Proximal Humerus Fracture Closed Reduction and Percutaneous Pinning
Carley Vuillermin
Donald S. Bae
Proximal humerus fractures represent less than 5% of all pediatric fractures, and debate remains about which fractures require surgical treatment.
The proximal humeral physis closes around 14 years old in girls and 16 years old in boys. The proximal physis contributes 80% of the longitudinal growth of the humerus, resulting in great remodeling potential. Furthermore, given the compensatory, multiplanar motion of the glenohumeral joint, some residual proximal humeral deformity is well tolerated. The vast majority of these fractures can therefore be managed nonoperatively.
Neer and Horwitz provided the most consistently used classification of proximal humeral epiphyseal fractures according to the degree of displacement (Table 13-1). Assessment of precise angulation of the proximal humerus is more difficult, and orthogonal radiographic views should be assessed in clinical decision making.
The decision for operative management should be based on the patient’s age, remaining skeletal growth, fracture angulation and translation, as well as the associated injuries. If a decision for reduction and fixation is made, the aim of the procedure must be to achieve a stable, adequate reduction and healing without complication.
INDICATIONS/CONTRAINDICATIONS
Absolute indications for surgical treatment include open fractures and those with vascular compromise. Similarly, fractures with significant soft-tissue interposition and impending skin penetration should undergo reduction and fixation.
Relative indications for surgical reduction and fixation continue to evolve and depend on the age of the patient, the remaining skeletal growth, the degree of displacement, and angulation. Surgical treatment is considered for patients with deformity exceeding what would be anticipated to remodel with remaining skeletal growth.
TABLE 13-1 Neer-Horowitz Classification | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Empiric reference values were introduced by Beaty in his Instructional Course Lecture in 1992 and remain a good reference in determining acceptable deformity.
|
Greater tuberosity position more cephalad than the articular surface is also a relative indication in those patients with less than 2 years of growth remaining, due to the risk of impingement in abduction.
PREOPERATIVE PREPARATION
Fracture assessment
Fracture pattern and displacement are determined by the nature of the injury as well as the soft tissues acting on the fragments.
Consider the likely deforming forces and potential blocks to reduction. Assessment of orthogonal images will provide the most useful clues to the necessary reduction maneuvers (Fig. 13-1A, B).
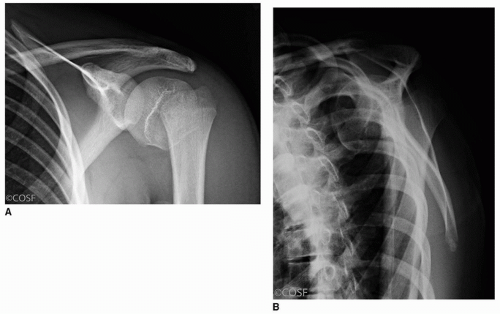
FIGURE 13-1 Initial shoulder radiographs. A. Anteroposterior. B. Scapular lateral. (Courtesy of the Children’s Orthopaedic Surgery Foundation, Boston, MA.)
The rotator cuff insertion into the lesser and greater tuberosities tends to pull the proximal fragment into a mild degree of abduction and external rotation. The pectoralis major leads to anterior and medial translation of the shaft at the fracture site. The deltoid may abduct the shaft distally and lead to shortening.
A periosteal hinge may remain intact; this is most commonly posteromedially.
Up to half of the time, a closed reduction may not be able to be achieved, and therefore, you must be prepared for open reduction. The most common blocks to reduction are the long head of biceps and periosteal interposition.
Implant selection
0.0625 in. (1.6-mm)- or 5/64th in. (2.0-mm)-diameter smooth Kirschner (K)-wires; alternatively 3.5-mm or 4.5-mm cannulated screws may be considered though is not our preference.
Threaded pins may be used; however, they will always require a return to the operating room to remove in a child.
2.0- or 2.5-mm drill for creation of the entry site.
SURGICAL PROCEDURE
Anesthesia
General anesthesia with muscle relaxation facilitates reduction.
Patient positioning
Modified beach chair on a radiolucent table or shoulder-specific table (Fig. 13-2). Elevating the head of the bed 45 to 60 degrees allows for gravity to assist with reduction, but does not expose the patient to the same risks of cerebral hypoperfusion that may occur with more extreme upright positioning. Beach chair positioning also facilitates “over-the-top” anteroposterior fluoroscopic imaging.
A small roll at the medial border of the scapular assists with stabilizing the scapular blade and therefore proximal humerus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








