. The presence of an inhalation injury or other coexisting injuries must be determined because these comorbidities impact medical and surgical management.
Serious burns require care by burn care specialists at a burn center that has multispecialty and multidisciplinary staff who are experienced in managing burn injuries. The criteria established by the American Burn Association for transfer of patients who have burn injuries to a burn center include burns that cover more than 10% of the total body surface area (TBSA), electrical injuries, chemical burns, and injuries to specialized body regions, such as the face and genitalia.
Classification of burns
The severity of a burn is determined by the age of the injured individual, the extent and depth of burn injury, and the presence or absence of associated injuries.
Burn depth
The extent to which the epidermis and dermis are injured determines the depth of injury. Describing a burn injury as superficial or partial or full thickness is increasingly preferred over the traditional classification of first-, second-, third-, and fourth-degree burns. Partial- and full-thickness burns impact fluid homeostasis, thermoregulation, and the body’s defense against infection. Loss of tissue integrity and disruption of normal microcirculation allow fluid loss and microbial invasion.
First-degree burn or superficial burn is limited to the epidermis. The skin is erythematous and tender. No blistering occurs. These injuries heal within a few days and are not associated with scarring. The damaged epithelium usually exfoliates in 5 to 10 days. Second-degree burns can be classified as superficial, partial-thickness, or deep partial-thickness injuries. These injuries involve the entire epidermis and varying depth of injury to dermis. Superficial partial-thickness burns are limited to the upper third of the dermis. Microvascular damage and increased capillary permeability occur, causing blistering. These wounds are painful because sensory nerve endings are exposed. They typically heal in 7 to 14 days.
In deep partial-thickness burns, the epidermis and dermis are injured and only the skin appendages, such as sebaceous gland and hair follicles, are spared. The wound is red and blanches with pressure. Typically these wounds are less painful because most nerve endings are destroyed. A marginal residual blood supply exists. A few epithelial cells survive in the hair follicles and other skin appendages. Repopulation by epithelial cells is slow. Regeneration with eventual wound closure can take weeks and months depending on the wound size. Wounds that heal in this manner demonstrate a poor cosmetic and functional outcome. Skin grafts are used to expedite wound closure and healing. Early closure prevents complications such as infection and leads to better cosmetic and functional outcomes .
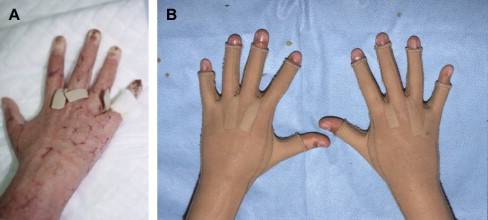
In full-thickness burns, the entire dermis and epidermis are lost. The wound bed is avascular, the texture is dry and leathery, and the wound is insensitive to pain. These burns have a white, brown, or tan waxy appearance and may appear charred. The skin does not blanch or refill because the blood vessels are thrombosed or destroyed ( Figs. 1 and 2 ). Distinguishing a full-thickness burn from a deep partial-thickness injury is often difficult, particularly during the first 3 to 5 days. When the depth of the wound is in question, the wound is treated as a full-thickness injury. Infection or inadequate circulation can convert a partial-thickness injury to a full-thickness wound. Re-epithelialization does not occur because no epithelial cells remain. These wounds require skin grafting unless the wound is small. Thick, dense scarring results. Fourth-degree burns extend to deep structures such as muscle, tendon, and bone. This type of burn is a severe injury that may require amputation or extensive deep débridement.


Extent of the burn injury
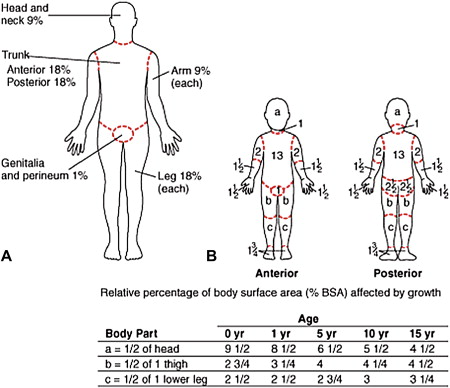
The extent of the injury is determined by the TBSA involved. The Rule of Nines is a commonly used as an estimate of injury in adults ( Box 1 ) . The surface area of the palm of the hand is approximately 1% of the patient’s body surface area and can be used as a quick estimate.
Head and neck, 9%
Each upper extremity, 9%
Each lower extremity, 18%
Anterior trunk, 18%
Posterior trunk, 18%
Perineum, 1%
For children, the Rule of Nines is not an accurate measure because a child’s body proportions are not the same as an adult’s. For instance, a child’s head is proportionately larger than an adult’s and an infant’s legs are proportionately smaller (approximately 13%). The Lund and Browder chart is more accurate and provides some correction for developmental differences ( Fig. 3 ) . When calculating the TBSA of a burn injury, only partial- and full-thickness areas of injury are included. Superficial wounds are not calculated in TBSA percent determination.
Medical and surgical care
The long-term goal of burn wound care is to restore skin integrity, function, and appearance. Immediate goals are to prevent infection, decrease pain, prepare wounds for grafting if needed, prevent contracture, prevent and suppress scarring, while maintaining strength and function.
Burn wound care
Wound débridement, the process of removing devitalized tissue and creating a viable base for wound healing and grafting, is typically required. Eschar is a coagulum of necrotic tissue composed of denatured collagen, elastin, and protein. Eschar and devitalized tissue are excellent media for bacterial growth and must be removed. There are several techniques of débridement. Mechanical débridement includes such things as wet-to-dry dressing and hydrotherapy via water immersion or spraying. Enzymatic débridement uses commercially available topical enzymes, such as sutilains, to induce proteolysis, fibrinolysis, and collagenolysis. These agents may result in local pain and cellulitis in some individuals. Their use is limited to small areas requiring débridement. Surgical débridement procedures include sequential and fascial débridement. Sequential or tangential wound débridement removes thin slices of tissue until a viable tissue bed is identified. Fascial débridement involves surgical removal of tissue down to fascia. Although a viable wound is virtually ensured, a significant soft tissue defect occurs.
Deep skin burns are inelastic. In the case of a circumferential wound of the leg, the burned skin does not expand to allow for increasing edema. In circumferential burns, a tourniquet-like phenomenon can occur and create a tissue compartment with pressure that reaches 40 mm Hg or higher. In this situation, surgical decompression of these compartments must be urgently done or necrosis of the underlying tissues occurs. Escharotomy is a surgical intervention performed to relieve the tourniquet effect of devitalized nonextensible burn tissue. This procedure is critical to limb salvage in full-thickness circumferential injuries of the arms or legs. Incisions are made medially and laterally throughout the length of the extremity involved. It is performed with the arms supinated ( Fig. 4 ). If this procedure is not successful, fasciotomy is performed.

Wound dressings and skin grafts
Biologic dressings are biologic tissues used for wound closure. These dressings provide for early wound coverage, reduce pain, decrease infection, and limit evaporative fluid loss. Cadaveric tissue and human fetal membranes are termed homografts. Porcine grafts, which are heterografts or xenografts, are also used. In addition to the goals mentioned, these temporary grafts are used as test grafts to determine if a wound will accept an autograft. Often a patient’s immune system rejects these grafts. Typically these grafts are changed after several days. Synthetic wound dressings include polyvinylchloride and polyurethanes and other plastic membranes that are water and gas permeable. These temporary dressings are used until the wound has healed or autografting is possible. Bilaminate analogs, composed of thin sheets of silastic and epidermal/dermal analogs, are available. Biobrane and Integra are probably the two most commonly used analogs. Autografting is the surgical transfer of skin from one body site of the patient to another. Autografts are applied once the wound bed is free of devitalized tissue and is not infected. A wound biopsy with a bacterial count of less than 10 6 is needed for the wound to accept a skin graft .
Split-thickness grafts, which are grafts of partial-thickness skin, are applied in sheets or meshed. Meshed autografts undergo a process of creating small, staggered parallel slits in the sheet of skin. Meshing expands the size of the graft from 1.5 times its original area to several times its normal surface area. One disadvantage is that the greater the degree the graft is meshed and expanded, the poorer the cosmetic outcome. The epithelialization of the interstices creates a mesh pattern that persists after the wound is healed. Sheet grafts are more cosmetic because no interstices are cut into the graft. Sheet grafts are typically used for cosmetically important areas, such as the face and hands. Full-thickness skin grafts are used for small areas or critical areas, such as the palms of the hands, and are used in reconstructive procedures. These grafts, as the term implies, involve removing the entire skin thickness from one area and moving it to another . Cultured epidermal autographs are sheets of cultured keratinocytes that show some promise but are currently under development and are not commonly used .
Rehabilitation
The ultimate goal of rehabilitation after a burn injury is to assist an individual in achieving optimal function and independence. This is a multistage process that requires months—even years—of treatment and patient commitment. The goals of the acute period of burn rehabilitation are to promote wound healing and scar suppression, reduce pain, and prevent complications. Patient goals are individualized by burn location, depth of injury, percent of body surface injured, associated injuries and complications. An individual’s age, previous functional level, and health also play a significant role in determining a rehabilitation plan.
Joint care and protection
Proper positioning of the body is fundamental to preventing the development of contractures. This also prevents compression neuropathies and decubitus ulcers. The primary underlying principle of positioning is to keep tissues in an elongated state, which can be difficult because an injured individual typically assumes a position of comfort (ie, flexion and adduction). Extension and abduction are usually the most appropriate positions, but positioning must be individualized in accord with each person’s specific injuries. Joints with deep partial-thickness or full-thickness burns overlying them are at high risk for developing contracture and must be kept in an elongated state ( Fig. 5 ).
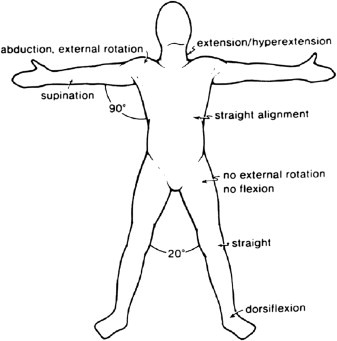
Splints are used to prevent joint contractures, maintain proper positioning, protect skin grafts, and prevent or assist motion. Splints should be “user friendly” for the patient, nursing staff, and other caregivers. Poorly applied splints can cause nerve injury, loss of skin grafts, and worsening of a burn wound and cause new wounds. An effective splint avoids pressure over bony prominences and is compatible with wound dressings and topical medications. Splints fabricated of re-moldable materials can be modified as a patient’s needs change. Factors to consider when prescribing a splint include the area of the body injured, extent and type of injury, the functional goal, and the ability of the patient to participate.
If normal range of motion (ROM) of a joint is maintained, a splint is typically not indicated. Exposed tendons require splinting in a slack position. If a joint is exposed, a splint is indicated to provide protection. Joints that have not sustained an overlying or direct injury typically do not require splinting. Splinting or a positioning device may be needed in some additional situations, such as preventing ankle contractures during prolonged bed rest. During the acute period, many types of splints can be prescribed. Upper and lower extremity splints include knee extension splints to prevent knee flexion contracture and posterior foot drop splints to maintain neutral ankle dorsiflexion. In the case of axillary burns, a splint that holds the upper extremity at 90° abduction to the side, often called an “airplane” splint, is used to prevent shoulder adduction contracture. Custom splints can be designed for virtually all parts of the body. Commercially available designs, which may reduce costs, are also available but often need modifications to fit appropriately.
Exercise
Establishing a therapeutic exercise plan requires an understanding of the location, depth, and TBSA of an individual’s burn injury. Pre-existing medical problems, such as coronary artery disease, impact the exercise prescription for an individual patient. The strength and endurance of burn patients also are compromised because of bed rest. Loss of strength in an inactive muscle is approximately 3% per day and 22% by 1 week . The goal of exercise is to maintain normal ROM, strength, and endurance. If a patient is alert and able to participate, a program of active and active-assisted exercise is appropriate. For obtunded or critically ill patients, passive ROM exercises that emphasize the end of ROM are prescribed. In the event that full ROM is not maintained, a program of stretching is prescribed.
ROM can be performed with a patient under anesthesia. It is often a good choice for pediatric cases and for patients who cannot tolerate the pain of ROM. Anesthesia allows accurate determination of ROM without inducing pain. Effective stretching requires a slow sustained stretch. Stretching skin is not equivalent to stretching muscle, in which active contraction and relaxation of the tissue is under patient control. Skin, a tissue without active contractile elements, requires sustained mechanical stretch to facilitate alignment lengthening of the underlying collagen and other fibers.
Skin demonstrates preconditioning, that is, initially it shows increasing elongation at repetitive low loads but then the change in length plateaus. Once this stage of preconditioning is reached, a prolonged stretch is applied to maximize the stretch. In short, the joint is repeatedly moved slowly to its end range several times before applying a prolonged stretch. When prolonged stretch is performed, the stretch is maintained until the tissue blanches. Blanching is a clinical sign that capillary blood flow is impeded and the tissue’s yield point is approaching .
Strengthening exercise begins as soon as a patient can tolerate it. Strengthening programs include a wide range of programs, including progressive resistive exercise. Fatigue and loss of endurance are major issues as a patient recovers. It is important to include endurance training and monitor cardiopulmonary response.
Immediately after autografting, active and passive exercises are not performed on the limb. Depending on the type of graft, condition of the graft wound, and the judgment of the surgeon, no exercise or ROM is performed for approximately 3 days for mesh grafts and 5 days for sheet grafts. Splints are used to protect the graft and maintain tissue length. Heterografts, synthetic dressings, escharotomies, and surgical débridements are not contraindications to exercise.
Ambulation
Walking is an important activity. Ambulating patients have fewer lower extremity contractures, endurance problems, and venous thromboses. Early ambulation maintains independence, balance, lower extremity ROM, and function and decreases the risk of deep venous thrombosis. Once a patient’s condition allows, ambulation should begin. Although the expertise of a physical therapist may be needed initially for many patients to resume ambulation, nurses and family can be taught to assist and encourage patients to ambulate. Physical therapy sessions should not be the only time a patient ambulates.
Autografts to the lower extremities are a contraindication to ambulating until stable circulation to the graft sites is established. Typically, depending on the surgeon and the condition of the graft, the patient may not be permitted to put lower extremities in a dependent position for 5 to 7 days after grafting. Once a patient is cleared by the surgeon to resume lower extremity weight bearing, a program of dangling the lower extremities is initiated as a preambulation exercise. Dangling also helps to determine if the graft tolerates the dependent position. Elastic wraps or other forms of compression are used to avoid venous pooling, which can lead to graft sloughing. The graft is evaluated before and after dangling. Initially, the limb is dangled for 5 minutes and the duration is progressively increased. If the graft tolerates dependency, walking with ace wraps or other support is begun. Ambulation time is increased daily if no untoward effects on the graft occur. Gait deviations are common. There are multiple causes, including abnormalities caused by the location of the injury, pain, focal or generalized weakness, contractures, impaired sensation, and central nervous system causes. Although some gait deviations resolve as wounds heal, some persist if not addressed early.
Scoliosis and kyphosis may occur because of asymmetrical burn injuries of the trunk, pelvis, and shoulder regions. This type of injury can result in abnormal posture. Aggressive exercise and positioning are critical to prevent these abnormalities, which is especially important during the growing years of childhood. Gait devices are used to protect, reduce pain, or assist with weight bearing of injured lower extremities. These devices also can prevent or correct abnormal posture or gait caused by burns of the chest, back, or other areas that cause the patient to stand or move abnormally.
Finally, during periods when a patient cannot ambulate, wheelchairs provide mobility and can be adapted to patients needs, including using elevating leg rests and attaching splints and other position devices to the chair.
The hand
The hand is a highly specialized body part that not only allows fine and gross motor function but also has great social importance in communication and human interaction. Injuries to the hand require intense and specialized attention. Hand splints are used to preserve function and prevent contracture. The resting hand splint positions the wrist in slight extension, 60° to 80° of metacarpophalangeal flexion, full interphalangeal extension, and thumb abduction. This position places the flexors and extensor, tendons, and ligaments under maximal stretch to avoid the soft tissue shortening associated with contractures.
Hand edema leads to deformation, which makes edema control a major priority. Edema is an interstitial protein-rich substance that forms a gel-like consistency and impedes vascular clearance. Mechanical joint and soft tissue motion is inhibited and contracture develops. Elevation of the hand and arm is accomplished using splints, casts, bedside troughs, or other devices used to inhibit edema formation ( Fig. 6 ). Web spacers can be placed between digits to prevent fluid collection and edema formation. Once the wounds of the hand are closed, compression gloves are placed to control edema further.