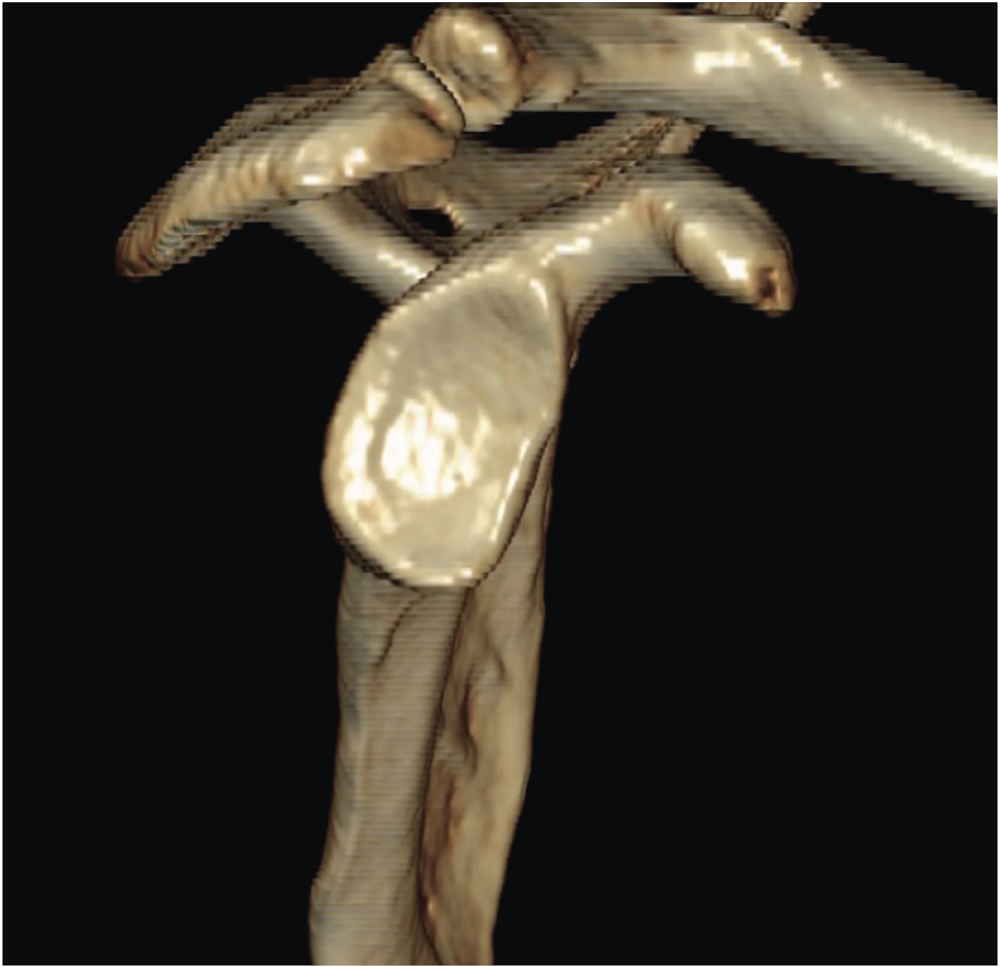
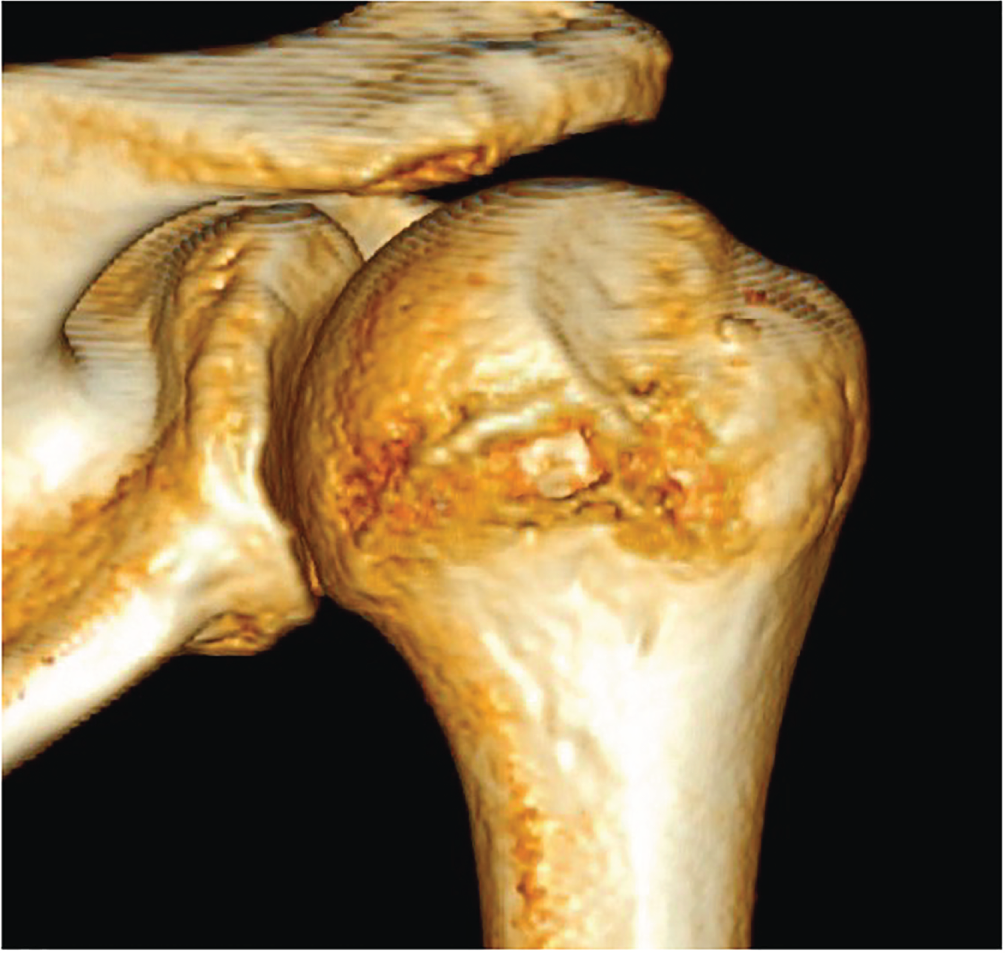
Joost I. P. Willems MD1, Amber von Gerhardt MD1, W. Jaap Willems MD2 and Arthur van Noort MD PhD1 1 Department of Orthopaedic Surgery, Spaarne Gasthuis, Hoofddorp, The Netherlands 2 Lairesse Kliniek, Amsterdam, The Netherlands Figure 122.1 CT scan of the right shoulder, with erosion of the anterior glenoid. Source: Joost I. P. Williams, Amber von Gerhardt, W. Jaap Willems, Arthur van Noort. Figure 122.2 CT scan of the humeral head, showing a Hill–Sachs defect on the posterolateral part of the humeral head. Source: Joost I. P. Williams, Amber von Gerhardt, W. Jaap Willems, Arthur van Noort. Historically, an open or arthroscopic labrum repair is the gold standard for treating recurrent anterior instability, but long‐term follow‐up studies have shown that the rate of recurrence is rather high. Bony procedures seem to show better long‐term results with lower recurrence rates, but at the expense of greater number of complications.1 Labrum repair is nowadays mostly performed arthroscopically and is a procedure with low morbidity but high recurrence in cases with considerable bone loss. The bony procedures, of which the Latarjet is the most popular, are a more difficult operation with potentially less recurrence, but with a higher complication rate. In a recent systematic review, including seven studies of level III and one study of level II, 795 patients were evaluated of which 416 underwent an open or arthroscopic Bankart repair and 397 an open Latarjet procedure with a mean range of follow‐up of 4.9 to 17.5 years. None of these studies reported on the preoperative bone loss. Latarjet procedure leads to less recurrence and less revision surgery, with no higher complication rate leading to reoperation.2 In another recent systematic review with a minimum follow‐up of five years, arthroscopic (n = 336) and open Bankart (n = 632), as well as open Latarjet repairs (n = 684), were evaluated. Recurrence rates were respectively 15.1, 7.7, and 2.7%. Only the difference between arthroscopic Bankart repair and Latarjet was statistically significant. Complication rates were higher in Latarjet repair (9.4% vs 0%) in the arthroscopic Bankart repair (p = 0.002).1 One level III study,3 comparing arthroscopic Bankart versus open Latarjet with a minimum follow‐up of six years, showed superior results for the Latarjet procedure regarding any type of recurrent instability (positive apprehension, subluxation, dislocation) (41% vs 11% respectively, p = 0.0001). Small bone lesions were operated by Bankart repair, larger bone defects with a Latarjet. Revision surgery was more frequent in the Bankart repair group (21% vs 5.3%, p = 0.0001). In two studies, Bankart repair combined with remplissage was compared with Latarjet procedure in patients with considerable Hill–Sachs lesions.4,5 Both were retrospective level III studies. With a follow‐up of both studies varying between two and four years, the recurrence rate was not significantly different. In one study the rate of complications was higher in the Latarjet group; in the other study, the patients with Bankart plus remplissage showed more pain and loss of external rotation. Apart from the bony lesions, other clinical factors play a significant role in predicting the chance of recurrence after arthroscopic Bankart repair, especially for those aged <22, male, with a number of preoperative dislocations who participate in competitive sports.6 There is moderate evidence, that labrum repair alone (Bankart repair) is inferior to the Latarjet procedure in recurrent instability. No high‐level evidence data are available if, in minor bony erosions of the glenoid, the labrum repair alone is as effective in preventing recurrence compared to the Latarjet procedure. A randomized controlled trial would be helpful. Following the data at present, with a higher recurrence after labral repair in undefined bone lesions, it is probable, that the Latarjet procedure is superior whenever there is a bone lesion.
122 Recurrent Shoulder Instability
Clinical scenario
Top three questions
Question 1: In patients with recurrent post‐traumatic anterior shoulder instability with a bony defect, does a bony procedure lead to less recurrent instability in comparison to a labrum repair alone?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Resolution of clinical scenario
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





