Proximal Row Carpectomy
Kathryn A. Heim
Alex M. Meyers
Thomas B. Hughes
Mark E. Baratz
DEFINITION
Proximal row carpectomy (PRC) involves removal of the proximal carpal row (scaphoid, lunate, and triquetrum).
PRC has been described as a treatment option for a number of pathologic conditions:
Scaphoid nonunion advanced collapse (SNAC) wrist
Scapholunate advanced collapse (SLAC) wrist
Kienböck disease
Chronic or missed perilunate dislocation
Scaphoid osteonecrosis or Preiser disease
Wrist deformity or contracture
ANATOMY
The proximal row of the wrist consists of three bones: scaphoid, lunate, and triquetrum.
The proximal row moves as a single unit through intercarpal ligamentous attachments and bony congruity.
The proximal row flexes with radial deviation and extends with ulnar deviation.
The capitate, in the distal row, articulates with the lunate.
The proximal capitate articular surface is relatively, although not completely, congruous with the lunate facet of the radius.
PATHOGENESIS
A number of pathologic conditions lead to wrist degeneration requiring PRC. Patients with progressive pain and limited motion can gain relief following this procedure.
SNAC and SLAC
Stage I: degenerative changes along the radial half of the radioscaphoid articulation. In SNAC wrists, the degenerative changes are typically limited to the articulation between the distal scaphoid fragment and the radius.
Stage II: degenerative changes involving the entire radioscaphoid articulation (FIG 1). In SNAC wrists, the articulation between the proximal scaphoid fragment and the radius is preserved, and instead, stage II degeneration occurs in the scaphocapitate joint.
Stage III: degenerative changes at the capitolunate joint. The radiolunate joint is spared.
Kienböck disease
Stage I: normal plain radiographs with wrist pain and positive magnetic resonance imaging (MRI) finding
Stage II: sclerosis without collapse of the lunate
Stage IIIa: lunate collapse without instability
Stage IIIb: where there is lunate collapse with carpal instability (dorsal intercalated segmental instability [DISI]: flexion of the scaphoid with extension of the lunate)
Stage IV: fixed carpal instability with pancarpal degenerative changes
Missed perilunate dislocation
Scaphoid osteonecrosis (Preiser disease)
Congenital or spastic wrist and hand flexion contractures severe enough that a PRC allows deformity correction that tendon lengthening procedures alone would be unable to correct.
PATIENT HISTORY AND PHYSICAL FINDINGS
Determine the cause of the wrist degeneration.
Mechanical wrist pain is aggravated by use and relieved by rest. The history must support this for the proposed treatment to be successful.
The history defines the patient’s symptoms, level of severity, and progression over time as well as any previous attempts at treatment.
Limited and painful wrist motion with diminished grip strength tends to be a common denominator regardless of the initial source of pathology.
Normal range of motion: wrist extension, 70 degrees; wrist flexion, 75 degrees; radial deviation, 20 degrees; ulnar deviation, 35 degrees. This varies considerably.
Normal grip strength: Mean grip for males is 103 to 104 for the dominant extremity and 92 to 99 for the nondominant extremity. Mean grip for females is 62 to 63 for the
dominant extremity and 53 to 55 for the nondominant extremity.6
Radioscaphoid joint line tenderness on palpation implies radioscaphoid arthritis.
Swelling over the dorsal and dorsoradial aspects of the wrist can be associated with radiocarpal and intercarpal arthritis. Most often, dorsoradial wrist swelling will be visible and palpable in cases of SLAC and SNAC.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs assist with making the underlying diagnosis (eg, SNAC wrist, SLAC wrist, Kienböck disease).
Evaluate the articular facets and surfaces, specifically the head of the capitate and lunate facet of the radius.
Look for other sources of limited wrist motion, diminished grip strength, and pain (eg, thumb carpometacarpal arthritis, scapholunate instability without degenerative changes, fracture).
MRI has limited use with the exception of suspected Kienböck disease or Preiser disease.
DIFFERENTIAL DIAGNOSIS
Triangular fibrocartilage complex or distal radioulnar joint pathology
Extensor carpi ulnaris, flexor carpi ulnaris, flexor carpi radialis tendinitis
De Quervain tenosynovitis
Thumb carpometacarpal arthritis
Scapholunate or lunotriquetral instability without degenerative changes
SURGICAL MANAGEMENT
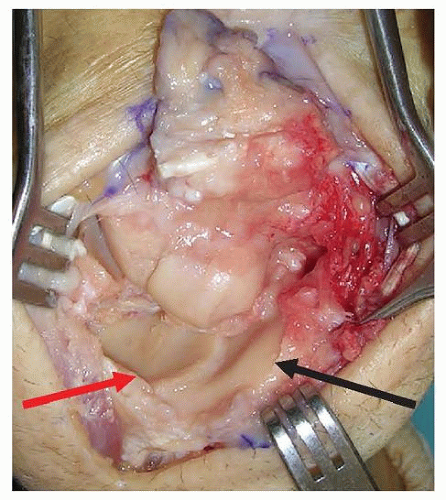
The integrity of the articular cartilage on the head of the capitate and the lunate facet of the radius are critical. The ultimate assessment is made intraoperatively.
Indications
SLAC and SNAC wrist degeneration: stage I, II, or III (only if the degenerative changes at proximal capitate are limited to thinning or minor fissuring)
Kienböck disease (stage IIIb)
Chronic or missed perilunate dislocations
Scaphoid osteonecrosis (Preiser disease)
Wrist deformity or contracture
Contraindications
Active inflammatory arthritis (rheumatoid arthritis). PRC may be used for inflammatory arthritis patients with “burnout” disease (those without active synovitis).
Advanced degenerative changes at the proximal articular surface of the capitate or lunate facet of the radius
Ulnar carpal translation or subluxation of the radiocarpal joint
Relative contraindications
Heavy laborers
Young (younger than 35 years) active patients8
Preoperative Planning
Review the plain radiographs of the wrist. Scrutinize the location of degenerative changes.
Obtain consent for alternative procedures from the patient (ie, if you find excessive degenerative changes on the capitate head, you might proceed with an intercarpal arthrodesis).
Regional anesthesia, general anesthesia, or a combination of the two (for postoperative analgesia) is suitable.
Positioning
The patient is supine with the arm on a radiolucent arm board.
A nonsterile tourniquet preset at 250 mm Hg is on the upper arm.
The shoulder, elbow, and hand are positioned such that the hand rests in pronation at the center of the arm board.
TECHNIQUES
▪ Incision and Exposure
Make a dorsal longitudinal skin incision over the fourth dorsal compartment or a transverse incision across the dorsal wrist crease just distal to the tubercle of Lister.
The longitudinal incision is more extensile and versatile.
The transverse incision tends to be more cosmetic.
Expose the extensor retinaculum.
Maintain full-thickness flaps when elevating soft tissues off the extensor retinaculum to minimize the risk of damage to the radial and ulnar sensory nerves (TECH FIG 1A).
Incise the extensor retinaculum in line with extensor pollicis longus (EPL) and transpose the EPL radially, dorsal to the retinaculum.
Incise the radial septum of the fourth dorsal compartment and expose the wrist capsule by retracting the fourth compartment extensor tendons ulnarly and the EPL and radial wrist extensor tendons radially.
Look for the distal extent of the posterior interosseous nerve (PIN) in the proximal portion of the incision on the radial floor of the fourth compartment. Perform a PIN neurectomy after coagulating the accompanying vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree