Proximal Interphalangeal and Metacarpophalangeal Joint Surface Replacement Arthroplasty
Christopher R. Goll
Peter M. Murray
DEFINITION
Rheumatoid arthritis is a disorder that can affect the hands and can cause systemic symptoms of fatigue, muscle pain, loss of appetite, depression, weight loss, anemia, and immunocompromise. The effect on the hands is a combination of tenosynovitis and inflammation of the metacarpophalangeal (MCP) synovial lining of the joints (synovitis).14,17
Rheumatoid arthritis less frequently involves the proximal interphalangeal (PIP) joints of the hand; more commonly, the PIP joints are affected by degenerative arthritis or psoriatic arthritis. Degenerative arthritis may occur after trauma or infection or may arise as an idiopathic process.1
PATHOGENESIS
Rheumatoid arthritis is a multifactorial entity.
The disease is autoimmune mediated and may occur after a bacterial or viral infection.
There is a hereditary influence.
The B lymphocytes, T lymphocytes, and macrophages lead to proliferation and hypertrophy of synovial cells. The enzymes released by these cells can cause bony erosions, ligamentous laxity, and tendon ruptures.14
MCP joint deformities in rheumatoid patients include concentric joint wear as well as ulnar deviation and volar subluxation or dislocation of the proximal phalanx on the metacarpal head (FIG 2).4,15
These deformities occur after synovial proliferation in the recesses between the collateral ligaments and the metacarpal head, attenuating the collateral ligaments.
Radial inclinations of the metacarpals and wrist joint destruction often leads to an ulnar translation of the entire carpus. This translation can cause ulnar and volar extensor tendon subluxation between the metacarpal heads. Ulnar forces generated by the extensor apparatus and volar forces produced by the flexors lead to ulnar drift of the fingers and fixed MCP flexion deformities or volar dislocations of the MCP joints.
Degenerative arthritis affecting the PIP joints of the hand is a process whereby the articular cartilage develops irreversible wear changes, caused by an incompletely understood mechanism. Subchondral bone stiffens and periarticular new bone formation occurs, which leads to restricted joint motion and pain.11
Less commonly, degenerative arthritis can affect the MCP joints of the hand. This can occur after trauma, infection, and osteonecrosis or may be idiopathic, having a predilection for the index and long MCP joints.11
NATURAL HISTORY
Rheumatoid arthritis has a variable prognosis based on the severity of the disease and the structures involved. Mild presentations may go undiagnosed for years, whereas severe presentations may progress to rapid joint destruction in the third or fourth decade of life.
Three clinical stages of rheumatoid arthritis exist.
First, swelling of the synovial lining, which causes pain, warmth, stiffness, redness, and fullness around the joint
Second, synoviocyte hypertrophy and proliferation leading to synovial thickening
Third, enzymatic release causing bone and cartilage destruction, ligamentous laxity, and tendon ruptures
Medical management as well as surgical management, including synovectomy, can halt or minimize progression of rheumatoid arthritis.
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough patient history and physical examination are important before implant arthroplasty of the fingers.
The surgeon should note the patient’s occupation, hobbies, and expectations.
The history of the patient’s condition is helpful in gauging the progression of the disease.
The primary indication for surface replacement arthroplasty of the MCP or PIP joints is pain relief. Correction of deformity and improvement in function are secondary considerations. It is important to remember that profound deformity may be painless and functional for some.
Examination of the entire upper extremity should be performed. Although the order of reconstruction is controversial, deficits of the shoulder, wrist, and elbow should be addressed before addressing hand conditions.
Particular attention should be paid to elements of radiocarpal instability, including ulnar translation of the carpus as well as distal radioulnar joint instability. In some situations, a wrist arthrodesis or wrist realignment procedure may be necessary before performing MCP arthroplasties.6
Failure to correct carpal collapse and radial deviation of the metacarpals can result in recurrence of ulnar drift deformity after MCP arthroplasty.
Careful examination of flexor and extensor tendons of the hand and wrist should be performed. The extensor digiti quinti minimi, extensor pollicis longus, and flexor pollicis longus often rupture in more active forms of rheumatoid arthritis.
Extensor tendon or flexor tendon ruptures should be treated before considering implant arthroplasty of the hand.
Examination of the PIP joint should include range-of-motion assessment of the joint, assessment of volar plate integrity, central slip integrity, and collateral ligament stability.
Normal range of motion of the PIP joint is 0 to 110 degrees.
Varus and valgus stability should be compared to the contralateral side.
Failure of volar plate integrity in rheumatoid arthritis can lead to swan-neck deformity, which is characterized by PIP joint hyperextension, dorsal subluxation of the lateral bands, and flexion of the distal phalangeal joint. The swan-neck deformity is considered a relative contraindication for surface replacement arthroplasty of the PIP joint (FIG 3A).
A boutonnière deformity is caused by failure of the central slip mechanism. This can occur in rheumatoid arthritis or after trauma (FIG 3B). It is characterized by flexion of the PIP joint due to central slip incompetence, volar subluxation of the lateral bands, and hyperextension of the distal interphalangeal (DIP) joint.
Normal MCP range of motion is between 0 and 90 degrees.
Instability testing: The individual MCP or PIP joints are tested by the examiner grasping the patient’s finger and then applying a valgus and then a varus stress in approximately 30 degrees of flexion. The resultant opening of the joint, or laxity, is compared to the contralateral side. Differences in laxity indicate ligamentous instability. Attempts at hyperextension of the digit at the PIP or the MCP joint can identify volar plate instability and the propensity of the digit to subluxate or dislocate. Surface replacement arthroplasty of either the MCP or the PIP joint is contraindicated in patients with ligamentous instability, as these are semiconstrained devices.
Grade 1: no difference in joint line opening compared to the contralateral joint
Grade 2: notable opening of the joint line compared to the contralateral joint, but a solid “end point” is reached
Grade 3: complete opening of the radial or lateral joint line with valgus or varus stress. This can be demonstrated at either the MCP or the PIP joints. No end point can be discerned.
Bunnell test of intrinsic tightness of the PIP joints: The resistance to flexion of the PIP joint encountered with the MCP joint in the extended position is compared with the resistance encountered with the MCP joint in the flexed position. An increase of resistance to flexion of the PIP joint with the
MCP joint in the extended position indicates intrinsic tightness of that digit.
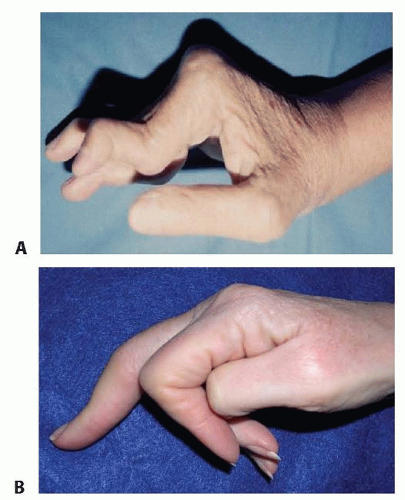
FIG 3 • A. Rheumatoid arthritis of the hand demonstrating swan-neck deformity and volar subluxation of the MCP joints. B. Boutonnière deformity of the digit.
It is important to distinguish intrinsic tightness from extrinsic tightness. Extrinsic tightness is encountered when the long extensors of the digits are adherent to either the surrounding soft tissues or the metacarpals. The result is increased resistance to flexion of the PIP joint with the MCP in flexion. In either instance, the limitation of motion is important to clarify, as it can affect the outcome of implant arthroplasty of the MCP or the PIP joint.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Posteroanterior, lateral, and oblique views of the hands will adequately image the MCP joints. Brewerton views may add additional information.
Posteroanterior and lateral views of the digits are preferred to image the PIP joints.
DIFFERENTIAL DIAGNOSIS
Psoriatic arthritis
Chronic septic arthritis
Osteomyelitis
Gout
Articular malunions of the MCP and PIP joints
Scleroderma
NONOPERATIVE MANAGEMENT
Nonoperative management in rapidly progressing rheumatoid arthritis is largely ineffective.
In the quiescent forms of rheumatoid arthritis, nighttime wrist and hand splinting in conjunction with medical management may provide pain relief. Various combinations of prednisone, remitting agents (eg, methotrexate, hydroxychloroquine sulfate, sulfasalazine, adalimumab, etanercept, infliximab, minocycline), and nonsteroidal anti-inflammatory agents may prove effective for extended periods in certain cases.
During periods of active rheumatoid arthritis of the MCP joints, corticosteroid injections into the joint may provide acute pain relief and improve function in the short term.
The symptoms of MCP and PIP joint degenerative arthritis may come and go, successfully responding to nighttime wrist and hand splinting and nonsteroidal anti-inflammatory agents.
Corticosteroid injection into the MCP and PIP joints for advanced degenerative arthritis seldom provides long-term benefits.
SURGICAL MANAGEMENT
The indications for surface replacement or pyrocarbon MCP arthroplasty are similar to those for flexible MCP implants. These include pain in the face of deformity and worsening function.
Surface replacement implants are designed to recreate the anatomy of a native joint, potentially resulting in greater stability than with flexible MCP implants.
The enhanced stability of these implants is best demonstrated in the index and long fingers, where flexible MCP implants are prone to fracture and failure due to the increased forces born by these joint in pinch.
Contraindications to surface replacement implant arthroplasty of the MCP joint include infection, lack of adequate bone stock, insufficient radial or ulnar collateral ligament support, lack of adequate soft tissue coverage, and excessively small metacarpal or proximal phalanx medullary canals.
These implants rely on intact soft tissue elements. This includes functioning flexors and extensors as well as intact radial and ulnar collateral ligaments.
Indications for PIP joint surface replacement arthroplasty are pain and diminishing function in the context of advanced radiographic articular degeneration.1,8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree