The prosthetic and orthotic field is in constant flux, with newer technology and materials being incorporated into everyday practice. Research into the field is increasing as interest in restoring or simulating lost human function becomes more of a reality with advances in computer and microprocessor technology. This article explores the world of braces and artificial limbs, and reviews the inherent challenges encountered during rehabilitation of patients who have these specific orthotic/prosthetic needs. The authors provide quick-reference tables and highlight critical information needed to manage patients. It examines newer technology being developed and gauges how close the field really is to the era of Steve Austin, television’s Six-Million Dollar Man.
This article focuses on the basic principles of orthotic principles, applications, and prosthetic restoration rehabilitation. If physiatrists and other rehabilitation team members use these fundamental principles, patients will experience optimal care and hopefully successful outcomes. As in any field of medicine, this text cannot substitute for the need to follow ongoing research, learn from the patient, and exercise sound clinical judgment. The goal was not to reproduce the compendium of orthotics and prosthetics in an article this size, but to provide essential information in a succinct format that augments the knowledge base of today’s busy health care providers. An abundance of newer materials and technology is available for patients, but that does not mean every patient will benefit. This article outlines what factors influence component choices.
Introduction to orthotics
Orthoses can serve multiple functions, including controlling, correcting, facilitating, limiting, or inhibiting motion of the extremities or spine. Orthoses can also substitute for weak or paralyzed muscles and reduce muscle spasticity. These goals are not mutually exclusive; to maximize patient outcome, many clinical scenarios require complementary use of these functions.
Abnormal biomechanics can affect any age group and typically result from orthopedic, neurologic, or musculoskeletal pathology. The underlying pathology and biomechanics must be considered when prescribing an orthosis. However, physicians must also consider the individual patient’s personal goals and expectations.
In 1989 the International Standards Organization (ISO) endorsed a standardization of terms to describe orthoses and prostheses. The ISO terminology describes the orthoses based on the joints they encompass and the desired function. Therefore, an orthosis that encompasses the foot and ankle is termed an ankle foot orthosis (AFO), and one that envelops the knee, foot, and ankle is referred to as knee ankle foot orthosis (KAFO). Similarly, an orthosis that encompasses the lumbar and sacral spine is referred to as lumbosacral orthosis, and so forth, including the thoracolumbosacral, cervicothoracolumbosacral, cervical (CO), and cervicothoracic (CTO) orthoses. However, despite this classification system, many other traditional ways of naming and categorizing orthoses persist. Some orthoses retain the name of the place where it was developed (e.g., Miami J cervical orthosis), are named based on the materials used in fabrication (e.g., a double upright metal AFO) or the patient’s diagnosis (e.g., scoliosis brace).
Human motion occurs not only in rotational and translation planes, but more typically in combination. Rotational movement is angular, whereas translation motion occurs without an angular component. The strength of the angular force determines torque. The rotational and nonrotational components, the distance from the axis of motion, and the magnitude of the force determine the effect of torque.
When designing or fabricating an orthosis, one must weigh the effect of the torque on the anatomic joints, particularly with a dynamic orthosis. Levers can be used to amplify force.
Minimizing pressure on body tissues prevents injury and improves patient tolerance of an orthosis. Pressure is limited by moment and force. Moment equals the lever arm length and the force applied. Using the longest lever arm feasible is advantageous because the same moment can be created using less force, minimizing the pressure on the body. Hence many orthoses are classified as first-class levers. Because pressure equals force per unit area using broad cuff, bands and pads can reduce the pressure on body structures.
The three-point force system, also called a three-point pressure system , is also a fundamental of orthotic principle. Two forces acting opposite to a third prevents motion in that direction. An orthosis can have one or more three-point systems incorporated in its design.
A wide range of materials are used in fabricating an orthosis and are frequently used in combination. Metals are durable but are often considered unattractive and heavy. Thermoplastic orthoses are more cosmetic, especially high-temperature thermoplastics, which can be more transparent. Although they are not as strong or durable as metal, they are effective for long-term use. Low-temperature plastics are moldable at temperatures of 140° to 170°F and come in various colors, which may make the orthosis more appealing to children and adults. These plastics can be molded directly on the body area, unlike high-temperature plastic (copolymer polypropylene), which softens at a higher temperature. Low-temperature plastics (orthoplast) can be reheated and remolded but are not as durable or as strong as high-temperature plastics.
High-temperature plastic requires a mold onto which to be fitted. Some of these plastics are flexible and hold their shape well. They soften at temperatures greater than 170°F and can be reheated to allow some remolding. Plastic materials allow application of foam materials to the inner aspect of the orthosis to increase comfort or provide protection.
Thermosetting plastics are used for lamination. They must be set; that is, they harden at high temperatures. They are not remoldable, do not soften with heat, and are often heavier than thermoplastics.
Some of the newest materials that have emerged into mainstream manufacturing include preimpregnated (prepreg) carbon fibers and Ready Preg . Prepregs are carbon textile fabrics preimpregnated with curable resins by the manufacturer. The manufacturer precisely controls the amount and type of resin to create consistent ratios of fiber to resin for maximum strength and quality, allowing for quicker and consistent manufacturing with lower costs in material and labor.
An orthosis is commonly called a brace by the general public. An orthotist is the individual trained to fit and fabricate orthoses. Orthotics is the study of orthoses.
Several terms are fundamental to understanding orthotic design, including free, assist, resist, stop and variable . The term free indicates that unrestricted movement is permitted in one plane. An assist means that an external force is applied to facilitate increased velocity, force, or range of motion (ROM), whereas resist provides the opposite function of an assist. A stop is a mechanical feature built into the device to prevent an undesired motion in a specific plane. The term variable means a feature can be adjusted without altering the basic structure of the orthosis.
Ideally, an orthosis is simple in design, patient-friendly, comfortable, and durable, and provides the intended function. Additionally, it should be affordable, made of high quality materials, and worth the investment of time and money.
Lower extremity orthotics
Foot orthosis and shoe modifications
Foot orthoses (FOs) normalize the foot’s architecture and function. The primary goal is to redistribute the forces experienced by the foot during the stance phase of weight bearing. If correction of the foot is not feasible, the FO may be prescribed to accommodate for foot abnormalities. Common causes of foot abnormalities include neuropathy, architectural bone changes, and muscle dysfunction.
Prescribing a FO requires an understanding of the diagnosis, its impact on the function and form of the foot, the desired biomechanical correction or accommodation, and patient characteristics, such as the patient’s weight, activity level, and other comorbidities.
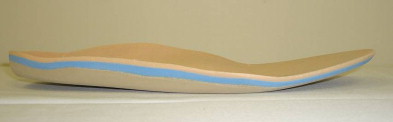
A foot orthosis is composed of three basic layers ( Fig. 1 ). A firm base functions to support or control the foot structure and achieve or maintain normal alignment. If normal alignment is not achievable, the FO should effectively accommodate the abnormality. A moderately dense middle layer functions as a shock absorber. A soft layer or covering is applied to prevent shearing of the plantar aspect of the foot and aids in pressure identification.
FOs and shoe modifications are indicated in many clinical scenarios. Leg length discrepancy is a common clinical problem. Treatment goals include equalizing limb length, creating a more symmetric posture, and improving gait. If the leg length discrepancy is greater than 1 inch, the correction should be placed on the outside heel and sole of the shoe. However, if a discrepancy of 0.5 to 1 inch is present, modification of the external heel is appropriate. If the discrepancy is less than 0.5 inch, no correction is typically needed unless the patient is symptomatic.
In the case of subtalar joint arthritis, fusion, or instability, the goals are pain relief through limiting joint motion, joint support, and accommodation of deformities. Treatment options include a high-quarter shoe with reinforced counters, long steel shank, rocker sole, and a shock-absorbing cushioned heel. The steel shank decreases joint motion and reduces pain. A rocker sole modification facilitates forward progression during stance and reduces the duration of weight bearing. FOs with a soft layer for comfort and a semirigid layer for support are also helpful.
Pes planovalgus deformity requires reduction in eversion coupled with support of the longitudinal arch. Children are effectively treated with a high-quarter shoe with broad heel, long medial counter, and medial heel wedge. Adults do well with a Thomas heel and medial heel wedge. The FO should be designed to provide medial longitudinal arch support.
The treatment goals for pes cavus deformity include redistributing the weight-bearing over the entire foot to reduce pressure at the metatarsals. In addition to high-quarter shoes with a high toe box, lateral heel, and sole wedging, the FO should include metatarsal relief and medial and lateral longitudinal arch support.
The treatment goals for a fixed pes equinus deformity include the provision of heel strike, containment of the foot in the shoe, and reduction of pressure at the metatarsal heads. If the condition is unilateral, another goal is leg-length equalization. In addition to prescribing a FO with medial longitudinal arch support, a high-quarter shoe with heel elevation, modified lace stay for wide opening, and possible addition of a rocker bar on the sole of the shoe may also be used.
In the case of pes varus, the treatment goal depends on whether the foot is flexible or fixed. With a flexible deformity, the goal is achieving normal alignment. However, if the deformity is fixed, a prescription for a FO and a shoe that accommodates the foot abnormalities is indicated.
Metatarsalgia, painful metatarsal heads, is managed through reducing pressure over the metatarsal heads and supporting the transverse arch. The FO can be fabricated with a metatarsal pad or sesamoid pad to alleviate pressure over the painful metatarsals. Effective shoe modifications include a metatarsal bar or rocker sole.
Hallux valgus is a common deformity. Treatment focuses on reducing pressure on the first metatarsophalangeal joint and great toe by preventing forward foot slide. Pain is also reduced by immobilizing the first metatarsophalangeal and shifting weight to the lateral foot. Shoes that accommodate the deformity are critical and include a shoe with a soft vamp and broad ball and toe box. In more difficult cases, a relief in vamp with cutout or balloon patch is needed coupled with a low-heeled, stiff-soled shoe with rocker bottom. FO prescription should indicate a metatarsal or sesamoid pad to increase the transverse arch, and a medial longitudinal arch support.
Hallux rigidus, restricted motion at the metatarsophalangeal joint of the great toe, results from degenerative arthritis, faulty biomechanics, or structural abnormalities of the foot. Treatment goals include reducing motion or pressure at the first metatarsophalangeal joint and facilitating push-off. A shoe with a stiff sole or modification to increase the stiffness of the foot’s sole reduces pain. The FO should include a sesamoid pad and medial longitudinal arch support.
Foot fractures require immobilization. Depending on the location of the fracture, devices such as a walking cast or off-the-shelf walking boots may be required. Post-fracture healing shoes with a long steel shank to provide rigidity, longitudinal arch support, and metatarsal relief may be necessary.
Diabetes is a common disease, with diabetic peripheral neuropathy a common complication that can lead to insensate foot and even amputation. The treatment goal is to protect the foot and its structure, provide appropriate support, and accommodate any fixed deformities. Custom FOs are prescribed to protect the foot through equalizing weight-bearing pressure over the entire foot, minimizing shear, and accommodating any structural abnormalities. Extra-depth shoes allow extra room in the toe box for hammering or clawing of toes common in peripheral neuropathy.
Charcot foot refers to architectural changes caused by neuropathic disorders, such as diabetes mellitus, alcoholic neuropathy, or syphilis. During the inflammatory phase, a custom bivalved ambulatory AFO is indicated until the chronic phase is reached ( Fig. 2 ).

Chronic architectural changes typically result. Treatment requires accommodation of the resulting fixed deformities. Custom deer skin shoes may be required ( Fig. 3 ).

Custom FO should be designed to appropriately distribute weight-bearing forces.
Ankle foot orthosis
AFOs are most commonly prescribed for lower-extremity weakness, such as dorsiflexion or plantar flexion weakness. AFOs are also used to control medial lateral instability or reduce axial loading of the leg. Because ankle plantar flexion facilitates an extension moment at the knee, an AFO can be used to control knee extension. One must remember that although an AFO does not control the knee, it can strongly influence knee function.
AFOs with sagittal control systems influence plantar and dorsiflexion ( Fig. 4 and Table 1 ). The floor-reaction AFO uses ground reaction forces to stabilize ankle mortise and creates an extension moment at the knee, resulting in stability ( Fig. 5 ).

| Type | Function | Materials |
|---|---|---|
| Leaf spring AFO | Prevents plantar flexion, allows dorsiflexion | Plastic, metal, or carbon fiber |
| Semirigid AFO | Resists plantar flexion, allows little dorsiflexion | Plastic or metal |
| Solid ankle AFO | Inhibits sagittal motion | Plastic or metal; if made of plastic, the anterior trim line is in front of the malleoli |

Less commonly seen is the patellar tendon–bearing AFO that provides axial unloading through incorporating a patellar tendon bar to accept the forces at the ankle ( Fig. 6 ).

A prescription for an AFO may or may not order an ankle joint. An AFO may include a joint to allow dorsiflexion or plantar flexion of varying degrees. A solid ankle in an orthosis prevents ankle motion in all directions. A stop, which is a static mechanical unit, can be added to an orthosis to inhibit an undesired motion ( Table 2 ).
| Type of ankle joint | Function | Clinical indications |
|---|---|---|
| Limited motion | Variable; allows adjustment of PF and DF settings | Contracture treatment |
| Change in PF and DF function or strength anticipated | ||
| Free-motion | Provides medial lateral stability while full range of motion in the sagittal plane | Ankle joint instability in the mediolateral plane |
| PF and DF function is normal | ||
| Dorsiflexion-assist | Facilitates DF; PF stop is also typically incorporated | Peroneal mononeuropathy |
| Common causes of foot drop (except spasticity) | ||
| Plantar flexion stop | Inhibits PF motion | Extensor synergy spasticity |
| Clonus | ||
| Genu recurvatum | ||
| Dorsiflexion stop | Inhibits DF; facilitates extension moment at the knee | Accommodates for weak plantar flexor |
| Weak quadriceps muscles |
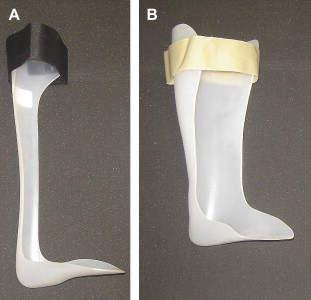
The common option when an ankle joint is not needed is the leaf spring design, commonly used for flaccid foot drop ( Fig. 7 A). A solid ankle AFO is indicated if medial lateral ankle instability, ankle fusion, or ankle pain with gait is present, or in cases of diffuse lower-extremity weakness ( Fig. 7 B). These AFOs do not include an external ankle joint.
An AFO can be designed to provide control in the coronal plane. Medial and lateral control is achieved in metal and leather AFOs through incorporating a T-strap at the ankle to direct the ankle in a varus or valgus direction. AFOs made of plastic use a valgus correction (sustentaculum tali modification) or a plastic extension medially/laterally above the ankle to control varus and valgus motion. Additionally, a high medial or lateral trim line on the foot plate can also be used. If an AFO is laminated, the rigid characteristics of lamination provide coronal control.
Knee ankle foot orthoses
During gait, the primary functions of the knee are shock absorption, stable support during stance, and limb shortening during the swing phase of ambulation. When an external device is needed to augment the function of the knee and ankle, a KAFO is prescribed. If the problem is limited to the knee alone, a KO is typically prescribed.
Multiple types of KOs are available commercially, which are used to provide medial or lateral stability at the knee ( Fig. 8 ).

KAFOs are typically hybrid orthoses made of metal and plastic with a metal knee joint incorporated. Whenever possible, plastic components are preferred over metal or leather to reduce the weight of the orthosis. Plastics can be used to produce a more intimate fit. Carbon fiber is increasingly being used because it is a strong rigid material but is lightweight. Unlike some plastics, carbon fiber cannot be reheated to allow for remolding, and therefore fit must be precise.
Indications for a KAFO are myriad. KAFOs are most typically prescribed for lower-extremity paralysis or weakness, knee instability, and extension spasticity caused by an upper motor neuron lesion. Components include proximal and distal thigh cuff, calf band, double or single upright metal supports, and metal knee and ankle joints. The orthosis can be made with an unrestricted ankle allowing full dorsiflexion and plantar flexion. Single upright KAFOs are often used for knee instability. The single upright can be placed medially or laterally. For genu valgum, the upright is placed laterally, and medially for genu varus.
Variations exist on the basic design, and various knee locking mechanisms can be chosen. Although double metal uprights provide more stability compared with a single upright, one must consider whether the additional stability outweighs the disadvantage of added weight and bulk.
An orthosis with a free knee does not inhibit knee flexion or extension; however, stops, or mechanical devices that block motion, can be incorporated to limit ROM if required, such as after knee surgery. Variable units that allow for adjusting the orthotic knee ROM are also available.
In addition to evaluating the lower-extremity dysfunction and function the KAFO can provide, one must also consider the other functional problems and comorbidities that may be present. For instance, patients who require a high level of stability for standing and ambulating but have poor, impaired upper-extremity fine motor function would benefit from a KAFO with a bail lock for locking and unlocking the knee ( Fig. 9 ).

Stance-control knees are available. These devices lock once heel strike is achieved and release with toe-off. Typically these devices require hip extension strength of a least fair plus to extend the leg to activate the stance control.
Although total unloading of the lower extremity with a KAFO is not possible, a quadrilateral brim (ie, a plastic thigh portion that extends to the ischial tuberosity) can accept the load of weight-bearing. This device is similar to the quadrilateral socket used in a transfemoral amputation prosthesis.
Lastly, a KAFO can serve as an adjunct to exercise and other therapeutic modalities. A KAFO with a dial lock can maintain a prolonged stretch to treat a knee contracture ( Table 3 ).
| Knee joint | Function | Advantages | Disadvantages | Indications |
|---|---|---|---|---|
| Free-motion knee joint | Provides medial and lateral control and stability | Cosmetic; light weight.; permits full flexion; 180° extension stop; controls any associated genu recurvatum | Good knee extension strength required for knee control; patient must control knee flexion/extension | Unstable knee in coronal plane |
| Polycentric knee | Approximates the anatomic planes of normal knee motion; stability in coronal plane | More biomechanically correct | Weight; not cosmetic | Similar to free-motion knee joint |
| Posterior offset knee | Decreases hyperextension moment; axis of rotation posterior to knee → early extension | Mechanical knee locks before anatomic knee; increased stability from ground reaction forces | Weight; appearance is not cosmetic; not used when hip/knee contracture is present; not appropriate with plantar flexion stop | Decreases hyperextension; maximal stability |
| Drop-lock knee | Locks into place with stance (gravity-assist); knee locked in extension | Locking the knee is hands-free; no bending or use of upper extremity/hands to lock knee; durable; low maintenance | Must manually unlock knee joint; locked knee during gait leads to vaulting or circumduction | Optimal stability in standing or stance is desired |
| Trigger-lock knee | Trigger on proximal thigh allows locking without using upper extremities | No bending required to lock/unlock | Needs periodic adjustment and “tuning”; profile is bulky | Maximal stability in upright is desired |
| Lever-lock with bail release (“Cam,” “Swiss,” or “Bail Lock”) | Engages with full extension; when bail lifted, joint unlocks | Hands-free; no bending to lock/unlock; very stable | Bulky; not cosmetic; unlocks unexpectedly if bumped; bail mechanism wears clothing | Maximal stability desired; work well for persons lacking arm and hand function; useful for those who have compromised balance |
| Dial-lock knee | Allow static extension and support of the knee | Adjustment can be made in 6° increments | Difficult to ambulate; wear out, requiring replacement | Knee flexion contracture improving but requires further intervention |
| Ultraflex knee joint | Provides low-load prolonged tension for stretch | Constant stretch; tension adjustable; rate of spring tension is constant and independent of joint angle | Bulky; ambulation is difficult | |
| Stance-control knee | Provides secured knee extension with weight-bearing; unlocks with toe-off | Drop lock, bail locks are not necessary; frees up hands and upper extremities | Must have fair plus or better hip extension strength | Lower-extremity paresis or paralysis |
Hip orthosis
Hip orthoses are used for hip flexion, extension, abduction, and adduction. They are not effective for controlling hip external and internal rotation, but are frequently used after hip arthroplasty and surgical correction of the hip to control hip adduction. If control rotation at the hip is indicated, the orthosis must be converted to a hip knee ankle foot orthosis (HKAFO) to allow further control.
Hip knee ankle foot orthoses
HKAFOs controls flexion, extension, abduction, and adduction, and also hip rotation through the below-the-knee components and the foot plate. These orthoses provide maximal support of the lower extremities. They are used in cases of paraplegia from spinal cord injury, poliomyelitis, or other causes. These also allow upright standing and ambulation with a walker and swing-to or swing-through gait pattern.
Essentially an HKAFO is a KAFO with a pelvic band and hip joint added. They are heavy and cumbersome, although the advent of lighter weight materials has helped. These orthoses cause high energy consumption during gait .
A reciprocating gait orthoses is also known as a lumbosacral HKAFO with cables. The cable system couples the flexion and extension of the bilateral hips. This coupling results in extension of the contralateral hip when the other hip is flexed. A release mechanism to allow simultaneous hip flexion is incorporated. This design has been shown to decrease energy expenditure and increase ambulation speed and distance in the community .
Lower extremity orthotics
Foot orthosis and shoe modifications
Foot orthoses (FOs) normalize the foot’s architecture and function. The primary goal is to redistribute the forces experienced by the foot during the stance phase of weight bearing. If correction of the foot is not feasible, the FO may be prescribed to accommodate for foot abnormalities. Common causes of foot abnormalities include neuropathy, architectural bone changes, and muscle dysfunction.
Prescribing a FO requires an understanding of the diagnosis, its impact on the function and form of the foot, the desired biomechanical correction or accommodation, and patient characteristics, such as the patient’s weight, activity level, and other comorbidities.
A foot orthosis is composed of three basic layers ( Fig. 1 ). A firm base functions to support or control the foot structure and achieve or maintain normal alignment. If normal alignment is not achievable, the FO should effectively accommodate the abnormality. A moderately dense middle layer functions as a shock absorber. A soft layer or covering is applied to prevent shearing of the plantar aspect of the foot and aids in pressure identification.
FOs and shoe modifications are indicated in many clinical scenarios. Leg length discrepancy is a common clinical problem. Treatment goals include equalizing limb length, creating a more symmetric posture, and improving gait. If the leg length discrepancy is greater than 1 inch, the correction should be placed on the outside heel and sole of the shoe. However, if a discrepancy of 0.5 to 1 inch is present, modification of the external heel is appropriate. If the discrepancy is less than 0.5 inch, no correction is typically needed unless the patient is symptomatic.
In the case of subtalar joint arthritis, fusion, or instability, the goals are pain relief through limiting joint motion, joint support, and accommodation of deformities. Treatment options include a high-quarter shoe with reinforced counters, long steel shank, rocker sole, and a shock-absorbing cushioned heel. The steel shank decreases joint motion and reduces pain. A rocker sole modification facilitates forward progression during stance and reduces the duration of weight bearing. FOs with a soft layer for comfort and a semirigid layer for support are also helpful.
Pes planovalgus deformity requires reduction in eversion coupled with support of the longitudinal arch. Children are effectively treated with a high-quarter shoe with broad heel, long medial counter, and medial heel wedge. Adults do well with a Thomas heel and medial heel wedge. The FO should be designed to provide medial longitudinal arch support.
The treatment goals for pes cavus deformity include redistributing the weight-bearing over the entire foot to reduce pressure at the metatarsals. In addition to high-quarter shoes with a high toe box, lateral heel, and sole wedging, the FO should include metatarsal relief and medial and lateral longitudinal arch support.
The treatment goals for a fixed pes equinus deformity include the provision of heel strike, containment of the foot in the shoe, and reduction of pressure at the metatarsal heads. If the condition is unilateral, another goal is leg-length equalization. In addition to prescribing a FO with medial longitudinal arch support, a high-quarter shoe with heel elevation, modified lace stay for wide opening, and possible addition of a rocker bar on the sole of the shoe may also be used.
In the case of pes varus, the treatment goal depends on whether the foot is flexible or fixed. With a flexible deformity, the goal is achieving normal alignment. However, if the deformity is fixed, a prescription for a FO and a shoe that accommodates the foot abnormalities is indicated.
Metatarsalgia, painful metatarsal heads, is managed through reducing pressure over the metatarsal heads and supporting the transverse arch. The FO can be fabricated with a metatarsal pad or sesamoid pad to alleviate pressure over the painful metatarsals. Effective shoe modifications include a metatarsal bar or rocker sole.
Hallux valgus is a common deformity. Treatment focuses on reducing pressure on the first metatarsophalangeal joint and great toe by preventing forward foot slide. Pain is also reduced by immobilizing the first metatarsophalangeal and shifting weight to the lateral foot. Shoes that accommodate the deformity are critical and include a shoe with a soft vamp and broad ball and toe box. In more difficult cases, a relief in vamp with cutout or balloon patch is needed coupled with a low-heeled, stiff-soled shoe with rocker bottom. FO prescription should indicate a metatarsal or sesamoid pad to increase the transverse arch, and a medial longitudinal arch support.
Hallux rigidus, restricted motion at the metatarsophalangeal joint of the great toe, results from degenerative arthritis, faulty biomechanics, or structural abnormalities of the foot. Treatment goals include reducing motion or pressure at the first metatarsophalangeal joint and facilitating push-off. A shoe with a stiff sole or modification to increase the stiffness of the foot’s sole reduces pain. The FO should include a sesamoid pad and medial longitudinal arch support.
Foot fractures require immobilization. Depending on the location of the fracture, devices such as a walking cast or off-the-shelf walking boots may be required. Post-fracture healing shoes with a long steel shank to provide rigidity, longitudinal arch support, and metatarsal relief may be necessary.
Diabetes is a common disease, with diabetic peripheral neuropathy a common complication that can lead to insensate foot and even amputation. The treatment goal is to protect the foot and its structure, provide appropriate support, and accommodate any fixed deformities. Custom FOs are prescribed to protect the foot through equalizing weight-bearing pressure over the entire foot, minimizing shear, and accommodating any structural abnormalities. Extra-depth shoes allow extra room in the toe box for hammering or clawing of toes common in peripheral neuropathy.
Charcot foot refers to architectural changes caused by neuropathic disorders, such as diabetes mellitus, alcoholic neuropathy, or syphilis. During the inflammatory phase, a custom bivalved ambulatory AFO is indicated until the chronic phase is reached ( Fig. 2 ).
Chronic architectural changes typically result. Treatment requires accommodation of the resulting fixed deformities. Custom deer skin shoes may be required ( Fig. 3 ).
Custom FO should be designed to appropriately distribute weight-bearing forces.
Ankle foot orthosis
AFOs are most commonly prescribed for lower-extremity weakness, such as dorsiflexion or plantar flexion weakness. AFOs are also used to control medial lateral instability or reduce axial loading of the leg. Because ankle plantar flexion facilitates an extension moment at the knee, an AFO can be used to control knee extension. One must remember that although an AFO does not control the knee, it can strongly influence knee function.
AFOs with sagittal control systems influence plantar and dorsiflexion ( Fig. 4 and Table 1 ). The floor-reaction AFO uses ground reaction forces to stabilize ankle mortise and creates an extension moment at the knee, resulting in stability ( Fig. 5 ).
| Type | Function | Materials |
|---|---|---|
| Leaf spring AFO | Prevents plantar flexion, allows dorsiflexion | Plastic, metal, or carbon fiber |
| Semirigid AFO | Resists plantar flexion, allows little dorsiflexion | Plastic or metal |
| Solid ankle AFO | Inhibits sagittal motion | Plastic or metal; if made of plastic, the anterior trim line is in front of the malleoli |
Less commonly seen is the patellar tendon–bearing AFO that provides axial unloading through incorporating a patellar tendon bar to accept the forces at the ankle ( Fig. 6 ).
A prescription for an AFO may or may not order an ankle joint. An AFO may include a joint to allow dorsiflexion or plantar flexion of varying degrees. A solid ankle in an orthosis prevents ankle motion in all directions. A stop, which is a static mechanical unit, can be added to an orthosis to inhibit an undesired motion ( Table 2 ).
| Type of ankle joint | Function | Clinical indications |
|---|---|---|
| Limited motion | Variable; allows adjustment of PF and DF settings | Contracture treatment |
| Change in PF and DF function or strength anticipated | ||
| Free-motion | Provides medial lateral stability while full range of motion in the sagittal plane | Ankle joint instability in the mediolateral plane |
| PF and DF function is normal | ||
| Dorsiflexion-assist | Facilitates DF; PF stop is also typically incorporated | Peroneal mononeuropathy |
| Common causes of foot drop (except spasticity) | ||
| Plantar flexion stop | Inhibits PF motion | Extensor synergy spasticity |
| Clonus | ||
| Genu recurvatum | ||
| Dorsiflexion stop | Inhibits DF; facilitates extension moment at the knee | Accommodates for weak plantar flexor |
| Weak quadriceps muscles |
The common option when an ankle joint is not needed is the leaf spring design, commonly used for flaccid foot drop ( Fig. 7 A). A solid ankle AFO is indicated if medial lateral ankle instability, ankle fusion, or ankle pain with gait is present, or in cases of diffuse lower-extremity weakness ( Fig. 7 B). These AFOs do not include an external ankle joint.
An AFO can be designed to provide control in the coronal plane. Medial and lateral control is achieved in metal and leather AFOs through incorporating a T-strap at the ankle to direct the ankle in a varus or valgus direction. AFOs made of plastic use a valgus correction (sustentaculum tali modification) or a plastic extension medially/laterally above the ankle to control varus and valgus motion. Additionally, a high medial or lateral trim line on the foot plate can also be used. If an AFO is laminated, the rigid characteristics of lamination provide coronal control.
Knee ankle foot orthoses
During gait, the primary functions of the knee are shock absorption, stable support during stance, and limb shortening during the swing phase of ambulation. When an external device is needed to augment the function of the knee and ankle, a KAFO is prescribed. If the problem is limited to the knee alone, a KO is typically prescribed.
Multiple types of KOs are available commercially, which are used to provide medial or lateral stability at the knee ( Fig. 8 ).
KAFOs are typically hybrid orthoses made of metal and plastic with a metal knee joint incorporated. Whenever possible, plastic components are preferred over metal or leather to reduce the weight of the orthosis. Plastics can be used to produce a more intimate fit. Carbon fiber is increasingly being used because it is a strong rigid material but is lightweight. Unlike some plastics, carbon fiber cannot be reheated to allow for remolding, and therefore fit must be precise.
Indications for a KAFO are myriad. KAFOs are most typically prescribed for lower-extremity paralysis or weakness, knee instability, and extension spasticity caused by an upper motor neuron lesion. Components include proximal and distal thigh cuff, calf band, double or single upright metal supports, and metal knee and ankle joints. The orthosis can be made with an unrestricted ankle allowing full dorsiflexion and plantar flexion. Single upright KAFOs are often used for knee instability. The single upright can be placed medially or laterally. For genu valgum, the upright is placed laterally, and medially for genu varus.
Variations exist on the basic design, and various knee locking mechanisms can be chosen. Although double metal uprights provide more stability compared with a single upright, one must consider whether the additional stability outweighs the disadvantage of added weight and bulk.
An orthosis with a free knee does not inhibit knee flexion or extension; however, stops, or mechanical devices that block motion, can be incorporated to limit ROM if required, such as after knee surgery. Variable units that allow for adjusting the orthotic knee ROM are also available.
In addition to evaluating the lower-extremity dysfunction and function the KAFO can provide, one must also consider the other functional problems and comorbidities that may be present. For instance, patients who require a high level of stability for standing and ambulating but have poor, impaired upper-extremity fine motor function would benefit from a KAFO with a bail lock for locking and unlocking the knee ( Fig. 9 ).
Stance-control knees are available. These devices lock once heel strike is achieved and release with toe-off. Typically these devices require hip extension strength of a least fair plus to extend the leg to activate the stance control.
Although total unloading of the lower extremity with a KAFO is not possible, a quadrilateral brim (ie, a plastic thigh portion that extends to the ischial tuberosity) can accept the load of weight-bearing. This device is similar to the quadrilateral socket used in a transfemoral amputation prosthesis.
Lastly, a KAFO can serve as an adjunct to exercise and other therapeutic modalities. A KAFO with a dial lock can maintain a prolonged stretch to treat a knee contracture ( Table 3 ).
| Knee joint | Function | Advantages | Disadvantages | Indications |
|---|---|---|---|---|
| Free-motion knee joint | Provides medial and lateral control and stability | Cosmetic; light weight.; permits full flexion; 180° extension stop; controls any associated genu recurvatum | Good knee extension strength required for knee control; patient must control knee flexion/extension | Unstable knee in coronal plane |
| Polycentric knee | Approximates the anatomic planes of normal knee motion; stability in coronal plane | More biomechanically correct | Weight; not cosmetic | Similar to free-motion knee joint |
| Posterior offset knee | Decreases hyperextension moment; axis of rotation posterior to knee → early extension | Mechanical knee locks before anatomic knee; increased stability from ground reaction forces | Weight; appearance is not cosmetic; not used when hip/knee contracture is present; not appropriate with plantar flexion stop | Decreases hyperextension; maximal stability |
| Drop-lock knee | Locks into place with stance (gravity-assist); knee locked in extension | Locking the knee is hands-free; no bending or use of upper extremity/hands to lock knee; durable; low maintenance | Must manually unlock knee joint; locked knee during gait leads to vaulting or circumduction | Optimal stability in standing or stance is desired |
| Trigger-lock knee | Trigger on proximal thigh allows locking without using upper extremities | No bending required to lock/unlock | Needs periodic adjustment and “tuning”; profile is bulky | Maximal stability in upright is desired |
| Lever-lock with bail release (“Cam,” “Swiss,” or “Bail Lock”) | Engages with full extension; when bail lifted, joint unlocks | Hands-free; no bending to lock/unlock; very stable | Bulky; not cosmetic; unlocks unexpectedly if bumped; bail mechanism wears clothing | Maximal stability desired; work well for persons lacking arm and hand function; useful for those who have compromised balance |
| Dial-lock knee | Allow static extension and support of the knee | Adjustment can be made in 6° increments | Difficult to ambulate; wear out, requiring replacement | Knee flexion contracture improving but requires further intervention |
| Ultraflex knee joint | Provides low-load prolonged tension for stretch | Constant stretch; tension adjustable; rate of spring tension is constant and independent of joint angle | Bulky; ambulation is difficult | |
| Stance-control knee | Provides secured knee extension with weight-bearing; unlocks with toe-off | Drop lock, bail locks are not necessary; frees up hands and upper extremities | Must have fair plus or better hip extension strength | Lower-extremity paresis or paralysis |
Hip orthosis
Hip orthoses are used for hip flexion, extension, abduction, and adduction. They are not effective for controlling hip external and internal rotation, but are frequently used after hip arthroplasty and surgical correction of the hip to control hip adduction. If control rotation at the hip is indicated, the orthosis must be converted to a hip knee ankle foot orthosis (HKAFO) to allow further control.
Hip knee ankle foot orthoses
HKAFOs controls flexion, extension, abduction, and adduction, and also hip rotation through the below-the-knee components and the foot plate. These orthoses provide maximal support of the lower extremities. They are used in cases of paraplegia from spinal cord injury, poliomyelitis, or other causes. These also allow upright standing and ambulation with a walker and swing-to or swing-through gait pattern.
Essentially an HKAFO is a KAFO with a pelvic band and hip joint added. They are heavy and cumbersome, although the advent of lighter weight materials has helped. These orthoses cause high energy consumption during gait .
A reciprocating gait orthoses is also known as a lumbosacral HKAFO with cables. The cable system couples the flexion and extension of the bilateral hips. This coupling results in extension of the contralateral hip when the other hip is flexed. A release mechanism to allow simultaneous hip flexion is incorporated. This design has been shown to decrease energy expenditure and increase ambulation speed and distance in the community .
Spinal orthotics
Spinal and cervical orthoses, like other orthoses, provide many functions, such as stabilization of a segment, protection, maintenance and correction of alignment, relief of pain, and substitution for weakness.
Cervical orthoses
The cervical spine is the most mobile part of the spinal column. C5-C6 is the site of greatest cervical flexion extension, whereas the atlantoaxial joint (C1-C2) is the location of greatest cervical rotation. In addition, the neck functions in multiple planes of flexion, extension, rotation, and lateral bending. It is a small surface area on which to purchase an external device and deliver the indicated forces for effective treatment.
Like other orthoses, spinal orthoses increase stability or function though application of external forces. The three-point force system, the practice of directing two forces in opposition to the third, is the foundation of achieving spinal control and position.
Most COs are made of metal or plastic and function primarily to immobilize the cervical spine. They also relieve pain, reduce deformity, restrict undesired motion, substitute for weak muscles, and support soft tissues and fracture healing. Spinal instability is a contraindication for a spinal orthosis, except the halo cervical thoracic orthosis, which is used selectively for cervical injury.
Prefabricated COs are available in soft or rigid designs. A soft cervical orthosis provides sensory feedback to the patient, but provide virtually no control of cervical motion.
Multiple rigid or hard cervical orthoses are commercially available. They provide some sagittal plane motion but little coronal plane control. The Philadelphia collar is an example of a reinforced rigid collar, as are the Miami J and Aspen collars ( Fig. 10 ).

To achieve better cervical control, two- or four-poster braces, which have rigid uprights, are available. In addition to the control that the uprights provide, pads are provided at the occiput, mandible, sternum, and thorax. Extensions can be added to increase control of the lower cervical spine.
Cervicothoracic orthoses
The sternal occipital mandibular orthosis (SOMI) is probably the most common prefabricated CTO. Components of this device include a shoulder unit with a sternal yoke, and mandibular and occipital pads and bars. This construction achieves adequate control in all planes, except extension. The SOMI can be used for adults and children.
To achieve triplanar control, a Halo CTO is often prescribed. The chest jacket provides the base of the orthosis, with the halo ring secured to the bone of the skull with pins. The halo, or ring, is affixed to the chest jacket with external supports or superstructure. This CTO does not cover the neck, and therefore postsurgical incisions and other wounds can be visually monitored.
Although the Halo allows some spinal snaking, this is intersegmental motion, and therefore rotational control is maintained. The Halo is commonly used for high cervical (C1, C2) spinal fractures.
A Halo orthosis provides immobilization using the long leverage of the three-point control. The skull is used as the end point of fixation. An advantage of newer Halo materials is that a Halo can be constructed of MRI-compatible materials.
Cervical orthoses are challenging to fit fabricate. These challenges include accurate fit, adequate purchase on the body, and providing the correct direction and magnitude of therapeutic forces while also considering the forces the body exerts in response. Body habitus and patient compliance can further complicate the process.
Lastly, no cervical orthosis completely eliminates cervical motion. For optimal fit and outcome, a well-trained orthotist or practitioner must fabricate and fit the orthosis. Poor fitting will not only prevent achievement of treatment goals but also may lead to further problems ( Table 4 ).
| Orthosis | Advantages | Disadvantages | Indications | Contraindications |
|---|---|---|---|---|
| Soft cervical collars | Sensory feedback reminding patient to limit motion | Provides no motion control; psychological dependency; weakness from disuse | Soft tissue injury; pain | Unstable neck injuries |
| Philadelphia CO | Prefabricated; multiple sizes; useful when weaning from a more rigid orthosis (eg, Halo CTO); kinesthetic reminder; increased immobilization can be achieved by addition of thoracic extension | C-spine rotation or lateral flexion is not controlled; controls flexion more than extension; can be hot; Aspen and Miami J orthoses may provide more stability | Stable midcervical injuries; stable single-cervical column injury; after surgical cervical spine stabilization; weaning from a rigid CTO; situations requiring only mild limitation of flexion and extension; | When chin, occiput, upper thorax, or sternum cannot tolerate pressure; unstable neck injuries |
| Hard collar | More rigid than those above; | No control of C-spine rotation | Similar to Philadelphia orthosis | Unstable injury |
| adjustable height; | pain control; | |||
| greater control of C-spine; | support weak muscles | |||
| Two- or four-poster cervical collar | Greater flexion and extension immobilization | Does not prevent rotation or lateral flexion; not for unstable spinal injury | Indicated for stable mid- and low cervical pathology; more flexion extension control than above | When mandibular or occipital pressure cannot be tolerated; unstable injury |
| SOMI | Restricts forward flexion; prefabricated; can be applied in supine positions; radiographically translucent; skin of neck visible for inspection; increased patient compliance | Poor C-spine extension control; cervical spine extension can still occur | Indicated for stable mid- to low cervical injuries, postsurgery, and arthritis; particularly useful when no posterior cervical element pathology | When mandibular or occipital pressure cannot be tolerated; unstable injury |
| HALO | Best cervical immobilization; no contact with neck and therefore allows for inspection of neck (status post-surgery or injury); increased patient compliance | Pin site infection may occur; alters center of mass → may impair balance; “snaking”; some experience dysphagia; scars at pin site | High cervical spine fractures, injury, or postsurgical repairs | Multiple skull fractures |
Thoracolumbar sacral orthoses
Treatment goals of thoracolumbar sacral dysfunctions are similar to other spinal areas: decrease motion, stabilize or correct alignment, provide pain relief, and unload structures. Several caveats must be kept in mind when prescribing a spinal orthosis. The use of an orthosis may lead to atrophy of the muscles that are put at rest. Spinal structures directly above and below the orthoses experience increased motion and forces secondary to the restriction imposed by the orthosis ( Fig. 11 ). Depending on the design of the orthosis, pulmonary function may be impacted, such as limitation of rib motion with full inspiration. Lastly, depending on the extent of spinal restriction, the patient’s balance may be impacted.

Spinal orthoses are based on a three-point force control. The pelvis is the foundation on which the orthosis is fit and alignment is achieved. Anterior compression is provided, except in hyperextension orthoses. An abdominal apron or modification of a semirigid orthosis provides abdominal compression. The anterior force is countered by a rigid posterior system ( Fig. 12 ) ( Tables 5 and 6 ).

| Orthosis | Advantages | Disadvantages | Indications |
|---|---|---|---|
| Sacroiliac belt | Limits motion; supports sacroiliac joint and pubic symphysis; lightweight; cosmetic; can be worn under clothing | Patient compliance; must be worn tightly to achieve desired support | Postpelvic fracture or pubis symphysis diastasis; control musculoskeletal pelvic or sacroiliac pain |
| Sacroiliac corset | Total contact; circumferential pelvic pressure; lightweight; can be worn under clothing; increased rigidity possible using stays in this and other corsets | Men may find unacceptable; overuse → muscle weakness; patient dependence; urinary bladder compression → potentially aggravating incontinence | Control musculoskeletal pelvic; sacroiliac strain or pain |
| Lumbosacral corset | Axial unloading of lumbar spine; compression of abdomen → increased intracavitary pressure; moves center of gravity posteriorly → decrease lordosis; total contact; circumferential pressure; can be worn under clothing; can add stays of spring steel or low-temperature plastic | Variable hold of sagittal and coronal plane; may aggravate respiratory problems in chronic obstructive pulmonary disease (COPD) and other pulmonary diseases; pendulous abdomen requires special corset as does pregnant abdomen | Alleviate low back pain; may be used during pregnancy to support abdomen and reduce lordosis (coordinate with obstetrician) |
| Thoracolumbar corset | Axial unloading of lumbar spine; compression of abdomen → increased intracavitary pressure; circumferential about torso; soft; reasonably cosmetic; can add stays | Axillary straps are uncomfortable; difficult to fit is significant spinal asymmetry; may aggravate respiratory problems in COPD and other pulmonary diseases | Kyphosis caused by osteoporosis; soft tissue injury to thoracolumbar region; limits flexion |
| Orthosis | Advantages | Disadvantages | Indications |
|---|---|---|---|
| LSO anterior posterior chairback orthosis | Limits extension; allows minimal flexion; lateral bars restrict lateral bending; stable midlevel noncompression lumbar fracture control possible | Inadequate superior and inferior leverage to control low lumbar or high lumbar fractures not indicated for compression fractures; no total contact | Low back pain; stable midlumbar fracture management; limit lumbar extension (lordosis) |
| Lumbosacral (homopolymer) plastic orthoses | Custom-fabricated; total contact; lateral control in addition to sagittal control; prefabricated designs available and are modifiable; abdominal compression → increased intracavitary pressure; hip component and hip joint that prevent extension may be added if lumbosacral immobilization needed | Axial unloading of lumbar spine; compression of abdomen → increased intracavitary pressure; no rotational control; uncomfortable in hot climate | Stable midlevel lumbar or postsurgical maintenance of fracture; back pain; off-load spinal components; can be fabricated with spine in flexion for spondylolysis and spondylolisthesis (if hip component unit added, can be used for lumbosacral control) |
| Thoracolumbar orthosis (eg, Knight Taylor orthosis) | Rigid; increased intracavitary pressure; lateral bars → lateral control; allows flexion | Axillary straps are uncomfortable; not for use with unstable fractures; do not use for thoracolumbar | Postsurgical or nonsurgical stable fracture care; severe soft tissue or muscle strain injury |
| Hyperextension orthosis (eg, Jewett or CASH) | Prevents flexion; typically low-profile | Does not control rotation; no abdominal support; poorly tolerated by patients who have kyphosis; three-point pressure system is concentrated over small area | Anterior compression fracture; osteoporosis but some designs do not provide adequate inadequate leverage to control midthoracic region; Scheuermann’s disease |
| Total-contact TLSO orthosis | Total contact → maintain alignment; triplanar control (sagittal, coronal, transverse); increase intracavitary pressure; cervical extensions can be added | Does not control for T7 or higher (use CTLSO or CTO for T7 and higher); total contact → skin problems; heat intolerance | Used to prevent rotation or unload spine to allow spine fusion to mature (eg, status post-spine fusion, kyphoplasty, spine fractures, scoliosis) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





