CHAPTER 33 Reconstructive surgery
Surgical decision making
Assessment of the wound
Causative factors.
What caused the wound? Is the wound acute or chronic? Acute traumatic wounds may be missing fragments of skin, but with removal of these devitalized tissues and mobilization of surrounding skin, the laceration may be closed primarily. If the wound is chronic, can the factors contributing to the chronic nature of the wound be corrected? The underlying etiology of the wound must be corrected or minimized (e.g., pressure) and cofactors treated (e.g., infection, malnutrition) before healing can ensue. For example, the wound complicated by an ischemic process will require improvement of blood flow in order to heal. Likewise, an ischial pressure ulcer will not heal if the patient continues to sit on the ulcer. Surgical reconstruction of wounds in which the causative factor has not been addressed is not likely to succeed (Franz et al, 2008; WOCN 2010).
Selection of wound closure method
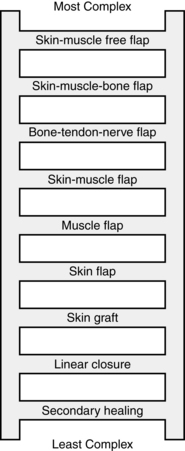
Selecting a method of closure depends on a holistic assessment that considers the needs and goals of the patient. A common set of decision-making steps (e.g., the reconstructive ladder) serves as a guide for plastic and reconstructive surgery (Figure 33-1). The simplest method that accomplishes the patient’s goals usually is the first choice. In addition to the complexity of the surgery, consideration is given to the morbidity that would be created for the donor site. For example, if a person lost a thumb, transplantation of the great toe to replace the thumb would be considered; however, the thumb would not be used to replace a great toe.
Skin grafts provide superficial coverage but do not replace deeper tissue layers, such as subcutaneous tissue and muscle; thus they are unable to provide the padding needed to protect bony prominences from recurrent breakdown. Therefore, skin grafts are rarely, if ever, used in the surgical management of pressure ulcers, except to close donor sites from flaps containing multiple layers of tissue. Skin grafts are commonly used to manage burn wounds and are described in greater detail in Chapter 32. Skin grafts have also been used in the management of venous ulcers (Robson et al, 2006).
Skin substitutes can be used to close a wound. The skin substitute can be epidermis only, dermis only, or both. Epidermal skin substitutes are composed of keratinocytes, take 2 to 3 weeks to “grow,” and are generally used when the patient does not have sufficient healthy skin graft donor sites available. Dermal substitutes are composed of fibroblasts embedded in a “matrix” material that provides a scaffolding for cellular and capillaries migration. Epidermal replacements and extracellular matrix scaffolds are discussed in Chapter 19.
Tissue flaps
Local flaps are most commonly used for pressure ulcers (WOCN, 2010). They are categorized by the anatomic structures they encompass, the method used to move the flap, or the method used to perfuse the flap (Box 33-1).
Methods of retaining perfusion
The perfusion of the flap is important in the design of the flap. All flaps of tissue carry with them a blood supply (unlike a skin graft). Random flaps depend on the dermal and subdermal vessels for their blood supply. Because these vessels are small, the blood supply to these flaps is tenuous. Axial flaps are designed to include an artery, which increases vascularity and the chances for flap survival. These vessels nourish the flap until new collateral capillary systems are established between the flap and the wound bed. Common axial flaps include the pectoralis flap to reconstruct the neck following radical neck surgery and the tensor fascia lata flap used to close ischial pressure ulcers. When tissue is not available locally, it can sometimes be brought in using a free flap. This type of operation is performed less commonly because it requires microvascular surgical techniques. In this approach, the donor tissue along with its blood supply is completely removed from the donor site and transferred to the recipient site. The artery and vein that supply the flap are attached by microvascular techniques to vessels near the wound. These types of flaps can be used to repair wounds of the head and neck, breast, or lower third of the leg. For example, recalcitrant venous ulcers with severe lipodermatosclerosis may benefit from free flap transfer by allowing wide excision of diseased tissue and replacing it with healthy tissue with its own microvasculature and uninjured venous valves (Robson et al, 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree