Principles of Diagnosis and Treatment
John A. Feagin Jr.
Part I of The Crucial Principles is devoted to principles of diagnosis and treatment of the knee-injured patient. These principles are illustrated in three key case studies (see Chapter 3).
The skills necessary for the diagnosis and treatment of knee ligament injuries are hard-earned and are the result of a never-ending quest for excellence. These skills are passed from generation to generation, perhaps more through the spoken word than through our texts. These skills form the basis of good judgment and become sources of unending pride.
One of the great teachers of orthopaedics had this to say:
Accurate diagnosis, the essential preliminary to appropriate treatment, is difficult because the diagnostic pathway is beset by tripwires. A detailed history of the injury is seldom obtainable; the most complete ligamentous and capsular disruptions are often the least painful because the sensory nerve fibers also are torn, and sometimes they are the least swollen (because the torn capsule allows the effusion to leak away). Moreover, even an innocent radiograph can be misleading, because a ligament whose substance is torn is more difficult to repair than that which has avulsed its bony attachment. For all these reasons and because the initial physical assessment may determine the entire future athletic life of the patient, the initial examination must be both meticulous and systematic.*
It would be impossible to acknowledge all who, like A. Graham Apley, have guided me with their wisdom and philosophy. Readers will get to know these mentors of mine in this book or in the selected bibliography. The bibliography is a collection of readings from colleagues the world over whose contributions form the core of science and experience that is fundamental to the care of the knee.
The information and philosophy presented under this chapter title, “Principles of Diagnosis and Treatment,” should be kept in mind while reading the case studies. References accompany each case study. Also, within the case study, the reader may be referred to other chapters within the text.
History and Mechanisms of Trauma
In athletic trauma, the history is usually quite straightforward and the patient usually is aware of the details and circumstances. This is a luxury not always found in the other fields of trauma. In obtaining the history, the physician should elicit from the patient the history of previous injury or dysfunction and the mechanism of injury. Also, the patient may tell the physician about the swelling (immediate or delayed), the pain, and the ability to continue participation in daily activities or athletics.
History of Previous Injury
Is the injury truly acute or was there a previous laxity or disability? Too often, the athlete “forgets” that the knee was previously injured. Once reminded, the athlete can usually offer the details. These details take on added meaning when the radiographic films are reviewed, as one seeks evidence of old injuries through osteophyte formation.
Simple as it is, the history can be a useful diagnostic tool. In fact, in my experience, deceleration, cutting injuries that are associated with a pop and with the gradual onset of effusion during the ensuing 24 hours will prove in 85% of cases to be an anterior cruciate ligament (ACL) injury. Because an ACL tear is seldom an isolated injury, the examiner’s task is to verify the ACL tear and seek out associated injuries through the physical examination.
Mechanism of Injury
The mechanism of injury alerts the physician to which ligaments were at risk in the knee. In Case Study 2, the mechanism of injury is a change of direction involving deceleration with the foot fixed and contact with another player. This classic injury of American football is often called the O’Donoghue triad—a tear of the ACL, the medial collateral ligament (MCL), and the medial meniscus.
As shoe/turf and ski/boot fixation devices have become more efficient, we now often see injuries caused by deceleration and change of direction that do not involve contact with another player. This type of injury is associated with a “pop,” the inability to continue “play,” and the onset during the next 24 hours of a relatively tense effusion. This mechanism was initially associated with the “isolated tear of the ACL,” but with time and sophistication, it has become clear that there is seldom an isolated ligamentous injury to the knee. The knee is a harmonius symphony of ligaments, in which no ligament stands alone.
Another mechanism of injury, which occurs predominantly in the skier, is an abrupt contraction by the quadriceps to regain balance—similar to a powerful Lachman test—which pulls the tibia forward on the femur and tears the ACL. This injury may not even be associated with a fall.
There are other mechanisms of injury, but these three predominate and will serve the clinician well:
Contact with another player and change of direction and deceleration with fixed foot.
No contact with a player, but change of direction and deceleration.
Abrupt contraction of the quadriceps to regain balance.
Pain
Many patients are able to walk off the field or ski down a slope after a severe ligamentous injury. Pain is certainly a characteristic of these injuries, but perhaps the feeling of subluxation is more ominous and limiting to the patient. A tried-and-true dictum of ligament injury is that the more pain, the less severe the injury. It is probable that a complete tear so disrupts the nerve fibers that the pain is less severe. Certainly, in a complete tear, one can “open” the joint more readily with less discomfort to the patient.
Pop
The pop is characteristic of a tear of the ACL. We know from Biomechanical studies that the helicoid arrangement of the ACL allows it to store considerable energy before its elastic limit is reached. As a result, when the elastic limit is reached, the ligament bursts convulsively, and the patient defines this sensation as “a pop.”
The pop is the part of the history that most reliably indicates an ACL tear. Neither the MCL nor the capsuloligamentous structures tear with this pop, perhaps because they have broader origins and insertions and are generally flattened rather then helicoid. At any rate, the pop is characteristic of a tear of the ACL. It has been my experience that few people will continue to play after sustaining a complete ACL tear. If they do continue, a more extensive injury may result, that is, subluxation of the tibia on the femur with increased structural damage.
Onset of Swelling
The onset and amount of swelling is an important diagnostic clue. Swelling that can be appreciated by physical examination is often delayed 6 to 24 hours. In the case of the ACL, the artery, a branch of the posterior geniculate, is not substantial and is easily tamponaded. In the surgical care of acute cases, blood has been seen to “drip much like a leaky faucet.” This explains the slow accumulation of the effusion. If the effusion is contained by the capsular mechanism, then it will reach maximum within 12 to 24 hours. If, however, a lesion of the capsule coexists with the ACL injury, the effusion may be slight because the fluid escapes through a rent in the capsuloligamentous structure.
If effusion develops immediately after injury, one should suspect an osteochondral fracture. Bleeding into the joint is more brisk with an osteochondral fracture than with a torn ACL; this distinction is a subtle diagnostic clue. The fluid is usually aspirated because its character and the presence or absence of fat are important diagnostic signs.
Principles of Physical Examination
The specific ligamentous injury is sought primarily by comparing the excursion of the tibia on the femur in the injured and uninjured knee. This is done by imparting stress through a range of motion. This can be quite precise, particularly if the clinician can get the patient to relax while the well leg is examined first. Using the well leg as a standard for comparison is a must.
The position of comfort for the patient is frequently the position in which the patient is found. I prefer to begin the examination with the patient in this position. The initial examination can be particularly revealing when it occurs before the onset of effusion and muscle spasm. A single examination is not always definitive. Re-examination is essential and appropriate.
Sometimes a change in venue will help both physician and patient to relax and will result in a more productive physical examination. Ice is a useful adjunct to the physical examination as it decreases pain and promotes relaxation. The sideline is often not conducive to meticulous attention to detail required by both patient and examiner. A change of venue and circumstances may be advantageous and should be determined by the examiner.
Inspection—Look!
The injured knee must be considered in the context of the entire patient. The patient’s physiologic age, body fat, and muscle mass reflect his or her previous selection of activities. I consider these to be key observations during the physical examination. The brachioradialis and gastrocsoleus are excellent muscles to observe because they are seldom developed by adult activity and thus reflect the activities of youth.
Besides the knee, the leg as a whole should be inspected. Is the skin intact? Are there abrasions, old scars, or bruising? The skin may give information about the direction, force, and mechanism of injury and the history. The alignment of the lower limb segments and any atrophy or swelling should be noted. These observations lead to the laying on of the hands—palpation.
Palpation—Feel!
The hands of the skilled examiner are a wonderful arthrometer. The palpatory examination of the knee involves a subtle gradient of force application. The initial laying on of the hands is performed on the normal side with only sufficient pressure to feel the subtleties of the knee’s form. This complements the visual inspection. When the form is ascertained, more pressure is applied to distinguish induration—the firmness of the tissue planes. Induration often is the clue to the severity as well as the site of injury. Gentle flexion of the knee, where possible, is helpful during this search for induration because it may separate some of the anatomic structures and help to localize more precisely the sites of injury.
Finally, palpation is conducted with slightly more vigor to identify tenderness. This must be performed with the patient’s full knowledge and cooperation, and the patient must appreciate the precision with which this portion of the examination can be conducted. Gentleness is the key to this precision.
Problems left unattended within the knee do not become easier with the passage of time. Initial subtleties become blunted by induration, edema, and effusion, which develop days after injury. One misses important details by not examining the knee-injured patient shortly after the injury occurs.
Movements—Move!
Should the examiner begin with active or passive movements? I prefer to ask the patient to move the well leg within the range of motion that is comfortable and possible. This gives a standard of comparison for the injured leg. Then I ask the patient to move the injured extremity within the bounds of comfort. This shows the range of motion available to position the leg for the ligamentous examinations.
Flexion/Extension
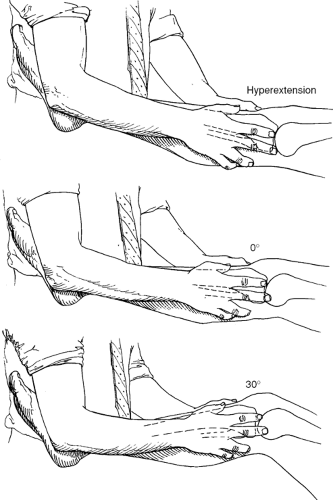
One of the goals of movement is to place the extremity in the optimum position for isolating and examining the different ligamentous structures. If hyperextension can be achieved, it is a good position to begin. If the knee is stable in hyperextension, the medial and lateral capsuloligamentous structures and the posterior cruciate ligament (PCL) are intact. Thus, the maximum amount of information is gained quickly. The collateral ligaments are best examined
at hyperextension, neutral, and 30 degrees flexion (Fig. 2.1). The technique that Smillie (I. Smillie, Dundee, Scotland, personal communication, 1972) taught me still seems the most useful—the patient’s foot is loosely constrained against the examiner’s hip so both hands are free to palpate the joint lines and ligamentous structures.
at hyperextension, neutral, and 30 degrees flexion (Fig. 2.1). The technique that Smillie (I. Smillie, Dundee, Scotland, personal communication, 1972) taught me still seems the most useful—the patient’s foot is loosely constrained against the examiner’s hip so both hands are free to palpate the joint lines and ligamentous structures.
Varus/Valgus Angulation
Laxity in hyperextension to varus or valgus angulation is an ominous sign that indicates disruption of key ligamentous structures. If in hyperextension the joint is lax to valgus angulation, the medial capsuloligamentous structures and the PCL are probably interrupted. If in hyperextension, the knee is lax to varus angulation, the arcuate complex and PCL are probably disrupted. When varus and valgus are applied with the knee at 0 degrees of flexion, the ACL and PCL are slackened sufficiently that these tests are diagnostic of medial or lateral capsular injuries. At 30 degrees of flexion, the cruciate ligaments are in their most relaxed state, and pathologic laxity palpated is capsular laxity.
Anteroposterior Glide—The Lachman or Drawer Test
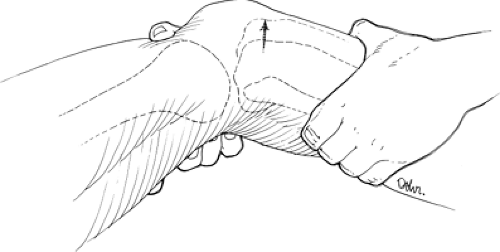
The essence of the physical examination is an appreciation of pathologic excursion of the tibia with respect to the femur. Anteroposterior (AP) glide is a particularly sensitive test, but may be misinterpreted if the relation of the tibia to the femur is not understood and the test is started in the wrong place.
This misinterpretation most frequently occurs when the test is begun with the tibia inadvertently posteriorly subluxated on the femur. AP glide is best determined with the fingers measuring the translation of the tibia on the femur in an AP direction (Fig. 2.2). The fingers are quite accurate arthrometers, although perhaps often undertrained (see Chapter 1).
This misinterpretation most frequently occurs when the test is begun with the tibia inadvertently posteriorly subluxated on the femur. AP glide is best determined with the fingers measuring the translation of the tibia on the femur in an AP direction (Fig. 2.2). The fingers are quite accurate arthrometers, although perhaps often undertrained (see Chapter 1).
Rotation
The appreciation of increased rotatory excursion requires careful attention to detail. With the hip and knee flexed 90 degrees, internal and external rotation stress are applied first to the well and then to the injured leg (Fig. 2.3). This test can give quite meaningful information on the status of the cruciate ligaments, as well as the complementary medial and lateral capsuloligamentous structures. I have found this test particularly useful to determine the envelope of motion.
Combined Anteroposterior Glide and Rotation
The pivot shift test is a combination of translation and rotation (Fig. 2.4). This test has been eloquently described by Losee et al.1 and is referred to in Case Study 1 (see Chapter 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree