Proximal Femoral Fractures Treated with Arthroplasty
Douglas E. Padgett
Joseph B. Assini
Introduction
Hip fractures are a cause of significant morbidity and mortality. The cost of treatment is estimated to be in excess of nine billion dollars/year (1). With the aging population in North America the incidence will increase, putting excessive strain on an already taxed health care system. In 2008 there were over 340,000 hip fractures diagnosed in the United States and this is projected to rise to 580,000 by the year 2040 (2). Elderly patients are the largest cohort suffering from these injuries. Thus, both orthopedic and nonorthopedic issues need to be addressed by the orthopedic, geriatric, and rehab team when considering treatment options. Aside from age; activity level, social dynamics, and patient cognitive level should play a role in surgical planning. Broadly speaking surgical choices are divided into arthroplasty and osteosynthesis via internal fixation. This chapter will be to focus on the indications, technical challenges, and literature around the use of arthroplasty for treating hip fractures primarily and in the conversion of internal fixation devices and failed arthroplasty.
Historical Developments and Trends in Femoral Neck Fracture
In the young patient, and historically in all patients, osteosynthesis was considered the gold standard for hip fractures regardless of fracture pattern. Common complications prevalent in femoral neck fractures include nonunion, malunion, and osteonecrosis. As surgeons became more familiar with endoprosthetic designs, their use in treating displaced femoral neck fractures has grown substantially. A long-term randomized control trial (3) and a meta-analysis of RCT’s with nearly 1,200 patients (4) both found favorable outcomes in femoral neck fractures treated with arthroplasty in older patients. Still, the precise indications for arthroplasty in the acute fracture setting are not agreed upon.
Arthroplasty options first appeared in the 1960s with the earliest endoprosthetic designs being uncemented monopolar femoral stems. A major issue with these early designs was acetabular wear and erosion. To diminish forces across the acetabulum, bipolar hemiarthroplasties were introduced in the mid-1970s. Persistent issues continued in more active patients with decreased joint motion, persistent acetabular erosion, and diminished hip function leading some surgeons to recommend the use of total hip arthroplasty (THA) for the treatment of displaced neck of femur fractures.
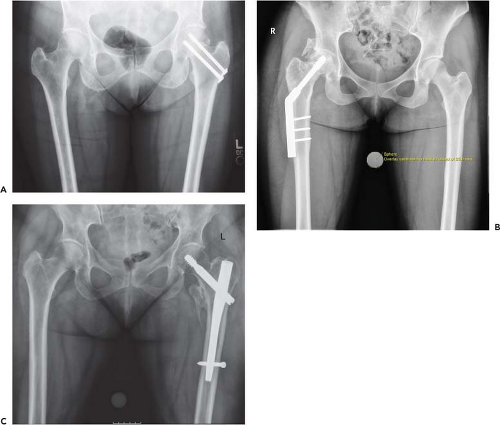
Nondisplaced femoral neck fractures in most patients, regardless of age should be treated with internal fixation. Subcapital and intertrochanteric fractures may also be treated with osteosynthesis in certain settings and patient populations (Fig. 77.1). Similarly, in displaced femoral neck fractures in the young patient, most surgeons still favor internal fixation over arthroplasty. However, in the older patient with a displaced fracture of the femoral neck primary arthroplasty should be considered. Patient factors such as general health, premorbid activity level, cognitive function, and bone stock must be assessed by the operating surgeon to determine if THA or hemiarthroplasty is most appropriate. Generally, if there is preexisting hip pain, significant osteoarthritis, and pathologic bone disease (i.e., metabolic/oncologic), THA should be considered as a primary treatment.
Femoral neck fractures occur in a bimodal distribution with regards to age and mechanism. Younger patients typically sustain femoral neck fracture as the result of high energy trauma and often occur in conjunction with other injuries. Older patients with femoral neck fracture usually sustain the injury as a result of lower energy mechanism such as fall from standing height. In both populations however, treatment algorithms begin with the amount of fracture displacement. Nondisplaced or valgus-impacted patterns in both patient populations should be treated with in situ pinning. Given the majority of blood supply to the femoral head is derived from an extracapsular source via the retinacular vessels these fractures should heal uneventfully. Increased fracture displacement however, increases vessel injury and a tamponade effect within the capsule can further diminish blood supply and predispose to development of avascular necrosis.
Proponents of osteosynthesis suggest that internal fixation after anatomic reduction provides more natural hip mechanics, a lower risk of dislocation, and decreased OR time with lower mortality risk (2). Anatomic reduction however is paramount and technical errors in the placement of hardware can lead to early failure, nonunion, or clinical dissatisfaction. A meta-analysis of nine randomized trials (1,162 patients) has shown an increased rate of revision in patients undergoing internal fixation versus arthroplasty for femoral neck fracture (4). Further analysis demonstrated that 17 conversion procedures can be prevented for every 100 patients treated with arthroplasty (4). Two large randomized control trials from Sweden echo the positive results of arthroplasty in hip fracture treatment. The first examined the short-term outcomes at the 2-year follow-up, finding patients that received primary arthroplasty treatment (hemi- or THA) had improved pain, functionality, and mobility. In additionally, these patients had a revision rate of 4% compared to 43% in the internal fixation group (5). When longer-term trends are examined, arthroplasty treatment once again offers improved clinical function and lower revision rates. At the 17-year follow-up, Chammout et al. (3) demonstrated decreased major revision surgery in the THA group and observed that the majority of failures in the internal fixation group occurred early (<2 years), while those in the arthroplasty group occurred later (>48 months). None of the patients in this long-term randomized trial had preexisting hip pain and all were over the age of 65. Furthermore, active older patients without significant medical co-morbidity do better with hemiarthroplasty/THA versus reduction and fixation (6).
There has been some belief that internal fixation is associated with lower cost when compared to arthroplasty options. Iorio et al. (7) however found that internal fixation was in fact the most expensive option. They performed a cost analysis for 2 years postoperative comparing internal fixation, unipolar, bipolar hemiarthroplasty and THA. Hospital admission, rehabilitation, and adjusted revision costs
were considered and demonstrated that cemented THA was the most cost-effective option ($20,670). Internal fixation meanwhile was found to be the least cost-effective of the cohorts examined ($24,606). Therefore due to positive long-term results and cost neutrality the use of arthroplasty (hemiarthroplasty or THA) should be strongly considered in older patients with femoral neck fracture.
were considered and demonstrated that cemented THA was the most cost-effective option ($20,670). Internal fixation meanwhile was found to be the least cost-effective of the cohorts examined ($24,606). Therefore due to positive long-term results and cost neutrality the use of arthroplasty (hemiarthroplasty or THA) should be strongly considered in older patients with femoral neck fracture.
The remainder of this chapter will focus on the indications, techniques, and literature pertaining to the use of arthroplasty for the treatment of femoral neck fractures. We will discuss hemiarthroplasty and THA for acute fracture treatment as well as explore the details surrounding conversion arthroplasty in revision settings.
Arthroplasty in Primary Fracture
The current literature clearly supports that elderly patients benefit from arthroplasty for the treatment of acute femoral neck fracture (3,4,5,6,7). The next decision the treating surgeon must make is whether a hemiarthroplasty (bipolar or monopolar) or THA would be most appropriate. Furthermore, one must determine the approach to be utilized; the type of fixation (cemented vs. uncemented); and the implant specifics such as head size, modularity, and bearing material to be used. Specific patient and fracture characteristics to consider have been presented by Zuckerman (8). Some general questions surgeons should consider when deciding on the treatment of acute femoral neck fracture must include the following:
What is the age of the patient?
What was/is the desired activity level of the patient?
Was there pre-existing hip pain?
What is the condition of the cartilage within the joint?
What bone stock is available for component fixation?
What are the patient’s medical co-morbidities?
What is the patient’s cognitive function?
Is there a pre-existing metabolic or neoplastic process present?
Hemiarthroplasty
Hemiarthroplasty can be divided into monopolar and bipolar designs. Regardless of modularity, issues that are common to these devices include infection, dislocation, loosening, and acetabular erosion or protrusio. While each of these complications can lead to persistent pain and poor outcomes, erosion of the acetabular cartilage and subchondral bone is a chief concern, especially in an active patient. Hemiarthroplasty was first introduced in the 1960s as a monopolar design. Despite issues with erosion, in some patients this may still be the appropriate surgical option. For the elderly, low-demand patient, a monopolar prosthesis can offer a stable and functional prosthesis that is relatively easy for the surgeon to implant. In addition, these components can typically be implanted in less OR time that bipolar or total hip designs which is an important consideration in the medically complicated patient. These implants often have larger head diameters which minimize the risk of dislocation; especially advantageous in the elderly patient with cognitive impairment. However, continued wear of the native acetabulum, with progressive erosion leading to pain, decreased functionality, and eventually protrusion are drawbacks of this implant. At the 2-year follow-up it has been shown that 55% of patients required conversion to THA. The most common reason for conversion was groin/buttock pain, thought to be related directly to acetabular wear (9).
In an attempt to alleviate the erosive patterns seen in the monopolar designs, bipolar hemiarthroplasty was introduced to the marketplace in the 1970s. With a second articulation within the implant itself, motion at the acetabular/implant interface should theoretically be lessened, leading to a decrease in acetabular erosion. Some 40 years after the introduction of this concept, the literature is still unclear as to whether or not bipolar designs reduce wear. Multiple randomized studies comparing bipolar to monopolar design have demonstrated conflicting results. Raia et al. (10) found that the in patients over the age of 65 years, the use of bipolar designs demonstrated no functional or quality of life improvements over monopolar designs at 1 year. However, Malhotra (11) found that bipolar hemiarthroplasty can offer improvements in ROM, pain, and a lower revision rate. A 2004 Cochrane Review examining 857 patients, enrolled in seven different randomized trials (12) found no difference in dislocation rate, acetabular erosion, reoperation rate, or mortality between unipolar and bipolar hemiarthroplasty. In patients with lower activity levels, advanced age, or medical comorbidities, monopolar implants are an acceptable choice for the treatment of acute femoral neck fracture. However, in patients with a longer life expectancy and higher activity levels most surgeons would recommend bipolar hemiarthroplasty or THA for treatment of acute femoral neck fracture.
Total Hip Arthroplasty
Controversy exists as to the precise indications for THA in femoral neck fracture. Some surgeons feel that pre-existing hip pain is a requisite; while others believe that THA decreases the risk of postoperative hip pain often seen in the setting of internal fixation or hemiarthroplasty. Figure 77.2 demonstrates a displaced femoral neck fracture in a 59-year-old patient with Parkinson disease. Despite the lack of radiographic findings consistent with osteoarthritis the patient was treated with THA and has been well postoperatively. Rogmark et al. (5) utilized a novel preoperative rating scale to stratify patients to receive either THA or hemiarthroplasty in their multicenter randomized trial. Patients were scored based on age, independent living, use of walking aids, and mental status. Those who scored greater than 14 received THA while patients scoring less than 14 were treated with hemiarthroplasty. Overall, patients who received THA based on this scoring system were younger, more independent, and ambulatory. The authors found no significant difference in complication rates between hemiarthroplasty and THA. Thus the Rogmark scoring system may assist surgeons in stratifying patients preoperatively.
Generally speaking, most complications (i.e., leg-length discrepancy, fixation compromise, and infection) associated with THA for fractures occur at a similar incidence to those in elective THA. In the setting of fracture however, instability is a concern. Literature shows dislocation occurs at a higher rate in THA’s after fracture, with early reports of nearly 10% to 20% (13,14,15). It is postulated that
an increased preoperative ROM (compared to that seen in the arthritic population) coupled with an alteration of proprioception after fracture are contributing factors. Not all authors however report such high dislocation rates. Rogmark et al. (5



an increased preoperative ROM (compared to that seen in the arthritic population) coupled with an alteration of proprioception after fracture are contributing factors. Not all authors however report such high dislocation rates. Rogmark et al. (5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree