Radial Head Replacement
Yishai Rosenblatt
Graham J. W. King
DEFINITION
Radial head fractures are the most common fracture of the elbow and usually can be managed either nonoperatively or with open reduction and internal fixation (ORIF).12
Radial head arthroplasty is indicated for unreconstructable displaced radial head fractures with an associated elbow dislocation or a known or possible disruption of the medial collateral, lateral collateral, or interosseous ligaments.26
Most comminuted radial head fractures have an associated ligament injury, so radial head excision without replacement is uncommonly indicated in the setting of an acute radial head fracture.
Biomechanical studies have shown that the kinematics and stability of the elbow are altered by radial head excision, even in the setting of intact collateral ligaments,24 and are improved with a metallic radial head arthroplasty.6,31,39
Radial head replacement is also indicated to treat posttraumatic conditions such as radial head nonunion and malunion and to manage elbow or forearm instability after radial head excision.41
ANATOMY
The radial head has a circular concave dish that articulates with the spherical capitellum and an articular margin that articulates with the lesser sigmoid notch of the ulna.
The articular dish has an elliptical shape that varies considerably in size and shape and is variably offset from the axis of the radial neck.44
There is a poor correlation between the size of the radial head and the medullary canal of the radial neck, making a modular implant desirable for an optimal fit.30
Elbow stability is maintained by joint congruity, capsuloligamentous integrity, and an intact balanced musculature.
The radial head is an important valgus stabilizer of the elbow, particularly in the setting of an incompetent medial collateral ligament, which is the primary stabilizer against valgus force.
The radial head is also important as an axial stabilizer of the forearm and resists varus and posterolateral rotatory instability by tensioning the lateral collateral ligament.25
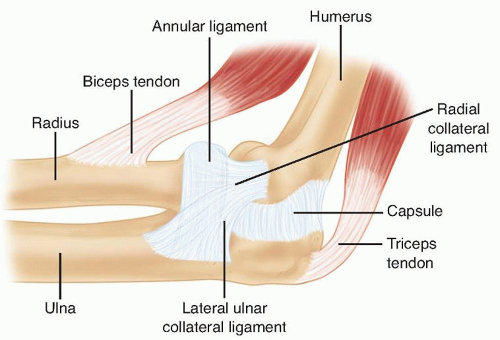
The lateral ulnar collateral ligament is an important stabilizer against varus and posterolateral rotational instability of the elbow37 and should be preserved or repaired after radial head arthroplasty (FIG 1).
The radial head accounts for up to 60% of the load transfer across the elbow.19
PATHOGENESIS
Displaced radial head fractures typically result from a fall on the outstretched arm.
Axial, valgus, and posterolateral rotational patterns of loading are all thought to be potentially responsible for these fractures.
Injuries of the medial collateral or lateral collateral ligament or the interosseous ligament are typically associated with comminuted displaced unreconstructable radial head fractures.9
In more severe injuries, dislocations of the elbow and forearm and fractures of the coronoid, olecranon, and capitellum can occur and further impair stability.
NATURAL HISTORY
Long-term follow-up studies suggest a high incidence of radiographic arthritis with radial head excision, although the incidence of symptomatic arthritis varies widely between series.7,22,23
Biomechanical data have demonstrated an alteration in the kinematics, load transfer, and stability of the elbow after radial head excision6,24 that may lead to premature cartilage wear of the ulnohumeral joint and secondary pain due to arthritis.
Metallic radial head replacement in elbows with intact ligaments restores the kinematics and stability similar to that of a native radial head and has been shown to provide good clinical and radiographic outcome in most patients at medium-term follow-up; however, long-term outcome studies are lacking.6
PATIENT HISTORY AND PHYSICAL FINDINGS
The mechanism of injury is typically a fall on the outstretched hand.
The patient will complain of pain and limitation of elbow or forearm motion.
A history of forearm or wrist pain should be sought.
Inspection may reveal ecchymosis along the forearm or medial aspect of the elbow. Deformity may be evident if there is an associated dislocation.
Careful palpation of the radial head, the medial and lateral collateral ligaments of the elbow, the interosseous ligament of the forearm, and the distal radioulnar joint should be performed. Local tenderness over one or all of these structures implies a possible derangement of the relevant structure.
Because associated injuries of the shoulder, forearm, wrist, and hand are common, these areas should be carefully examined.
Range of motion, including forearm rotation and elbow flexion-extension, should be evaluated. The presence of palpable and auditory crepitus should be noted.
Loss of terminal elbow flexion and extension is expected as a consequence of a hemarthrosis in acute fractures, whereas loss of forearm rotation typically is caused by a mechanical impingement.
A careful neurovascular assessment of all three major nerves that cross the elbow should be performed.
The examiner should observe for localized or diffuse swelling in the elbow. Effusion represents hemarthrosis due to intra-articular fracture.
The examiner should compare active and passive range of motion to the uninjured side. Reduced range of motion may be a result of hemarthrosis or mechanical block from a broken fragment. Intra-articular injection of a local anesthetic helps differentiate between reduced range of motion due to a mechanical block versus pain inhibition.
The examiner should look for varus-valgus instability. Any gapping on the medial or lateral side beneath the examiner’s hand is noted. Positive findings suggest medial or lateral collateral ligament insufficiency. Typically, this test is positive only when performed under a regional or general anesthetic, hence these injuries are easy to miss if an examination under anesthesia is not performed.
The lateral pivot shift test is performed. Positive apprehension or a clunk that is seen or felt when the ulna and radius reduce on the humerus suggests posterolateral rotatory instability.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and oblique elbow radiographs, with the x-ray beam centered on the radiocapitellar joint, usually provide sufficient information for the diagnosis and treatment of radial head fractures.
Bilateral posteroanterior radiographs of both wrists in neutral rotation should be performed to evaluate ulnar variance in patients with wrist discomfort or a comminuted radial head fracture because there is a higher incidence of an associated interosseous ligament injury in these patients.9
Computed tomography with sagittal, coronal, and three-dimensional (3-D) reconstructions may assist with preoperative planning and can help the surgeon predict whether a displaced radial head fracture can be repaired with ORIF or if an arthroplasty will likely be needed.
DIFFERENTIAL DIAGNOSIS
Acute radial head fractures
Other fractures or dislocations about the elbow (eg, supracondylar, capitellar, coronoid, osteochondral fractures)
Radial head nonunion or malunion, posttraumatic arthritis
Congenital dislocation of the radial head
Forearm or elbow instability
Lateral epicondylitis
Rheumatoid arthritis or osteoarthritis
Synovitis, inflammatory or infectious
Tumors
NONOPERATIVE MANAGEMENT
The indications for surgical management of radial head fractures are not well defined in the literature. Fragment size, number of fracture fragments, degree of displacement, and bone quality influence decision making regarding the optimal management.
Nondisplaced fractures or small (<33% of the radial head) minimally displaced fractures (<2 mm of displacement) can be treated with early motion with an excellent outcome in the majority of patients.21
Associated injuries and a block to motion are also important factors to consider when deciding between nonoperative and surgical management.
SURGICAL MANAGEMENT
Small displaced fractures that cause painful crepitus or limited motion are managed with fragment excision if they are too small (typically, <25% of the diameter of the radial head) or osteopenic to be internally fixated.
Larger displaced fractures are typically managed with ORIF with good outcomes in most patients.35,46
Radial head fractures that are displaced but too comminuted to be anatomically reduced and stably fixed and that are too large to consider fragment excision (involve more than a quarter to a third of the radial head) should be managed by radial head excision with or without arthroplasty.1,27
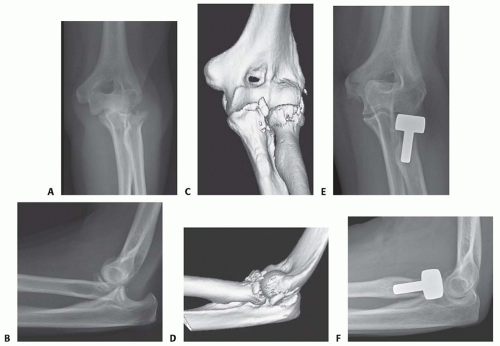
Patients who are known to have, or are likely to have, an associated ligamentous injury of the elbow or forearm should have a radial head arthroplasty because radial head excision is contraindicated (FIG 2).29
The decision as to what fracture is reconstructable depends on surgeon factors (eg, experience), patient factors (eg, osteoporosis), and fracture factors (eg, fragment number and size, comminution, associated soft tissue injuries). The final decision is often made only at the time of surgery.
Other indications for radial head arthroplasty include radial head nonunion or malunion, primary or secondary management of forearm or elbow instability (eg, Essex-Lopresti injury), rheumatoid arthritis or osteoarthritis, and tumors.
Preoperative Planning
Currently available devices include smooth stem spacer implants, press-fit ingrowth stems, monoblock and bipolar devices, and metallic or pyrolytic carbon articulations.
Most implants have an axisymmetric circular design; however, one currently available device has a more anatomic nonaxisymmetric elliptical shape.33,40,47
Silicone radial head implants offer little in the way of axial or valgus stability to the elbow and have been complicated by a high incidence of implant wear, fragmentation, and silicone synovitis leading to generalized joint damage. As a result, they have fallen out of favor and have been replaced by metallic implants.18
Most metallic radial head implants that are currently available are modular with separate heads and stems, allowing improved size matching of the native radial head and neck relative to older monoblock designs.17,28,30
Precise implant sizing and placement are critical with these devices to ensure correct capitellar tracking and to avoid a cam effect with forearm rotation, which may cause premature capitellar wear due to shearing of the cartilage and stem loosening due to increased loading of the stem-bone interface.15
Preoperative radiographic templating of the contralateral normal radial head should be employed in the setting of a secondary radial head replacement but is not needed for acute fractures because the excised radial head is available for accurate implant sizing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree