CHAPTER 39 Recurrent instability due to capsular deficiency
 Understand the common causes of capsular deficiency: (1) multiple failed prior surgeries, (2) previous thermal capsulorrhaphy resulting in tissue necrosis, and (3) hereditary collagen disorders.
Understand the common causes of capsular deficiency: (1) multiple failed prior surgeries, (2) previous thermal capsulorrhaphy resulting in tissue necrosis, and (3) hereditary collagen disorders. Patients with recurrent instability with capsular deficiency tend to lack the anterior labrum, middle glenohumeral ligament (MGHL), and anterior band of the inferior glenohumeral ligament (IGHL).
Patients with recurrent instability with capsular deficiency tend to lack the anterior labrum, middle glenohumeral ligament (MGHL), and anterior band of the inferior glenohumeral ligament (IGHL). Identifying the cause of failed shoulder stabilization procedures is imperative in producing a successful revision procedure.
Identifying the cause of failed shoulder stabilization procedures is imperative in producing a successful revision procedure. Allograft capsulolabral reconstruction is a salvage procedure for patients with a deficient capsulolabral complex without associated bone loss.
Allograft capsulolabral reconstruction is a salvage procedure for patients with a deficient capsulolabral complex without associated bone loss.Introduction
In the presence of bone loss, further complexity is present because of a lack of articular congruity between the humerus (Hill-Sachs lesion) and glenoid (bony Bankart lesion). In this setting, conventional soft tissue procedures have been met with high failure rates, especially in the contact athlete.1,2 However, bone grafting and bone transfer (Bristow, Latarjet) procedures designed to address bony deficiency have produced better results and lower recurrence rates.3,4
The less commonly encountered, but equally demanding problem of capsular insufficiency is one of the toughest challenges in the surgical management of glenohumeral instability.5,6 These patients have an attenuated or absent glenohumeral capsule that compromises repair efforts because of inadequate or poor-quality capsular and labral tissue. Capsular attrition in this population may be attributed to three possible etiologic factors: (1) multiple failed prior surgeries, (2) previous thermal capsulorrhaphy resulting in tissue necrosis, or (3) hereditary collagen disorders.
Recurrence of instability is related to the number of prior surgeries. Deficiency of reinforcing structures such as the subscapularis, capsule, and glenohumeral ligaments (the middle glenohumeral ligament [MGHL] and the anterior band of the inferior glenohumeral ligament [IGHL]) is often noted after multiple surgical attempts to stabilize the joint.7–13 The absence or attenuation of these structures in the revision setting is largely responsible for the suboptimal results seen in this population.
In addition to chondrolysis, irreversible damage to the capsule has been documented with the use of thermal capsulorrhaphy. Second-look arthroscopies have shown the joint capsule to be thin and attenuated in many instances while also exhibiting qualities of thermal necrosis in the most severe cases.13,14 Histologic examination also has shown alterations in tissue characteristics, with specimens exhibiting increased cellularity and apoptosis, increased vascularity, and hyalinization.15–18
When repair of the capsulolabral complex is not a possible option because of insufficiency of the aforementioned structures, reconstruction of the capsule and labrum is a viable option. Several surgical techniques, both anatomic19,20 and nonanatomic21 have been described to address the reconstruction of the anterior glenohumeral capsule and ligaments as a salvage procedure for end-stage shoulder instability. Glenohumeral capsule augmentation and reconstruction have been illustrated using autogenous hamstring or long head of the biceps tendon, autogenous iliotibial band, and reconstruction using Achilles, tibialis anterior, and hamstring allografts.19,20,22,23
Studies have shown dramatically increased failure rates of up to 44% in the setting of multiple revision stabilizations.24 Capsular tearing and progression to insufficiency have long been understood as major factors in recurrent instability.25
The treatment of recurrent shoulder instability in the setting of anterior soft tissue deficiency in young and active patients continues to be challenging. For patients with both pain and instability who have failed standard open and arthroscopic attempts to correct their pathology, few palatable options remain. Glenohumeral arthrodesis is the definitive answer to such end-stage instability, but many young patients remain unwilling to accept the associated sacrifice of shoulder motion. Furthermore, Richards et al26 described the unexpected complication in their series of glenohumeral arthrodeses of continued sensations of instability despite radiographic evidence of a solid fusion. Subsequently, there has been a continued interest in alternative salvage procedures that preserve glenohumeral motion and stabilize the shoulder by soft tissue reconstruction techniques.
The first reported cases of anterior capsular reconstruction are attributed to Gallie et al21 who eloquently described the natural history of recurrent anterior shoulder instability and their use of fascia lata graft to augment the capsule in a nonanatomic fashion. They reported only 7 failures in their series of 175, including 80 armed forces personnel. Subsequently, Lazarus et al27 showed 70% success in resolving recurrent instability using semitendinosus autograft in a series of 25 patients. Warner et al28 reported two successful cases of autograft hamstring capsular reconstruction.
Moeckel et al29 described the successful application of Achilles allograft augmentation in the setting of unstable shoulder replacements. Iannotti et al30 reported treating a series of 7 patients with instability but without significant bone loss with an iliotibial band graft placed in a Z-pattern to recreate the anterior capsule, middle glenohumeral, and anterior inferior glenohumeral ligaments (Fig. 39-1). American Shoulder and Elbow Surgeons (ASES) scores improved from a mean preoperative score of 30 to mean postoperative score of 55. There were no failures in their series at a mean follow-up of almost 4 years.
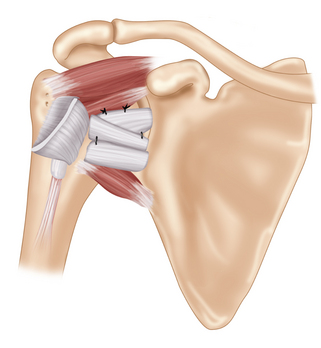
(Modified from Iannotti JP et al: Iliotibial band reconstruction for treatment of glenohumeral instability associated with irreparable capsular deficiency. J Shoulder Elbow Surg 11(6):618–623, 2002.)
Alcid et al31 recently reported a series of patients who underwent hamstring autograft and tibialis anterior allograft anterior capsular reconstruction. Their technique involves placing four limbs of graft material across the anterior shoulder joint (Fig. 39-2). Just over half of their patients had capsular deficiency from previous thermal capsular shrinkage and reported a mean 2.1 previous surgeries. The study showed no difference in satisfaction or postoperative ASES scores between patients receiving allograft versus autograft. Clinical failure in two patients was attributed to accelerated glenohumeral arthritis requiring total shoulder arthroplasty. Although no patients reported recurrent dislocation, one third had symptomatic recurrent subluxations, but remained satisfied with their surgery.
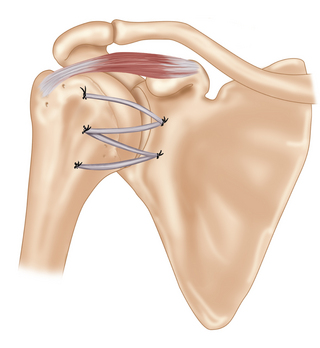
(Modified from Alcid JG et al: Revision anterior capsular shoulder stabilization using hamstring tendon autograft and tibialis tendon allograft reinforcement: minimum two-year follow-up. J Shoulder Elbow Surg 16(3):268–272, 2007.)
We present here our reconstructive technique for using tibialis anterior tendon allograft to reconstruct the main stabilizing structures of the anterior labrum, the middle glenohumeral ligament, and the anterior band of the inferior glenohumeral ligament. Our reconstruction technique is applicable in the setting of anterior soft tissue deficiency and allows for precise placement and tensioning of the allograft tendon to restore stability to the deficient glenohumeral joint. This allograft reconstruction should be viewed as an adjunct to a properly tensioned inferior capsular shift to ensure biologic healing and sustainable results after reconstruction. This procedure is designed to provide the surgeon with an alternative to more aggressive and invasive techniques such as glenohumeral arthrodesis.32
Pearls
Anatomy
The functional range of motion of the hand and upper extremity place a unique demand on the shoulder, specifically the glenohumeral joint, to provide stability without restricting mobility. A multitude of structures provides stability and restraint in various shoulder positions.33,34
Translation normally occurs between the humeral head and the glenoid. The degree of glenohumeral translation defines laxity and instability.26,35 However, laxity varies among individuals and is an important variable that must be assessed as part of the clinical evaluation to differentiate a normal versus pathologic condition.37
The shoulder joint is an inherently unstable articulation owing to the shallow glenoid articular surface and lack of bony congruency. Stability to the shoulder is conferred by both active and passive stabilizers.38,39 The rotator cuff muscles and other periscapular muscles confer the bulk of active or dynamic stability. Static stability is derived from the bony geometry of the glenoid and labrum, intra-articular pressure, the glenohumeral ligaments, and the joint capsule, in addition to other accessory ligaments.
The glenoid labrum acts as a static restraint by adding depth and concavity to the joint. This shape provides stability in both the anterior-posterior and superior-inferior directions. The labrum has been noted to account for as much as 50% of the socket depth and is an important structure in providing stability.40
Anatomic dissection studies of the shoulder define the glenohumeral ligaments as discreet thickenings of the joint capsule.41 However, individual variability exists in how well each of these ligaments develops.42 Four major structures are found to exist within the glenohumeral capsule: the coracohumeral ligament (CHL), superior glenohumeral ligament (SGHL), MGHL, and the IGHL.
The CHL spans from the base of the coracoid process laterally and downward to the greater and lesser tuberosities as two distinct bands. The CHL is considered a restraint to anteroinferior translation and external rotation in an adducted position.36,43
The SGHL originates at the anterosuperior rim of the glenoid, anterior to the biceps tendon, and attaches to the lesser tuberosity adjacent to the bicipital groove. Because this ligament tends to parallel the path of the CHL, it has a similar function as well. It is a primary restraint to inferior translation and external rotation in the adducted position.36,43
The MGHL is observed to be highly variable in nature and is absent in as many as 30% of cases.41 The MGHL originates at the upper third of the glenoid rim and attaches to the lesser tuberosity. It is described as a critical stabilizer to anterior translation in cases where it is present (in the abducted arm up to 45 degrees). At a position of 90 degrees of abduction, the MGHL was found to shorten and be less active as a restraint to anterior translation.41,44 It is also an important restraint to external rotation when the arm is abducted past 60 degrees.43,45
The IGHL consists of an anterior and posterior band. The anterior band originates between the 2- and 4-o’clock positions on the glenoid while the posterior attachment is between the 7- and 9-o’clock positions. Between the two bands lies an axillary pouch that acts as a hammock to support the humeral head.44 The IGHL complex is cited as the primary restraint to anterior and posterior translation with the arm abducted above 60 degrees. With external rotation, the anterior band becomes taut and is positioned in a more anterior position to resist anterior translation in the abducted shoulder. Similarly with internal rotation, the posterior band is under tension and oriented more posteriorly to better resist posterior translation.43,45
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









