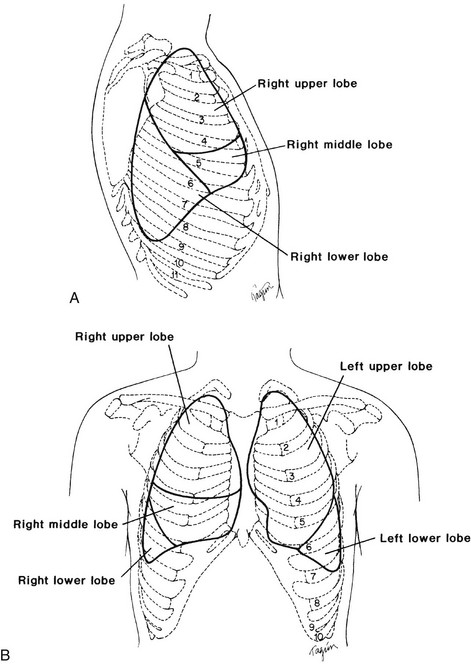
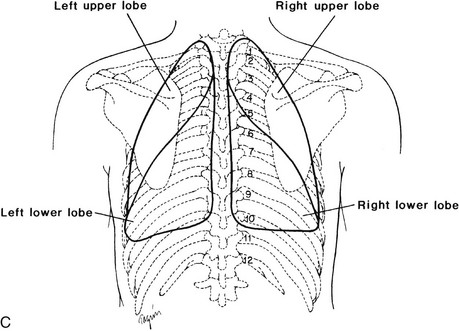
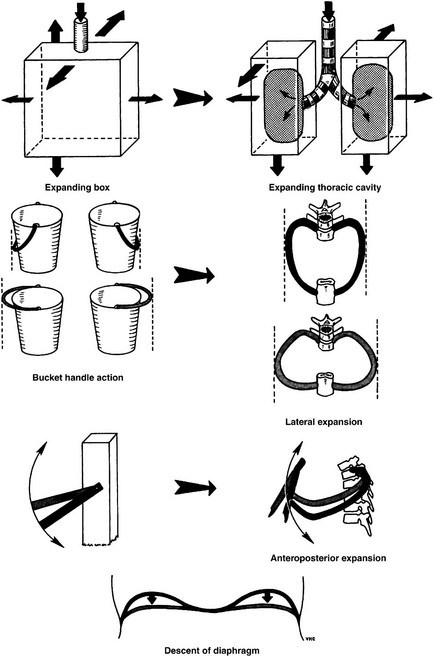
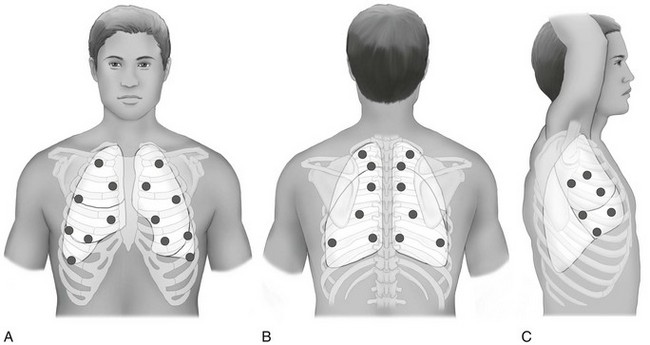
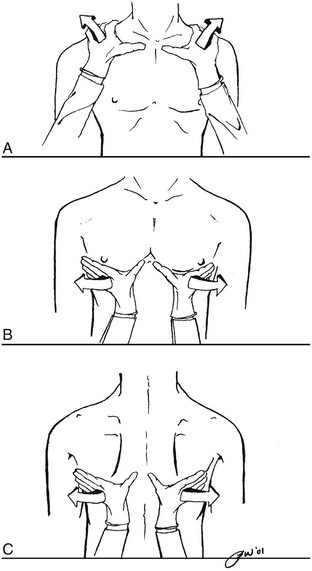
Chapter 4 The objectives of this chapter are the following: 1 Provide a brief review of the structure and function of the pulmonary system 2 Give an overview of pulmonary evaluation, including physical examination and diagnostic testing 3 Describe pulmonary diseases and disorders, including clinical findings, medical-surgical management, and physical therapy intervention • Impaired Aerobic Capacity/Endurance Associated with Deconditioning: 6B • Impaired Ventilation, Respiration/Gas Exchange, and Aerobic Capacity/Endurance Associated with Airway Clearance Dysfunction: 6C • Impaired Ventilation and Respiration/Gas Exchange Associated with Ventilatory Pump Dysfunction or Failure: 6E • Impaired Ventilation and Respiration/Gas Exchange Associated with Respiratory Failure: 6F • Impaired Ventilation, Respiration/Gas Exchange, and Aerobic Capacity/Endurance Associated with Respiratory Failure in the Neonate: 6G Please refer to Appendix A for a complete list of the preferred practice patterns, as individual patient conditions are highly variable and other practice patterns may be applicable. To safely and effectively provide exercise, bronchopulmonary hygiene program(s), or both to patients with pulmonary system dysfunction, physical therapists require an understanding of the pulmonary system and of the principles of ventilation and gas exchange. Ventilation is defined as gas (oxygen [O2] and carbon dioxide [CO2]) transport into and out of lungs, and respiration is defined as gas exchange across the alveolar-capillary and capillary-tissue interfaces. The term pulmonary primarily refers to the lungs, their airways, and their vascular system.1 The primary organs and muscles of the pulmonary system are outlined in Tables 4-1 and 4-2, respectively. A schematic of the pulmonary system within the thorax is presented in Figure 4-1. TABLE 4-1 Structure and Function of Primary Organs of the Pulmonary System Data from Marieb E: Human anatomy and physiology, ed 3, Redwood City, Calif, 1995, Benjamin-Cummings; Moldover JR, Stein J, Krug PG: Cardiopulmonary physiology. In Gonzalez EG, Myers SJ, Edelstein JE et al: Downey & Darling’s physiological basis of rehabilitation medicine, ed 3, Philadelphia, 2001, Butterworth-Heinemann. TABLE 4-2 Primary and Accessory Ventilatory Muscles with Associated Innervation Data from Kendall FP, McCreary EK, editors: Muscles: testing and function, ed 3, Baltimore, 1983, Lippincott, Williams, and Wilkins; Rothstein JM, Roy SH, Wolf SL: The rehabilitation specialist’s handbook, ed 2, Philadelphia, 1998, FA Davis; DeTurk WE, Cahalin LP: Cardiovascular and pulmonary physical therapy: an evidence-based approach, New York, 2004, McGraw-Hill Medical Publishing Division. FIGURE 4-1 A, Right lung positioned in the thorax. Bony landmarks assist in identifying normal right lung configuration. B, Anterior view of the lungs in the thorax in conjunction with bony landmarks. Left upper lobe is divided into apical and left lingula, which match the general position of the right upper and middle lobes. C, Posterior view of the lungs in conjunction with bony landmarks. (From Ellis E, Alison J, editors: Key issues in cardiorespiratory physiotherapy, Oxford, 1992, Butterworth-Heinemann, p 12.) Ventilation is regulated by two separate neural mechanisms: one controls automatic ventilation, and the other controls voluntary ventilation. The medullary respiratory center in the brain stem, which is responsible for the rhythmicity of breathing, controls automatic ventilation. The pneumotaxic center, located in the pons, controls ventilation rate and depth. The cerebral cortex, which sends impulses directly to the motor neurons of ventilatory muscles, mediates voluntary ventilation.3 Arterial levels of CO2 (PCO2), hydrogen ions (H+), and O2 (PO2) can modify the rate and depth of respiration. To maintain homeostasis in the body, specialized chemoreceptors on the carotid arteries and aortic arch (carotid and aortic bodies, respectively) respond to either a rise in PCO2 and H+ or a fall in PO2. Stimulation of these chemoreceptors results in transmission of impulses to the respiratory centers to increase or decrease the rate or depth, or both, of respiration. For example, an increase in PCO2 would increase the ventilation rate to help increase the amount of CO2 exhaled and ultimately lower the PCO2 levels in arterial blood. The respiratory center found in the medulla primarily responds to a rise in PCO2 and H+.4,5 Accessory muscles of inspiration, noted in Table 4-2, are generally not active during quiet breathing. Although not the primary actions of the individual muscles, their contractions can increase the depth and rate of ventilation during progressive activity by increasing the expansion of the thorax. Increased expansion results in greater negative pressures being generated and subsequent larger volumes of air entering the lungs. Although inhalation is an active process, exhalation is a generally passive process. The muscles relax, causing a decrease in the thoracic volume while the lungs deflate to their natural resting state. The combined effects of these actions result in an increase of intrathoracic pressure and flow of air out of the lungs. Contraction of the primary and accessory muscles of exhalation, found in Table 4-2, results in an increase in intrathoracic pressure and a faster rate of decrease in thoracic size, which forces air out of the lungs. These motions are outlined schematically in Figure 4-2.6,7 FIGURE 4-2 Respiratory mechanics (bucket and pump handle motions). (From Snell RS, editor: Clinical anatomy by regions, ed 9, Baltimore, 2012, Lippincott, Williams & Wilkins.) • A concentration gradient in which gases will diffuse from areas of high concentration to areas of low concentration: • Surface area, or the total amount of alveolar-capillary interface available for gas exchange (e.g., the breakdown of alveolar membranes that occurs in emphysema will reduce the amount of surface area available for gas exchange) • The thickness of the barrier (membrane) between the two areas involved (e.g., retained secretions in the alveolar spaces will impede gas exchange through the membrane) Gas exchange is optimized when the ratio of air flow (ventilation A Approximately 97% of O2 transported from the lungs is carried in chemical combination with hemoglobin. The majority of CO2 transport, 93%, occurs in the combined forms of carbaminohemoglobin and bicarbonate. A smaller percentage, 3% of O2 and 7% of CO2, is transported in dissolved forms.10 Dissolved O2 and CO2 exert a partial pressure within the plasma and can be measured by sampling arterial, venous, or mixed venous blood.11 See the Arterial Blood Gas section for further description of this process. In addition to the general chart review presented in Chapter 2, other relevant information regarding pulmonary dysfunction that should be ascertained from the chart review or patient interview is listed as follows11–13: • History of smoking, including packs per day or pack years (packs per day × number of years smoked) and the amount of time that smoking has been discontinued (if applicable) • Presence, history, and amount of O2 therapy at rest, with activity and at night • Exposure to environmental or occupational toxins (e.g., asbestos) • History of pneumonia, thoracic procedures, or surgery • History of assisted ventilation or intubation with mechanical ventilation • History or current reports of dyspnea either at rest or with exertion. Dyspnea is the subjective complaint of difficulty with respiration, also known as shortness of breath. A visual analog scale or ratio scale (Modified Borg scale) can be used to obtain a measurement of dyspnea. The American Thoracic Society Dyspnea Scale can be found in Table 4-3. Note: The abbreviation DOE represents “dyspnea on exertion” TABLE 4-3 American Thoracic Society Dyspnea Scale From Brooks SM: Surveillance for respiratory hazards, ATS News 8:12-16, 1982. • Level of activity before admittance • History of baseline sputum production, including color (e.g., yellow, green), consistency (e.g., thick, thin), and amount. Familiar or broad terms can be applied as units of measure for sputum (e.g., quarter-sized, tablespoon, or copious) • General appearance and level of alertness • Ventilatory or breathing pattern • Presence of digital clubbing • Presence of supplemental O2 and other medical equipment (refer to Chapter 18) Breathing patterns vary among individuals and may be influenced by pain, emotion, body temperature, sleep, body position, activity level, and the presence of pulmonary, cardiac, metabolic, or nervous system disease (Table 4-4). The optimal time, clinically, to examine a patient’s breathing pattern is when he or she is unaware of the inspection because knowledge of the physical examination can influence the patient’s respiratory pattern. TABLE 4-4 Description of Breathing Patterns and Their Associated Conditions CHF, Congestive heart failure; PCO2, partial pressure of carbon dioxide. *Hoover’s sign has been reported to have a sensitivity of 58% and specificity of 86% for detection of airway obstruction. Hoover’s sign is associated with a patient’s body mass index, severity of dyspnea, and frequency of exacerbations and is seen in up to 70% of patients with severe obstruction.† Data from Kersten LD: Comprehensive respiratory nursing: a decision-making approach, Philadelphia, 1989, Saunders; DesJardins T, Burton GG: Clinical manifestations and assessment of respiratory disease, ed 3, St Louis, 1995, Mosby; Auscultation proceeds in a systematic, side-to-side, and cephalocaudal fashion. Breath sounds on the left and right sides are compared in the anterior, lateral, and posterior segments of the chest wall, as shown in Figure 4-4. The diaphragm (flat side) of the stethoscope should be used for auscultation. The patient should be seated or lying comfortably in a position that allows access to all lung fields. Full inspirations and expirations are performed by the patient through the mouth, as the clinician listens to the entire cycle of respiration before moving the stethoscope to another lung segment. FIGURE 4-4 Landmarks for lung auscultation on (A) anterior, (B) posterior, and (C) lateral aspects of the chest wall. (Courtesy Peter P. Wu.) All of the following ensure accurate auscultation: • Make sure stethoscope earpieces are pointing up and inward (toward your patient) before placing in the ears. • Long stethoscope tubing may dampen sound transmission. Length of tubing should be approximately 30 cm (12 in) to 55 cm (21 to 22 in).12 • Always check proper function of the stethoscope before auscultating by listening to finger tapping on the diaphragm while the earpieces are in place. • Apply the stethoscope diaphragm firmly against the skin so that it lays flat. • Observe chest wall expansion and breathing pattern while auscultating to help confirm palpatory findings of breathing pattern (e.g., sequence and symmetry). For example, decreased chest wall motion palpated earlier in the left lower lung field may present with decreased breath sounds in that same area. • Ensure full, deep inspirations (decreased effort can be misinterpreted as decreased breath sounds). • Be aware of the stethoscope tubing’s touching other objects (especially ventilator tubing) or chest hair. • Periodically lift the stethoscope off the chest wall to help differentiate extraneous sounds (e.g., chest or nasogastric tubes, patient snoring) that may appear to originate from the thorax. To maximize patient comfort, allow periodic rest periods between deep breaths to prevent hyperventilation and dizziness. Normal tracheal or bronchial breath sounds are loud tubular sounds heard over the proximal airways, such as the trachea and main stem bronchi. A pause is heard between inspiration and expiration; the expiratory phase is longer than the inspiratory phase. Normal bronchovesicular sounds are similar to bronchial breath sounds; however, no pause occurs between inspiration and expiration.11,12 Breath sounds are abnormal if they are heard outside their usual location in the chest or if they are qualitatively different from normal breath sounds.14 Despite efforts to make the terminology of breath sounds more consistent, terminology may still vary from clinician to clinician and facility to facility. Always clarify the intended meaning of the breath sound description if your findings differ significantly from what has been documented or reported. Abnormal breath sounds with possible sources are outlined in Table 4-5. TABLE 4-5 Possible Sources of Abnormal Breath Sounds Adventitious breath sounds occur from alterations or turbulence in airflow through the tracheobronchial tree and lung parenchyma. These sounds can be divided into continuous (wheezes and rhonchi) or discontinuous (crackles) sounds.12,14 The American Thoracic Society and American College of Chest Physicians have discouraged use of the term rhonchi, recommending instead that the term wheezes be used for all continuous adventitious breath sounds.15 Many academic institutions and hospitals continue to teach and practice use of the term rhonchi; therefore it is mentioned in this section. These sounds are generated from dysfunction outside of the lung tissue. The most common sound is the pleural friction rub. This sound is heard as a loud grating sound, generally throughout both phases of respiration, and almost always is associated with pleuritis (inflamed pleurae rubbing on one another).12,14 The presence of a chest tube inserted into the pleural space also may cause a sound similar to a pleural rub. 1. Whispered pectoriloquy. The patient whispers “one, two, three.” The test is positive for consolidation if phrases are clearly audible in distal lung fields. This test is positive for hyperinflation if the phrases are less audible in distal lung fields. 2. Bronchophony. The patient repeats the phrase “ninety-nine.” The results are similar to whispered pectoriloquy. 3. Egophony. The patient repeats the letter e. If the auscultation in the distal lung fields sound like a, then fluid in the air spaces or lung parenchyma is suspected. The third component of the physical examination is palpation of the chest wall, which is performed in a cephalocaudal direction. Figure 4-5 demonstrates hand placement for chest wall palpation of the upper, middle, and lower lung fields. Palpation is performed to examine the following: FIGURE 4-5 Palpation of (A) upper, (B) middle, and (C) lower chest wall motion. (Courtesy Peter P. Wu.) • Presence of fremitus (a vibration caused by the presence of secretions or voice production, which is felt through the chest wall) during respirations11 • Presence, location, and reproducibility of pain, tenderness, or both • Presence of bony abnormalities, rib fractures, or both • Chest expansion and symmetry • Presence of subcutaneous emphysema (palpated as bubbles popping under the skin from the presence of air in the subcutaneous tissue). This finding is abnormal and represents air that has escaped or is escaping from the lungs. Subcutaneous emphysema can occur from a pneumothorax (PTX), a complication from central line placement, or after thoracic surgery1
Pulmonary System
Preferred Practice Patterns
Body Structure and Function
Structure
Structure
Description
Function
Nose
Paired mucosal-lined nasal cavities supported by bone and cartilage
Conduit that filters, warms, and humidifies air entering lungs
Pharynx
Passageway that connects nasal and oral cavities to larynx, and oral cavity to esophagus
Subdivisions naso-, oro-, and laryngopharynx
Conduit for air and food
Facilitates exposure of immune system to inhaled antigens
Larynx
Passageway that connects pharynx to trachea
Opening (glottis) covered by vocal folds or by the epiglottis during swallowing
Prevents food from entering the lower pulmonary tract
Voice production
Trachea
Flexible tube composed of C-shaped cartilaginous rings connected posteriorly to the trachealis muscle
Divides into the left and right main stem bronchi at the carina
Cleans, warms, and moistens incoming air
Bronchial tree
Right and left main stem bronchi subdivide within each lung into secondary bronchi, tertiary bronchi, and bronchioles, which contain smooth muscle
Warms and moistens incoming air from trachea to alveoli
Smooth muscle constriction alters airflow
Lungs
Paired organs located within pleural cavities of the thorax
The right lung has three lobes, and the left lung has two lobes
Contains air passageways distal to main stem bronchi, alveoli, and respiratory membranes
Alveoli
Microscopic sacs at end of bronchial tree immediately adjacent to pulmonary capillaries
Functional unit of the lung
Primary gas exchange site
Surfactant lines the alveoli to decrease surface tension and prevent complete closure during exhalation
Pleurae
Double-layered, continuous serous membrane lining the inside of the thoracic cavity
Divided into parietal (outer) pleura and visceral (inner) pleura
Produces lubricating fluid that allows smooth gliding of lungs within the thorax
Potential space between parietal and visceral pleura
Pulmonary Muscles
Innervation
Primary inspiratory muscles
Diaphragm
Phrenic nerve (C3-C5)
External intercostals
Spinal segments T1-T9
Accessory inspiratory muscles
Trapezius
Cervical nerve (C1-C4), spinal part of cranial nerve XI
Sternocleidomastoid
Spinal part of cranial nerve XI
Scalenes
Cervical/brachial plexus branches (C3-C8, T1)
Pectorals
Medial/lateral pectoral nerve (C5-C8, T1)
Serratus anterior
Long thoracic nerve (C5-C7)
Latissimus dorsi
Thoracodorsal nerve (C5-C8)
Primary expiratory muscles
Rectus abdominis
Spinal segments T5-T12
External obliques
Spinal segments T7-T12
Internal obliques
Spinal segments T8-T12
Internal intercostals
Spinal segments T1-T9
Accessory expiratory muscles
Latissimus dorsi
Thoracodorsal nerve (C5-C8)
Function
Neural Control
Chemical Control
Mechanics of Ventilation
Gas Exchange.
Ventilation and Perfusion Ratio.
 ) to blood flow (perfusion
) to blood flow (perfusion  ) approaches a 1 : 1 relationship. However, the actual
) approaches a 1 : 1 relationship. However, the actual  ratio is 0.8 because alveolar ventilation is approximately equal to 4 L per minute and pulmonary blood flow is approximately equal to 5 L per minute.2,8,9
ratio is 0.8 because alveolar ventilation is approximately equal to 4 L per minute and pulmonary blood flow is approximately equal to 5 L per minute.2,8,9
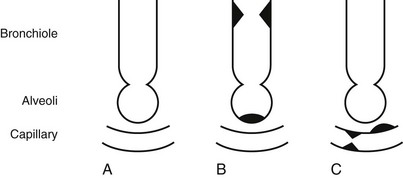
 mismatch (inequality in the relationship between ventilation and perfusion) can occur in certain situations. Two terms associated with
mismatch (inequality in the relationship between ventilation and perfusion) can occur in certain situations. Two terms associated with  mismatch are dead space and shunt. Dead space occurs when ventilation is in excess of perfusion, as with a pulmonary embolus. A shunt occurs when perfusion is in excess of ventilation, as in alveolar collapse from secretion retention. These conditions are shown in Figure 4-3.
mismatch are dead space and shunt. Dead space occurs when ventilation is in excess of perfusion, as with a pulmonary embolus. A shunt occurs when perfusion is in excess of ventilation, as in alveolar collapse from secretion retention. These conditions are shown in Figure 4-3.
Gas Transport.
Evaluation
Patient History
Grade
Degree
0
None
Not troubled with breathlessness except with strenuous exercise
1
Slight
Troubled by shortness of breath when hurrying on the level or walking up a slight hill
2
Moderate
Walks slower than people of the same age on the level because of breathlessness, or has to stop for breath when walking at own pace on the level
3
Severe
Stops for breath after walking about 100 yards or after a few minutes on the level
4
Very severe
Too breathless to leave the house or breathless when dressing or undressing
Inspection
Observation of Breathing Patterns
Breathing Pattern
Description
Associated Conditions
Apnea
Lack of airflow to the lungs for >15 seconds
Airway obstruction, cardiopulmonary arrest, alterations of the respiratory center, narcotic overdose
Biot’s respirations
Constant increased rate and depth of respiration followed by periods of apnea of varying lengths
Elevated intracranial pressure, meningitis
Bradypnea
Ventilation rate <12 breaths per minute
Use of sedatives, narcotics, or alcohol; neurologic or metabolic disorders; excessive fatigue
Cheyne-Stokes respirations
Increasing depth of ventilation followed by a period of apnea
Elevated intracranial pressure, CHF, narcotic overdose
Hyperpnea
Increased depth of ventilation
Activity, pulmonary infections, CHF
Hyperventilation
Increased rate and depth of ventilation resulting in decreased PCO2
Anxiety, nervousness, metabolic acidosis
Hypoventilation
Decreased rate and depth of ventilation resulting in increased PCO2
Sedation or somnolence, neurologic depression of respiratory centers, overmedication, metabolic alkalosis
Kussmaul respirations
Increased regular rate and depth of ventilation
Diabetic ketoacidosis, renal failure
Orthopnea
Dyspnea that occurs in a flat supine position. Relief occurs with more upright sitting or standing
Chronic lung disease, CHF
Paradoxic ventilation
Inward abdominal or chest wall movement with inspiration and outward movement with expiration
Diaphragm paralysis, ventilation muscle fatigue, chest wall trauma
Sighing respirations
The presence of a sigh >2-3 times per minute
Angina, anxiety, dyspnea
Tachypnea
Ventilation rate >20 breaths per minute
Acute respiratory distress, fever, pain, emotions, anemia
Hoover’s sign*
The inward motion of the lower rib cage during inhalation
Flattened diaphragm often related to decompensated or irreversible hyperinflation of the lungs
Auscultation
Normal Breath Sounds.
Tracheal, Bronchial, or Bronchovesicular Sounds.
Abnormal Breath Sounds.
Sound
Possible Etiology
Bronchial (abnormal if heard in areas where vesicular sounds should be present)
Fluid or secretion consolidation (airlessness) that could occur with pneumonia
Decreased or diminished (less audible)
Hypoventilation, severe congestion, or emphysema
Absent
Pneumothorax or lung collapse
Adventitious Breath Sounds.
Extrapulmonary Sounds.
Voice Sounds.
Palpation
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pulmonary System
Only gold members can continue reading. Log In or Register to continue