Essentials of Diagnosis
- Microscopic polyangiitis (MPA) is the most common cause of the pulmonary-renal syndrome of alveolar hemorrhage and glomerulonephritis.
- Usually includes combinations of two or more of the following:
- Nonspecific constitutional symptoms, including fatigue, myalgias, weight loss, and fevers.
- Migratory arthralgias or arthritis, either pauciarticular or polyarticular.
- Palpable purpura, sometimes with skin ulcerations.
- Sensorimotor mononeuritis multiplex.
- Alveolar hemorrhage associated with hemoptysis and respiratory compromise.
- Glomerulonephritis.
- Nonspecific constitutional symptoms, including fatigue, myalgias, weight loss, and fevers.
- Antineutrophil cytoplasmic antibodies (ANCAs) are often critical in making the diagnosis, but a significant minority of patients are ANCA-negative.
- The majority of patients with MPA who are ANCA positive have antibodies directed against myeloperoxidase (MPO-ANCA).
- ANCA titers are often elevated during disease flares but do not have a consistent temporal relationship with disease activity. Thus, ANCA titers are not reliable predictors of disease flares.
General Considerations
Microscopic polyangiitis (MPA) is a form of systemic vasculitis that may affect many major organs with crippling or fatal effects. Seventy percent of patients with MPA have antineutrophil cytoplasmic antibodies (ANCAs). MPA is recognized to be related to both granulomatosis with polyangiitis (GPA; formerly Wegener granulomatosis) and eosinophilic granulomatosis with polyangiitis (EGPA; the Churg-Strauss syndrome) (see Chapters 32 and 34). These disorders are sometimes considered together as the ANCA-associated vasculitides, but important differences exist among these three conditions and significant percentages of patients with these diagnoses do not have ANCA.
MPA has been recognized increasingly since the first Chapel Hill Consensus Conference on the nomenclature of systemic vasculitides, the results of which were published in 1994. Many cases before then were considered to be forms of polyarteritis nodosa (PAN), a disease with which MPA shares substantial overlap. Table 33–1 compares the features of MPA with those of GPA (Wegener) and PAN.
| MPA | GPA | PAN | |
|---|---|---|---|
| Vessel size | Small to medium | Small to medium | Medium |
| Vessel type | Capillaries, venules, and arterioles; sometimes arteries and veins | Capillaries, venules, and arterioles; sometimes arteries and veins | Muscular arteries |
| Granulomatous inflammation | No | Yes | No |
| Lung involvement | Yes (pulmonary capillaritis) | Yes (pulmonary nodules, often cavitary) | No |
| Glomerulonephritis | Yes | Yes | No |
| Renin-mediated hypertension | No | No | Yes |
| ANCA-positive | 75% | 60–90% | No |
| Hepatitis B association | No | No | Yes (<10% of cases now) |
| Microaneurysms | Rarely | Rarely | Typically |
| Mononeuritis multiplex | Commonly (60%) | Occasionally | Commonly (60%) |
| Likelihood of disease recurrence | 33% | >50% | ≤10% |
The term “polyangiitis” is preferred to “polyarteritis” for MPA because of the disease’s tendency to involve veins as well as arteries. The first Chapel Hill Consensus Conference defined MPA as a process that (1) involves necrotizing vasculitis with few or no immune deposits; (2) affects small blood vessels (capillaries, arterioles, or venules) and possibly medium-sized vessels; and (3) demonstrates a tropism for the kidneys and lungs. With an estimated incidence of 4 cases per million per year, MPA is more common than classic PAN but somewhat less common than GPA (Wegener).
MPA occurs in people of all ethnic backgrounds. The male:female ratio is approximately 1:1. The typical patient is middle-aged to elderly, but the disease may affect people of all ages. The mean age at diagnosis for MPA patients (approximately 60 years) is about 10 years older than the mean age of GPA (Wegener) patients at diagnosis. Several epidemiologic studies have tried to elucidate environmental factors associated with the onset of vasculitis. Some authors have found associations with silica and solvent exposure.
The strongest link between an exposure and MPA relates to the use of propylthiouracil (PTU) for the treatment of hyperthyroidism (a handful of other drugs for other indications have also been implicated, but not as strongly). Anti-MPO antibodies are detected frequently in PTU-treated patients, albeit overt vasculitis occurs in only a small minority (<5%). Drug-induced, ANCA-associated vasculitis is discussed further in Chapter 42).
Clinical Findings
The interval between the onset of first disease symptoms and diagnosis in MPA is substantially shorter than for patients with GPA (Wegener). This is because of the tendency for GPA (Wegener) to smolder in the upper respiratory tract and cause apparently mundane symptoms for months before leading to medical attention. In contrast, the clinical presentation of MPA is usually more obvious at the time the patient becomes aware of symptoms: cutaneous vasculitis, vasculitis neuropathy, or alveolar hemorrhage. Nevertheless, subtle and subacute presentations of MPA are known to occur, and the range of organ system manifestations is extensive.
Although MPA is classified appropriately as a “pulmonary-renal syndrome,” regarding this disorder exclusively as a disease that affects the kidneys and lungs is a major potential clinical error. The five most common clinical manifestations of MPA are glomerulonephritis (nearly 80% of patients), weight loss (>70%), mononeuritis multiplex (60%), fevers (55%), and cutaneous vasculitis (>60%). Alveolar hemorrhage, in contrast, occurs in only about 12% of patients. The major clinical manifestations of MPA are shown in Table 33–2.
| Organ | Manifestation |
|---|---|
| Constitutional | Weight loss, anorexia, fevers |
| HEENT | Rhinitis, tongue or other oral ulcers; occasional purpuric lesions on palate; ocular inflammation (eg, sclerouveitis) reported but rare |
| Lungs | Alveolar hemorrhage; nonspecific infiltrates; pulmonary fibrosis; pleural effusions |
| Gastrointestinal | Mesenteric vasculitis with microaneurysms in some patients |
| Kidneys | Glomerulonephritis (small-vessel vasculitis of the kidney); medium-vessel vasculitis occasionally evident on renal biopsy or demonstrated by cross-sectional imaging studies (renal infarcts) |
| Skin | Palpable purpura, ulcers, vesiculobullous lesions, splinter hemorrhages |
| Joints | Migratory pauciarthritis or polyarthritis or arthralgias; arthritis is nondestructive |
| Peripheral nerve | Sensory or motor mononeuritis multiplex |
| Central nervous system | True central nervous system vasculitis rare but reported |
Some vasculitis experts regard the presence of any upper respiratory tract involvement as evidence that the diagnosis is GPA (Wegener), not MPA. Thus, HEENT involvement in MPA is limited generally to rhinitis or mild cases of nondestructive sinusitis. Serous otitis media may occur in MPA but unlike in GPA (Wegener), granulomatous inflammation is absent. Ocular lesions in MPA (eg, episcleritis, conjunctivitis, keratitis, and occasionally scleritis) have been reported but are less common and less severe than in GPA (Wegener).
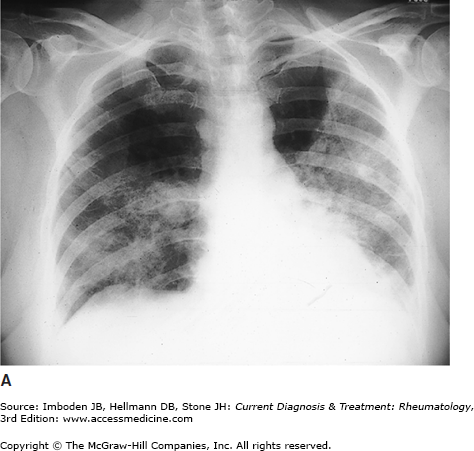
The principal pulmonary manifestation of MPA is capillaritis, which leads to alveolar hemorrhage and often to hemoptysis. Hemoptysis may be only a late indication of bleeding. The typical radiologic features of alveolar hemorrhage are shown in Figure 33–1. Alveolar hemorrhage is associated with a worse prognosis. Interstitial fibrosis and pleuritis occur in some patients with MPA. Pulmonary fibrosis that resembles usual interstitial pneumonitis in clinical presentation is increasingly recognized as a disease manifestation of MPA. Many cases of pulmonary fibrosis are associated with previous alveolar hemorrhage, but the precise relationship between alveolar hemorrhage and fibrosis is not clear.
Renal involvement is seen in at least 80% of patients with MPA. The classic presentation of renal disease in MPA is a rapidly progressive glomerulonephritis reminiscent of GPA (Wegener) (Figure 33–2A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree