Essentials of Diagnosis
- Sjögren syndrome (SjS) is a systemic autoimmune disease that presents with sicca symptomatology of mucosal surfaces.
- The main sicca features (xerophthalmia and xerostomia) are determined by specific ocular (rose bengal staining and Schirmer test) and oral (salivary flow measurement and parotid scintigraphy) tests.
- The histologic hallmark is a focal lymphocytic infiltration of the exocrine glands, determined by a biopsy of the minor labial salivary glands.
- The spectrum of the disease includes systemic features (extraglandular manifestations) in some patients, and may be complicated by the development of lymphoma.
- Patients with SjS present a broad spectrum of analytic features (cytopenias, hypergammaglobulinemia, and high erythrocyte sedimentation rate) and autoantibodies, of which antinuclear antibodies are the most frequently detected, anti-Ro/SS-A the most specific, and cryoglobulins and hypocomplementemia the main prognostic markers.
General Considerations
Sjögren syndrome (SjS) is a systemic autoimmune disease that mainly affects the exocrine glands and usually presents as persistent dryness of the mouth and eyes due to functional impairment of the salivary and lacrimal glands. An estimated 2–4 million persons in the United States have SjS, of whom approximately 1 million have established diagnoses. The prevalence in European countries ranges between 0.60% and 3.3%. The incidence of SjS has been calculated as 4 cases per 100,000. SjS primarily affects white perimenopausal women, with a female:male ratio ranging from 14:1 to 24:1 in the largest reported series. The disease may occur at all ages but typically has its onset in the fourth to sixth decades of life. When sicca symptoms appear in a previously healthy person, the syndrome is classified as primary SjS. When sicca features are found in association with another systemic autoimmune disease, most commonly rheumatoid arthritis, systemic sclerosis, or systemic lupus erythematosus, it is classified as associated SjS.
Major clinical manifestations are summarized in Table 26–1. Although most patients present with sicca symptoms, there are various clinical and analytic features that may indicate undiagnosed SjS (Table 26–2). The variability in the presentation of SjS may partially explain delays in diagnosis of up to 10 years from the onset of symptoms. SjS is a disease that can be expressed in many guises depending on the specific epidemiologic, clinical, or immunologic features. The management of SjS is centered mainly on the control of sicca features, using substitutive and oral muscarinic agents. Glucocorticoids and immunosuppressive agents play a key role in the treatment of extraglandular features.
| Organ | Manifestations |
|---|---|
| Mouth | Oral dryness (xerostomia), soreness, caries, periodontal disease, oral candidiasis, parotid swelling |
| Eyes | Ocular dryness (xerophthalmia), corneal ulcers, conjunctivitis |
| Nose, ear, and throat | Nasal dryness, chronic cough, sensorineural hearing loss |
| Skin | Cutaneous dryness, palpable purpura, Ro-associated polycyclic lesions, urticarial lesions |
| Joints | Arthralgias, nonerosive symmetric arthritis |
| Lungs | Obstructive chronic pneumopathy, bronchiectasis, interstitial pneumopathy |
| Cardiovascular | Raynaud phenomenon, pericarditis, autonomic disturbances |
| Liver | Associated hepatitis C virus infection, primary biliary cirrhosis, type 1 autoimmune hepatitis |
| Nephro-urologic | Renal tubular acidosis, glomerulonephritis, interstitial cystitis, recurrent renal colic |
| Peripheral nerve | Mixed polyneuropathy, pure sensitive neuronopathy, mononeuritis multiplex, small-fiber neuropathy |
| Central nervous system | White matter lesions, cranial nerve involvement (V, VIII, and VII), myelopathy |
| Thyroid | Autoimmune thyroiditis |
| General symptoms | Low-grade fever, generalized pain, myalgias, fatigue, weakness, fibromyalgia, polyadenopathies |
|
Clinical Findings
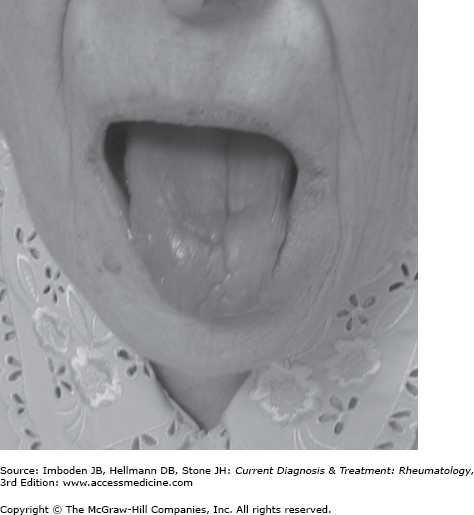
Xerostomia, the subjective feeling of oral dryness, is the key feature in the diagnosis of primary SjS, occurring in more than 95% of patients. Other oral symptoms may include soreness, adherence of food to the mucosa, and dysphagia. Reduced salivary volume interferes with basic functions such as speaking or eating. The lack of salivary antimicrobial functions may accelerate local infection, tooth decay, and periodontal disease. Xerostomia can lead to difficulty with dentures and the need for expensive dental restoration, particularly in elderly patients. Various oral signs may be observed in SjS patients. In the early stages, the mouth may appear moist, but as the disease progresses, the usual pooling of saliva in the floor of the mouth disappears. Typically, the surface of the tongue becomes red and lobulated, with partial or complete depapillation (Figure 26–1). In advanced disease, the oral mucosa appears dry and glazed and tends to form fine wrinkles. Angular cheilitis, erythematous changes of the hard palate, and a red tongue with atrophic papillae strongly suggest Candida infection.
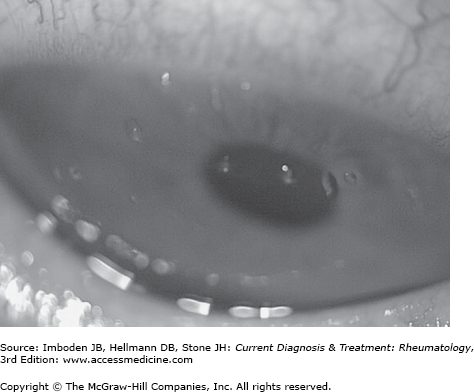
The subjective feeling of ocular dryness is associated with sensations of itching, grittiness, soreness, and dryness, although the eyes have a normal appearance. Other ocular complaints include photosensitivity, erythema, eye fatigue, or decreased visual acuity. Environmental irritants such as smoke, wind, air conditioning, and low humidity may exacerbate ocular symptoms. Diminished tear secretion may lead to chronic irritation and destruction of corneal and bulbar conjunctival epithelium (keratoconjunctivitis sicca). In severe cases, slit-lamp examination may reveal filamentary keratitis, marked by mucus filaments that adhere to damaged areas of the corneal surface (Figure 26–2). Tears also have inherent antimicrobial activity and SjS patients are more susceptible to ocular infections such as blepharitis, bacterial keratitis, and conjunctivitis. Severe ocular complications may include corneal ulceration, vascularization, and opacification.
Reduction or absence of respiratory tract glandular secretions can lead to dryness of the nose, throat, and trachea resulting in persistent hoarseness and chronic, nonproductive cough. Likewise, involvement of the exocrine glands of the skin leads to cutaneous dryness. In female patients with SjS, dryness of the vagina and vulva may result in dyspareunia and pruritus, affecting their quality of life.
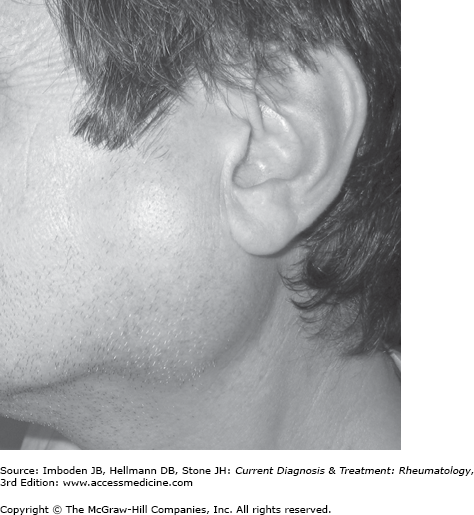
Chronic or episodic swelling of the major salivary glands (parotid and submandibular glands) is reported in 10–20% of patients and may commence unilaterally, but often becomes bilateral (Figure 26–3).
Patients with primary SjS often have general symptomatology, including fever, polyadenopathies, generalized pain, fatigue, weakness, sleep disturbances, anxiety, and depression, which may have a much greater impact on the quality of life of patients than sicca features. Low-grade fevers may occur in SjS, usually in young patients with positive immunologic markers. Fatigue, generalized pain, and weakness are among the most debilitating clinical features of primary SjS. The coexistence of primary SjS with a defined fibromyalgia is reported often.
Joint involvement, primarily generalized arthralgias, is seen in 25–75% of patients. Less frequently, joint disease presents as an intermittent symmetric arthritis primarily affecting small joints. Joint deformity and mild erosions are rare, except for those cases associated with rheumatoid arthritis. Clinical myopathy is rare but myalgias are frequently observed, and a recent study reported that subclinical muscular inflammation is often observed.
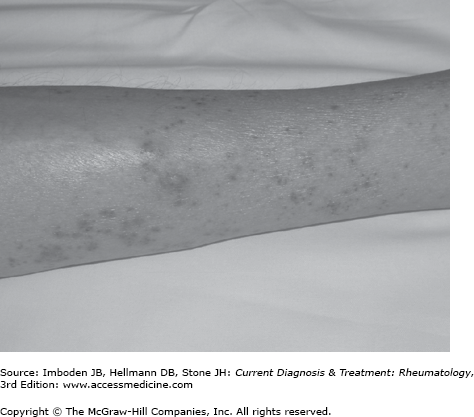
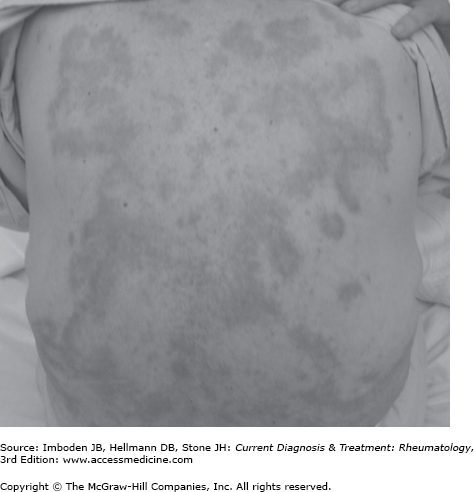
Although the main cutaneous manifestation of patients with primary SjS is skin dryness, a wide spectrum of cutaneous lesions may be observed, the most frequent of which is a small-vessel vasculitis, overwhelmingly leukocytoclastic. The skin findings include palpable purpura (Figure 26–4), urticaria, and erythematous macules or papules, and are associated with cryoglobulins in 30% of patients. Life-threatening vasculitis is also closely related to cryoglobulinemia.
Primary SjS patients may also have nonvasculitic cutaneous lesions. Some patients with anti-Ro/SS-A antibodies may present with polycyclic, photosensitive cutaneous lesions (Figure 26–5), clinically identical to the so-called annular erythema described in Asian SjS patients and subacute cutaneous lupus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree