Pulmonary Stenosis
John P. Cheatham
Obstruction of pulmonary blood flow may occur within the right ventricle, at the valve, or anywhere in the pulmonary arterial system. In general terms, pulmonary stenosis occurs in approximately 20% to 30% of all patients with congenital heart disease. In approximately one-half of these patients, the ventricular septum is intact.
PULMONARY VALVE STENOSIS
Epidemiology
Pulmonary valve stenosis constitutes approximately 7% to 12% of all congenital heart disease and as many as 80% to 90% of all lesions causing obstruction of right ventricular output. The defect originally was described in 1761 by Morgagni. The exact pathogenetic mechanism for its development is unclear. Several authors suggest that an abnormality of the distal bulbus cordis leads to valvar obstruction with sparing of the proximal bulbus, which participates in closure of the ventricular septum. Fetal endocarditis also is implicated in the etiology of this defect. Genetic factors may play an equally important role because pulmonary valve stenosis often is found in various syndromes.
Pathology
The gross and microscopic features of pulmonary valve stenosis are classified into six categories: domed (42%); tricuspid (6.5%); bicuspid (10%); unicommissural (16%); hypoplastic annulus (6.5%); and dysplastic (19%). The pathologic processes affecting the remaining portion of the right-sided cardiac structures involve changes secondary to the valve obstruction (i.e., right ventricular hypertrophy, fibrosis, and tricuspid valve abnormalities).
Clinically, pulmonary valve stenosis with intact ventricular septum is described best as mild, moderate, or severe. Mild stenosis is defined here as a systolic transvalvular gradient of less than 40 mm Hg or right ventricular pressure of less than one-half of systemic arterial pressure. Moderate obstruction is considered to be present when the systolic gradient across the pulmonary valve is greater than 40 mm Hg or right ventricular pressure is greater than one-half of, but still less than, systemic arterial pressure. Severe stenosis is defined as a systolic gradient of more than 80 mm Hg or the presence of suprasystemic right ventricular pressure.
Clinical Manifestations and Complications
Patients with mild stenosis are asymptomatic, exhibiting normal growth and development and no cyanosis. The jugular venous pulse is normal, and no sign of congestive heart failure is present. Children with moderate stenosis and an intact ventricular septum may develop mild dyspnea with exertion, but frequently they are asymptomatic. Cyanosis with exertion may be noted occasionally if an atrial septal defect is present. Individuals with severe valvular stenosis usually demonstrate
symptoms, although as many as 25% of these patients are asymptomatic. Frequently, dyspnea and fatigue with only a moderate amount of exertion are present. Central cyanosis is one of the most important signs in patients with an atrial communication; it may be present at rest or with minimal exercise. Some evidence indicates that the degree of cyanosis increases with age. When “squatting” is seen in a cyanotic child suspected of having pulmonary valve stenosis, the diagnosis of tetralogy of Fallot must be considered. Growth and development in infants with severe stenosis usually are normal, without evidence of wasting. “Moon facies” in conjunction with a chubby phenotype has been described as characteristic of young children with pulmonary valve stenosis, but it is not pathognomonic and is present in fewer than 50% of infants with severe obstruction.
symptoms, although as many as 25% of these patients are asymptomatic. Frequently, dyspnea and fatigue with only a moderate amount of exertion are present. Central cyanosis is one of the most important signs in patients with an atrial communication; it may be present at rest or with minimal exercise. Some evidence indicates that the degree of cyanosis increases with age. When “squatting” is seen in a cyanotic child suspected of having pulmonary valve stenosis, the diagnosis of tetralogy of Fallot must be considered. Growth and development in infants with severe stenosis usually are normal, without evidence of wasting. “Moon facies” in conjunction with a chubby phenotype has been described as characteristic of young children with pulmonary valve stenosis, but it is not pathognomonic and is present in fewer than 50% of infants with severe obstruction.
Diagnosis
The cardiovascular examination aids in establishing the diagnosis of pulmonary valve stenosis. The precordial activity is quiet with mild obstruction, but it may be increased with a palpable right ventricular tap in patients with moderate or severe stenosis. A systolic thrill over the pulmonary valve area may be present as the severity increases. The striking auscultatory feature of pulmonary valve stenosis is a prominent systolic ejection murmur. The murmur may vary in length and intensity, but it usually ends before the aortic valve closes. The maximum intensity of the murmur is at the upper left sternal border radiating to the back, but it also is heard along the precordium and the neck. As the severity increases, the systolic ejection murmur lengthens, and the peak in intensity occurs later. The murmur of pulmonary valve stenosis increases in duration and intensity after amyl nitrate inhalation, whereas the opposite is true in children with tetralogy of Fallot.
A high-pitched ejection sound or systolic click usually is audible along the left upper sternal border. The click probably originates from the sudden opening and doming of the thickened pulmonary valve leaflets. As the severity of the obstruction increases, the systolic ejection click occurs earlier until, in severe stenosis, it may be indistinguishable from the first heart sound. The second heart sound usually is split and of normal intensity in mild stenosis. The degree of splitting is directly proportional to the severity of obstruction. An inverse relationship exists between the severity of stenosis and the intensity of the pulmonary component of the second heart sound. In severe stenosis, therefore, a wide splitting of the second heart sound is present, with a very soft pulmonary component that often is heard as a single second sound.
The electrocardiogram frequently is normal in patients with mild stenosis, whereas it is normal in only 10% of children with moderate obstruction, and it is uniformly abnormal in cases of severe stenosis. Right axis deviation frequently is seen, with right ventricular hypertrophy noted in the anterior precordial leads. In patients with moderate stenosis, the magnitude of the R wave in V1 usually is less than 20 mm, whereas an upright T wave in V1 is present approximately 50% of the time. A qR or a pure R wave of more than 20 mm is present in patients with severe stenosis. In some children, ST or T waves may suggest ischemia.
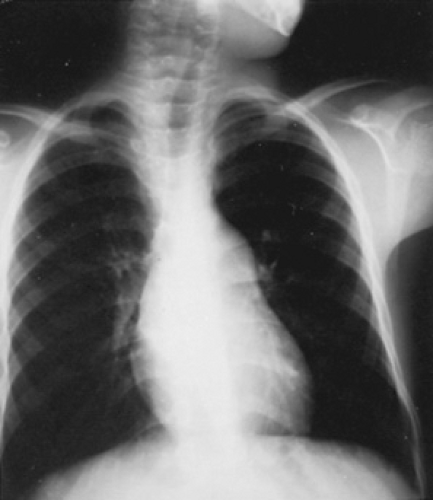
The most consistent and distinctive radiographic feature is prominence in the main pulmonary artery segment secondary to poststenotic dilation of the pulmonary trunk and the proximal left pulmonary artery (Fig. 274.1). This finding is present in as many as 90% of patients, but it does not correlate with the severity of obstruction. In patients with severe stenosis, the cardiac apex may be tilted upward, and generalized cardiomegaly and right atrial prominence may be present, especially if right-sided failure is present. The aortic arch usually is left-sided. Presence of a right arch should lead the physician to consider the diagnosis of tetralogy of Fallot.
The noninvasive evaluation of abnormalities of the pulmonary valve by M-mode and two-dimensional echocardiography has been less than satisfactory. Doppler echocardiography with color flow mapping techniques increases both the sensitivity and specificity of the diagnosis of pulmonary valve stenosis. Two-dimensional echocardiography enables visualization of the thickened and domed pulmonary valve leaflets, pulmonary annulus, dilated pulmonary trunk, hypertrophic right ventricle, and other associated congenital heart defects. Pulsed and continuous-wave Doppler echocardiography enable accurate estimation to be made of the location and severity of pulmonary stenosis without using invasive procedures. The recorded peak flow velocity on spectral display is converted to an estimated transvalvular pressure gradient using the modified Bernoulli equation: PG = 4V2, where PG equals instantaneous pressure gradient (mm Hg) and V equals peak Doppler velocity (m/second). Color-coded Doppler echocardiography may provide additional hemodynamic information about patients with pulmonary valve stenosis.
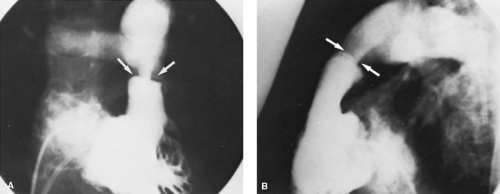
The role of cardiac catheterization and angiography in the diagnosis and treatment of pulmonary valve stenosis has changed significantly since the early 1980s. In the past, information obtained in the catheterization laboratory was a prerequisite for selecting patients for surgical valvotomy. Since the initial use of percutaneous, transluminal balloon pulmonary valvuloplasty in 1982, the catheterization laboratory has become the location for the “treatment” of moderate and severe pulmonary valve stenosis. The most important hemodynamic information obtained during cardiac catheterization is the measurement of right ventricular pressure simultaneously with left ventricular or aortic pressure and the systolic gradient across the pulmonary valve. Defining any associated cardiac defects at this time also is important. The use of biplanar angiocardiography with high-resolution video disks, recorders, and monitors has helped greatly in the use of therapeutic techniques during interventional pediatric cardiac catheterization. Angiographic features of pulmonary valve stenosis include thickening and doming of valve leaflets with poststenotic dilation of the pulmonary trunk (Fig. 274.2).
Some studies demonstrate hemodynamic abnormalities during exercise in children and adults with pulmonary valve stenosis. In both children and adults with severe stenosis, myocardial performance during exercise was altered (i.e., decreased stroke and cardiac index and increased right ventricular end-diastolic pressure). Adults, however, had a disproportionately lower cardiac index and heart rate at rest and during exercise than did children with obstruction of the same magnitude. Evidence exists of myocardial fibrosis in uncorrected moderate to severe pulmonary valve stenosis in adults, which suggests the need for aggressive treatment of this condition during childhood.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree