Chapter 37 Rehabilitation after Articular Cartilage Procedures
PRINCIPLES OF ARTICULAR CARTILAGE REHABILITATION
Several principles exist that must be considered when designing a rehabilitation program after articular cartilage repair procedures (Table 37–1). These key principles have been designed based upon the authors’ understanding of the basic science and mechanics of articular cartilage. These principles include individualization, creating a healing environment, understanding the biomechanics of the knee, reducing pain and effusion, restoring soft tissue balance, restoring muscle function, restoring proprioception and neuromuscular control, controlling the application of loads, and team communication. Each of these principles is briefly described as they relate to the rehabilitation program after articular cartilage repair procedures.
TABLE 37-1 Key Principles to Consider when Designing Rehabilitation Programs after Articular Cartilage Repair Procedures
Critical Points PRINCIPLES OF ARTICULAR CARTILAGE REHABILITATION
Individualization
Create a Healing Environment
Biomechanics of the Knee
Reduce Pain and Effusion
Restore Soft Tissue Balance
Restore Muscle Function
Control the Application of Loads
Individualization
One of the most important principles involving rehabilitation after articular cartilage repair procedures is the need for an individualized approach for each patient. Several variables must be considered when developing a unique rehabilitation progression for each patient. These include specifics regarding the patient, lesion, and surgery (Table 37–2).
TABLE 37-2 Specific Variables that Must be Considered when Designing Postoperative Rehabilitation Protocols after Articular Cartilage Procedures
| Lesion specifics | |
| Patient specifics | |
| Surgical specifics |
The quality of each individual’s articular cartilage is the result of several factors including age, BMI, general health, nutrition, history of previous injuries, and genetics. The composition of articular cartilage undergoes a gradual degeneration over time that results in a breakdown of tissue matrix and a reduction in the load-bearing capacity of the cartilage.8 The specific factors that contribute to this deterioration remain controversial, but it appears that age, obesity, poor nutrition, and a history of repetitive impact loading (through work or sport activities) may result in osteoarthritic changes.8 Thus, younger patients with isolated defects and relatively healthy surrounding articular cartilage will progress more rapidly than older individuals with more degenerative changes and less dense cartilage structure. Furthermore, the patient’s motivation and previous activity levels must be considered when determining the rehabilitation approach to ensure that the goals of each patient are addressed. The rehabilitation program should be individualized to the specific demands of each patient’s activities of daily living, work, and/or sport activities.
BMI is another factor to consider. Mithoefer and coworkers30 reported a correlation between BMI and outcomes after microfracture, because the greater the BMI, the more likely the clinical outcome would be less favorable.
Create a Healing Environment
The next principle of articular cartilage rehabilitation involves creating an environment that facilitates the healing process while avoiding potentially deleterious forces to the repair site. This involves a thorough knowledge of the physiologic repair process after surgery. Through animal studies, as well as closely monitoring the maturation of repair tissue in human patients via arthroscopic examination, the biologic phases of maturation have been identified after several articular cartilage repair procedures.4,5,16,36,38 Knowledge of the healing and maturation process after these procedures will ensure that the repair tissue is gradually loaded and that excessive forces are not introduced too early in the healing process. These are discussed in detail in regard to each specific surgical procedure.
Two of the most important modes of rehabilitation of articular cartilage procedures are weight-bearing restrictions and range of motion (ROM) limitations. Unloading and immobilization have been shown to be deleterious to healing articular cartilage, resulting in proteoglycan loss and gradual weakening.2,17,50 Therefore, controlled weight-bearing and ROM are essential to facilitate healing and prevent degeneration. This gradual progression has been shown to stimulate matrix production and improve the tissue’s mechanical properties.6,7,51
Controlled compression and decompression forces observed during weight-bearing may nourish the articular cartilage and provide the necessary signals to the repair tissue to produce a matrix that will match the environmental forces.2,17,50 A progression of partial weight-bearing with crutches is used to gradually increase the amount of load applied to the weight-bearing surfaces of the joint. The use of a pool or aquatic therapy may also be beneficial to initiate gait training and lower extremity weight-bearing exercises. The buoyancy of the water has been shown to decrease the amount of weight-bearing forces to approximately 25% of the individual’s body weight when submerged to the level of the axilla and 50% of the individual’s body weight when submerged to the level of the waist.20 Commercially available devices to unload the patient’s body weight during treadmill ambulation may also be useful.
A force platform is another useful tool during the early phases of rehabilitation when weight-bearing is limited. This can be used to monitor the percentage of weight-bearing on each extremity during closed kinetic chain (CKC) exercises such as weight-shifts, mini-squats, and leg press (Fig. 37–1).
Passive range of motion (PROM) activities, such as continuous passive motion (CPM) machines or manual PROM, performed by a rehabilitation specialist are also begun immediately after surgery in a limited ROM to nourish the healing articular cartilage and prevent the formation of adhesions. Motion exercises may assist in creating a smooth low-frictional surface by sliding against the joint’s articular surface and may be an essential component in cartilage repair.44,45 The authors’ opinion is that PROM is a safe and effective exercise to perform immediately postoperatively, with minimal disadvantageous shear or compressive forces, if done with patient relaxation. This ensures that muscular contraction does not create deleterious compressive or shearing forces. Furthermore, the use of CPM has been shown to enhance cartilage healing and long-term outcomes after articular cartilage procedures.41,42 In a study comparing the outcomes of patients after microfracture procedures, Rodrigo and associates41 reported an 85% satisfactory outcome in patients who used a CPM machine for 6 to 8 hours per day for 8 weeks as compared with a 55% satisfactory outcome in patients who did not use a CPM machine. PROM may also be performed on an isokinetic device (Biodex Corporation, Shirley, NY) in the passive mode or with a bike with adjustable pedals that can alter the available ROM (Unicam Corporation, Ramsey, NJ) (Fig. 37–2). The authors advocate low-intensity (light-resistance) bicycling for long duration to stimulate articular cartilage regeneration.
Biomechanics of the Knee
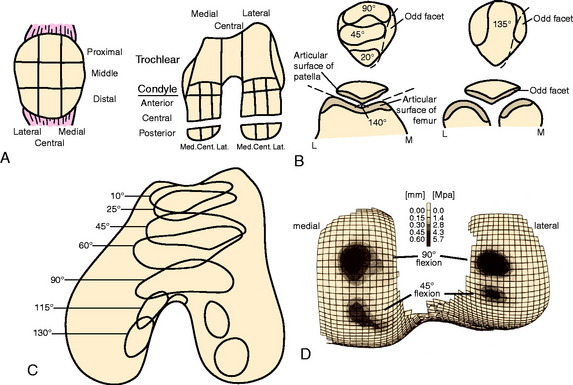
The next rehabilitation principle involves the biomechanics of the tibiofemoral and patellofemoral joints during normal joint articulation. Articulation between the femoral condyle and the tibial plateau is constant throughout knee ROM. The anterior surface of each femoral condyle is in articulation with the middle aspect of the tibial plateau near full knee extension. With weight-bearing, as the knee moves into greater degrees of knee flexion, the femoral condyles progressively roll posteriorly and slide anteriorly causing the articulation to shift posteriorly on the femoral condyle and tibial plateaus.24,28
The articulation between the inferior margin of the patella and the trochlea begins at approximately 10° to 20° of knee flexion depending on the size of the patella and the length of the patella tendon.23 As the knee proceeds into greater degrees of flexion, the contact area of the patellofemoral joint moves proximally along the patella. At 30°, the area of patellofemoral contact (inferior facets) is approximately 2 cm2.23 The area of contact gradually increases as the knee is flexed. At 60° of knee flexion, the middle facets of the patella articulate with the trochlea. At 90° of knee flexion, the contact area increases up to 6 cm2 and the superior facets articulate.23
Using this knowledge of joint arthrokinematics, the rate of weight-bearing, PROM, and exercise progression may be based on the exact location of the lesion (Fig. 37–3).3,12,14,15 For example, a patient with a lesion on the anterior aspect of the femoral condyle may perform exercises into deeper degrees of knee flexion without causing articulation at the repair site. Conversely, lesions on the posterior condyle may require the avoidance of exercise in deep knee flexion owing to the rolling and sliding component of the articulation during deeper knee flexion. Furthermore, the rehabilitation program for lesions on a non–weight-bearing surface, such as the trochlea, may include immediate partial weight-bearing with a brace locked in full knee extension without causing excessive compression on the repair site.
Rehabilitation exercises are altered based on the biomechanics of the knee to avoid excessive compressive or shearing forces. Whereas the exact ROM in which articulation of the lesion occurs is the most important factor to consider when designing the rehabilitation program, the amount of compressive and shear forces observed at the joint also vary throughout the ROM. Open kinetic chain (OKC) exercises, such as knee extension, are commonly performed from 90° to 40° of knee flexion. This ROM provides the lowest amount of patellofemoral joint reaction forces while exhibiting the greatest amount of patellofemoral contact area,22,23,49 thus distributing the force along a greater surface area. CKC exercises such as the leg press, vertical squats, lateral step-ups, and wall-squats are performed initially from 0° to 30° and then progressed to 0° to 60° where tibiofemoral and patellofemoral joint reaction forces are lowered.22,23,49 Clinically, these exercises are begun using a leg press machine rather than the vertical mini-squat owing to the ability to control the amount of weight applied to the lower extremities in the horizontal position in comparison with the vertical squat. As the repair site heals and symptoms subside, the ROM in which exercises are performed is progressed to allow greater muscle strengthening in a larger arc of motion. Exercises are progressed based on the patient’s symptoms and the clinical assessment of swelling and crepitation.
Reduce Pain and Effusion
Numerous authors have studied the effect of pain and joint effusion on muscle inhibition. A progressive decrease in volitional quadriceps activity has been noted as the knee exhibits increased pain and distention.48,52 Therefore, the reduction in knee joint pain and swelling is crucial to minimize this reflexive inhibition and restore normal quadriceps activity. Furthermore, any increase in intra-articular joint temperature has been shown to stimulate proteoglytic enzyme activity, which has a detrimental effect on articular cartilage.21,34
Treatment options for swelling reduction include cryotherapy, elevation, high-voltage stimulation, and joint compression through the use of a knee sleeve or compression wrap (Fig. 37–4). Patients presenting with chronic joint effusion may also benefit from a knee sleeve or compression wrap to apply constant pressure while performing everyday activities in an attempt to minimize the development of further effusion (Fig. 37–5).
Pain can be reduced passively through the use of cryotherapy, transcutaneous electrical nerve stimulation, and analgesic medication. Immediately after injury or surgery, the use of a commercial cold wrap can be extremely beneficial. PROM may also provide neuromodulation of pain during acute or exacerbated conditions.43
Restore Soft Tissue Balance
One of the most important aspects of articular cartilage rehabilitation involves the avoidance of arthrofibrosis, particularly with the OATS and ACI procedures, owing to the large open incision and extensive soft tissue trauma. This is achieved through the restoration of full passive knee extension, patellar mobility, and soft tissue flexibility of the knee and entire lower extremity. The inability to fully extend the knee results in abnormal joint arthrokinematics and subsequent increases in patellofemoral and tibiofemoral joint contact pressure, increased strain on the quadriceps muscle, and muscular fatigue.35 Therefore, a drop-lock postoperative knee brace locked into 0° of extension is used during ambulation, and PROM out of the brace is performed immediately after surgery.
The goal is to achieve at least 0° of knee extension within the first few days after surgery. Specific exercises include manual PROM exercises performed by the rehabilitation specialist, supine hamstring stretches with a wedge under the heel, and gastrocnemius stretching with a towel. Overpressure of 6 to 12 pounds may be used for a low-load long-duration stretch as needed to achieve full extension (Fig. 37–6). Patients are instructed to perform low, long-duration stretches for 10 to 12 minutes several times each day (usually five to six times per day). Modalities such as moist heat and ultrasound may also be applied to facilitate greater ROM improvements before and/or during these stretching techniques.25,40
Restore Muscle Function
The next principle involves restoring muscle function of the lower extremity. As previously stated, inhibition of the quadriceps muscle is a common clinical enigma in the presence of pain and effusion during the acute phases of rehabilitation. Electrical muscle stimulation (EMS) and biofeedback are often incorporated with therapeutic exercises to facilitate the active contraction of the quadriceps musculature (Fig. 37–7A).
EMS and biofeedback on the quadriceps musculature appear to facilitate the return of muscle activation and may be valuable additions to therapeutic exercises.9,46 Clinically, EMS is begun immediately after surgery while the patient performs isometric and isotonic exercises such as quadriceps sets, straight leg raises, hip adduction and abduction, and knee extensions (see Fig. 37–7B). EMS is used before biofeedback when the patient presents acutely with the inability to activate the quadriceps musculature. EMS is useful to attempt to recruit a maximum amount of muscle fibers during active contraction and may be used throughout the rehabilitation process. Once independent muscle activation is present, biofeedback may also be incorporated to facilitate further neuromuscular activation of the quadriceps. The patient must concentrate on neuromuscular control to independently activate the quadriceps during rehabilitation. The quadriceps and the hip/core muscles are emphasized to assist in dissipating ground reaction forces.
Enhance Proprioception and Neuromuscular Control
Proprioceptive and neuromuscular control drills of the lower extremities should be included to restore dynamic stabilization of the knee joint postoperatively. Proprioceptive deficits have been noted in the injured and postoperative knee.10,39 Specific drills initially include weight-shifting side-to-side, weight-shifting diagonally, mini-squats, and mini-squats on an unstable surface such as a tilt board (Fig. 37–8). Perturbations can be added to challenge the neuromuscular system as well as additional exercises including lunges, step-ups, and balance onto unstable surfaces (Figs. 37–9 and 37–10).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree