Principles of Shoulder Rehabilitation
Benjamin D. Rubin MD, MS
The shoulder functions in the context of a kinetic chain, a series of links and segments activated sequentially in a coordinated fashion to generate and transmit force.
The axioscapular shoulder muscles, which attach the scapula to the thorax, include the serratus anterior, the trapezius, the rhomboids, and the levator scapulae posteriorly, and the pectoralis minor anteriorly.
The scapulohumeral shoulder muscle group consists of supraspinatus, infraspinatus, teres minor, subscapularis, deltoid, and teres major.
The axiohumeral muscles are the “power” muscles of the shoulder and include the pectoralis major and latissimus dorsi.
Abnormal scapular kinematics occur as a result of alterations in anatomy, physiology, and/or biomechanics; or musculoskeletal adaptations to these aberrations.
The goal of functional rehabilitation goes beyond resolving symptoms to regaining normal function by re-establishing normal anatomy, physiology, biomechanics, and kinematics, thus restoring the integrity of the kinetic chain.
The goal of successful shoulder rehabilitation following an injury or surgery is to establish normal function rather than to merely resolve symptoms. In order to accomplish this, restoration of the normal anatomy, physiology, and biomechanics of the shoulder, as well as correction of any associated musculoskeletal adaptations that have occurred, are necessary to re-establish the normal kinematics. To many, the concept of evaluating and treating the shoulder in the context of the musculoskeletal system, rather than in isolation, represents a paradigm shift from the more traditional approach. This chapter will address shoulder function and dysfunction, and in that light, address the concepts and specifics of core-based functional rehabilitation of the shoulder.
The shoulder functions in the context of a kinetic chain, which is defined as a series of links and segments activated sequentially in a coordinated fashion to generate and transmit forces to accomplish a specific function (1,2,3). This can easily be understood by remembering the mechanics of the childhood game “crack the whip,” when a group of children holds hands in a line to try to increase the speed of the last child. The first child forms the base and whips the second child, who whips the third, thus transmitting the force and velocity, which are sequentially passed on until the final child is maximally accelerated. Each child represents a segment of the chain, and their joined hands represent links in the chain. In activities that utilize a throwing motion, (e.g., pitching or tennis), there is an open-ended kinetic chain with proximal to distal muscle activation and coordination of body segments producing interactive moments at the terminal segment (hand or racket) (4,5). In throwing, the sequence of link activation begins with the creation of a ground reaction force as a result of the foot and leg pushing against the ground. The force is increased as it is transmitted through the knees and hips through the large muscles of the
legs, into the lumbopelvic region and the rest of the trunk. The proximal segments, i.e., the legs and trunk, produce roughly half the energy (51%) and force (54%) that is ultimately delivered to the distal end of the kinetic chain (6,7,8). The scapula and glenohumeral joint function as both a link and a segment in the kinetic chain, increasing the kinetic energy and force generated; and as a conduit to funnel and transmit these forces to the distal segments (9).
legs, into the lumbopelvic region and the rest of the trunk. The proximal segments, i.e., the legs and trunk, produce roughly half the energy (51%) and force (54%) that is ultimately delivered to the distal end of the kinetic chain (6,7,8). The scapula and glenohumeral joint function as both a link and a segment in the kinetic chain, increasing the kinetic energy and force generated; and as a conduit to funnel and transmit these forces to the distal segments (9).
When an individual reaches, pushes, or pulls from a sitting position, there is less energy and force contribution from the legs, and the primary generator for upper-extremity motion is the initiation of trunk stabilization. Hodges has shown that before either arm or leg movement is initiated, the transverses abdominis is consistently activated first, increasing the intra-abdominal pressure in preparation of the action (10). Coordinated muscle activation sequences result in movement patterns, which create joint motions to efficiently accomplish specific tasks. These diagonal activation patterns create a “serape” effect from the knee or lumbopelvic region to the shoulder (11), act locally on one joint or harmonize several joints, provide co-contraction force couples that control joint perturbations and provide stability, and generate and transmit force. This enables the scapular stabilizing muscles to position the scapula optimally for shoulder function and for the rotator cuff to compress and position the humeral head in the glenoid fossa.
The Scapula in Shoulder Function
The scapula provides both anatomic and kinematic connections between the torso and the upper extremity. The shoulder muscles can be classified anatomically by their origins and insertions into the axioscapular, scapulohumeral, and the axiohumeral groups (12). The axioscapular muscles, which attach the scapula to the thorax, include the serratus anterior, the trapezius, the rhomboids, and the levator scapulae posteriorly, and the pectoralis minor anteriorly. These scapular stabilizing muscles position the scapula optimally for the humeral head. In the case of the serratus anterior and the trapezius, the muscles are so large and the muscle fibers course in different directions; therefore, each muscle may have multiple functions that relate to activity and arm position (13).
The scapulohumeral group consists of the supraspinatus, infraspinatus, teres minor, subscapularis, deltoid, and teres major. The rotator cuff muscles provide concavity/compression at the glenohumeral joint and fine tune humeral head rotation and depression, thus keeping the humeral head centered in the glenoid throughout the arc of upper-extremity motion. The axiohumeral muscles are the “power” muscles of the shoulder and include the pectoralis major and latissimus dorsi. The biceps and triceps comprise a special category, because they extend from the scapula to the forearm.
The shoulder is an important kinematic link between the trunk and arm, providing a stable platform for arm rotation during throwing. The shoulder includes the scapulothoracic articulation and the glenohumeral, acromioclavicular, and sternoclavicular joints, which together form two individual but paired mechanisms—one an open chain and one a closed chain (14). A closed kinetic chain, such as the one formed by the thorax, scapula, and clavicle is defined by the terminal link being fixed or immovable. The open kinetic chain mechanism, i.e., the glenohumeral joint, involves movement of the terminal link, which is the hand. Normal function requires that all four articulations participate in a simultaneous, synchronous, and coordinated manner, as well as in succession, creating what is termed scapulohumeral rhythm (15).
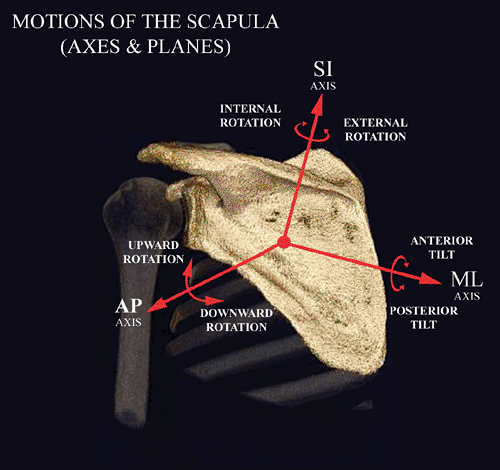
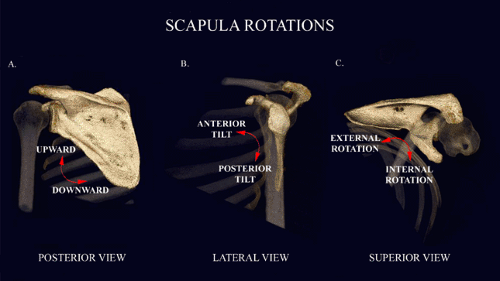
Every movement of the scapula involves six degrees of freedom of motion, which involves three rotations and three translations along three orthogonal axes (Fig 22-1). The medial-lateral axis is parallel to the spine of the scapula; the superior-inferior (vertical) axis is perpendicular to the transverse plane; and the anterior-posterior axis is perpendicular to the coronal plane. This six degrees of freedom motion of the scapula can be quite complex and confusing from a biomechanical perspective; therefore, for clinical purposes, the most dominant kinematic parameter for each functional motion is described below. The motions include anterior/posterior tilt (rotation on the sagittal plane about a medial-lateral axis—Fig 22-2A), internal and external rotation (rotation on the transverse plane about a vertical axis—Fig 22-2B), and upward and downward rotation (rotation on the coronal plane about an anterior-posterior axis—Fig 22-2C). Scapular translations are elevation/depression (translation along the vertical axis), abduction/adduction (translation along the medial-lateral axis), and anterior-posterior movement (translation along the anterior-posterior axis). Protraction and retraction, which are terms frequently used in the clinical setting, represent combinations of motions and translations to describe scapular movements and are dependent on the rotation of an intact clavicle about the sternoclavicular joint. Protraction, a movement frequently associated with shoulder dysfunction, involves anterior movement, anterior tilt, and upward rotation. During glenohumeral elevation, the normal scapula demonstrates a pattern of upward rotation, external rotation, and posterior tilting (16). The predominant motion is upward rotation, and to a lesser degree external rotation and posterior tilt. In addition, the scapula translates into a more superior and posterior position (16). Dynamic scapulohumeral rhythm depends on scapular motions and translations, combined with arm motion.
The scapular stabilizing muscles function as force couples to control the motions of the scapula. A force couple is formed when two forces act in opposite directions to impose rotation about an axis (17). The serratus anterior controls the movements of protraction and retraction (abduction and adduction), depending on shoulder position (18). This is counteracted by the upper and lower trapezius and the rhomboids, which act as retractors (adductors). Scapular
elevation is a function of the upper trapezius, the levator scapula, and the upper serratus anterior. This is balanced by the scapular depression resulting from the function of the lower portions of the trapezius and serratus anterior (12,13,18,19).
elevation is a function of the upper trapezius, the levator scapula, and the upper serratus anterior. This is balanced by the scapular depression resulting from the function of the lower portions of the trapezius and serratus anterior (12,13,18,19).
The Scapula in Shoulder Dysfunction
Abnormal scapular kinematics occur as a result of alterations in anatomy, physiology, and/or biomechanics, or musculoskeletal adaptations to these aberrations, and can usually be classified
as being proximally or distally derived (Table 22-1) (20). When the basic problem occurs proximal and posterior to the glenohumeral joint, the observed scapular dyskinesis is considered proximally derived (PDSD). When an abnormality of the glenohumeral joint, subacromial space, clavicle, acromioclavicular or sternoclavicular joints occurs, the resulting dyskinesis that is usually observed is considered distally derived (DDSD). The exception to this classification is the presence of shortening or tightness of the pectoralis minor or clavipectoral fascia, which fits best into PDSD despite its anterior position. Recently, Borstad and Ludewig (21) have documented the effect of altered pectoralis minor resting length on scapular kinematics in healthy individuals. In the context of the kinetic chain, PDSD is associated with proximal link or segment weakness or interruption, while DDSD is the result of “recoil” or “kick back” from a distal link or segment dysfunction. This has important implications in the treatment of shoulder and upper-extremity conditions. The pattern of abnormal scapular motion is usually multi-planar and frequently changes with the plane of arm elevation, concentric or eccentric function of the scapular stabilizers, and fatigue; however, if scapular dyskinesis is observed, the sensitivity of the observation is 0.74 and the positive predictive value is 0.84 (22).
as being proximally or distally derived (Table 22-1) (20). When the basic problem occurs proximal and posterior to the glenohumeral joint, the observed scapular dyskinesis is considered proximally derived (PDSD). When an abnormality of the glenohumeral joint, subacromial space, clavicle, acromioclavicular or sternoclavicular joints occurs, the resulting dyskinesis that is usually observed is considered distally derived (DDSD). The exception to this classification is the presence of shortening or tightness of the pectoralis minor or clavipectoral fascia, which fits best into PDSD despite its anterior position. Recently, Borstad and Ludewig (21) have documented the effect of altered pectoralis minor resting length on scapular kinematics in healthy individuals. In the context of the kinetic chain, PDSD is associated with proximal link or segment weakness or interruption, while DDSD is the result of “recoil” or “kick back” from a distal link or segment dysfunction. This has important implications in the treatment of shoulder and upper-extremity conditions. The pattern of abnormal scapular motion is usually multi-planar and frequently changes with the plane of arm elevation, concentric or eccentric function of the scapular stabilizers, and fatigue; however, if scapular dyskinesis is observed, the sensitivity of the observation is 0.74 and the positive predictive value is 0.84 (22).
TABLE 22-1 Causes of Scapular Dyskinesis | |
|---|---|
|
PDSD is frequently associated with postural dysfunction. The classic presentation is that of the patient who sits or stands with the head and neck in a forward position, with focal cervical lordosis (usually at C5-C6), thoracic kyphosis, and protracted scapulae (23). Lumbar lordosis with poor control of the abdominal musculature is frequently associated. Proximal kinetic chain weakness can be due to abnormalities of the lower extremities, lumbopelvic, lumbar, or thoracolumbar deficits. Lumbopelvic weakness appears to be one of the most common causes of primary scapular dyskinesis in the throwing athlete (11). Injury to either the long thoracic nerve or spinal accessory nerve causes weakness and atrophy of the serratus anterior and trapezius, respectively. Long thoracic stretch mononeuropathy is actually more common in overhead athletes than previously thought, and recently has been associated with the use of heavy backpacks by children and young adults (backpack palsy). When these muscles are compromised either from neurologic interruption or fatigue, force couple imbalances ensue, and a significant adverse cascade of events occurs (Fig 22-3). Proprioception is altered, a dyssynchronous muscle firing pattern occurs, with an abnormal increase in scapular mobility (usually loss of external rotation) and subsequent increased stress on the glenohumeral joint capsule, glenoid labrum, and rotator cuff (24,25,26,27,28). Increased protraction has been shown to specifically increase the strain on the anterior band of the inferior glenohumeral ligament and decrease anterior translation of the humeral head (28). As indicated in the discussion above concerning the role of the scapula as a kinematic link between the trunk and the arm, optimum rotator cuff activation occurs only in the presence of a scapula that is optimally positioned for stability (27). As a result, increased intrinsic joint loads and decreased force are delivered to the terminal segment (4).
DDSD is very common. Almost all shoulder pathology is associated with alterations in the ability to position the scapula properly, usually quite early in the pathologic process (8,27,29,30,31,32,33,34,35,36,37,38). Related intra-articular pathology may include labral tears or detachments and capsular attenuation or tears (with resultant instability), focal capsular restrictions such as glenohumeral internal rotation deficit (GIRD), which is commonly seen in overhead athletes, biceps lesions, adhesive capsulitis, and glenohumeral arthritis. Rotator cuff tendonitis and tears, primary impingement syndrome, and calcific tendonitis have been observed to be associated with scapular malposition. In these cases, the pain and altered biomechanics associated with the pathology causes inhibition of the serratus anterior and lower trapezius, with the subsequent events outlined earlier. This results in the vicious cycle of scapular dysfunction and shoulder pathology summarized in Figure 22-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree