38
Preventing and Treating Stiffness
Diagnosis
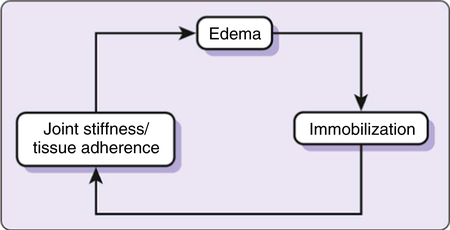
Nonuse resulting from pain, denervation, and immobilization triggers a cascade of problems that further perpetuate stiffness. These include muscle atrophy (and further weakness), edema, muscle collagen fiber cross-linkage, and altered motor programs (Fig. 38-1). All of these must be considered when working to undo the effects of upper extremity nonuse.
Other soft tissues that may indirectly restrict joint mobility include adhered or taut muscular fascia and taut peripheral nerves. In both cases, these adhered or taut structures can create painful and restricted joint mobility. See Chapters 12 and 24 for additional information on the cause and treatment of these conditions.
Lastly, a joint may be restricted by changes in the joint’s bony architecture. Arthritis; ankylosis (that is, fusion); and bony malalignment resulting from fracture, subluxation, or dislocation may result in structural “blockades” to joint motion. Chapters 25, 27, and 33 explore these conditions and the treatment of resultant physical and occupational performance limitations.
Timelines and Healing
After hemostasis has been achieved, our body responds during the first 2 to 12 days after a soft tissue injury through local vasodilatation and infiltration of white blood cells that clean up dead cells and, in the case of a wound, help to fight off infection. This phase is referred to as the inflammatory stage. Late in this phase, early bonding of the injured tissue begins via the migration of disorganized collagen fibers. A primary repair (that is, via suture) of injured soft tissue will typically require some amount of immobilization until the end of this phase to help facilitate healing. It is at this time that edema is prevalent and should be treated (see Chapter 3 for interventions). Edema control is often the emphasis at this time. The therapist works to facilitate prompt healing so that mobilization can be initiated. When inflammation is well controlled, the fibroblasts are signaled to begin their job of strengthening the repair of the damaged tissue. This is the fibroblastic stage and lasts from 3 days to about 3 weeks post injury in ideal conditions. Evolved fibroblasts soon begin laying down disorganized collagen fibers that cross-link with one another to stabilize the injury. This cross-linkage does not permit these fibers to efficiently move relative to one another and thus are an early source of stiffness.1 Edema continues throughout much of this phase as the wound environment continues to be hyperemic. Additionally, disuse leads to weakness of muscles that are antagonistic to this early stiffness. Stiffness early in this phase typically has a soft end feel but can feel firm as healing progresses. During this phase the therapist continues to focus on controlling edema and begins looking for critical opportunities to introduce appropriate controlled-stress to these healing structures to maintain soft tissue elasticity by promoting more functional organization of the collagen fibers.2 In the maturation phase, the process of laying down collagen normalizes and strong cross-linkages between collagen fibers form. Stiffness early in this phase feels firm in nature; however if pervasive for long periods, may feel hard. By this time, the therapist’s options become fewer.
Evaluation Tips
• Perceived and observed performance in occupations
• Importance and satisfaction of problematic areas of occupation
Your interview will also yield information about:
• Your client’s chief complaints
• The motivation level of your client
• Whether pain is experienced during movement; if so, where, how bad, and what
Clinical Examination
Generally speaking, the therapist should perform a clinical examination when:
Scarring
The therapist will also inspect for incisional scars, scarring that spans joints, or scarring that is proximal/distal to the stiff joint (see Chapter 34). Along with this, the observation of scar blanching (turning a white hue) or migration of surface scarring during joint movement may indicate that scar tissue is restricting mobility.
Goniometry
ROM assessment determines the nature and extent of stiffness in a given joint and is the most commonly used measure of change in joint mobility. To determine whether weakness or soft tissue/bony restrictions are sources of limited joint mobility, the therapist will take both active and passive measurements. Generally speaking, a goniometric measurement of the hand is subject to a 5° measurement error,5 and because of this, goniometric measurements need to have a discrepancy of greater than 5° for there to be a “real difference.”6 This is true for all of the following circumstances:
• When comparing active measurements to normative data
• When comparing active measurements to passive measurements of the same joint
• When comparing baseline goniometric measures to those taken when re-evaluating
The first step is to compare active measurements to normative measures. If a “real difference” exists that is impeding function, then compare the findings to a passive measurement of the same joint. If the passive measurement is 5° more than the active measurement, weakness or adherence is likely contributing to joint motion limitations. If active movement and passive movement are within 5° of one another yet are different from the norms, then a passive restriction is present. To further complicate things, it is possible to have both weakness and passive restrictions affecting the same joint. In these cases you would expect to have passive measures more than 5° below the norm and active measures more than 5° below passive measurements. When a passive limitation has been confirmed, a firm or hard end feel is experienced. The firm end feel indicates a soft tissue restriction, whereas the hard end feel indicates a boney block to movement.7 True boney blocks to movement are not responsive to stretching and for clients with such limitations, the focus should shift to an adaptation approach.8 If soft tissue is impeding joint motion, a series of differential tests will help to further explain the origin of the impediment.
Proximal Interphalangeal Joint Stiffness
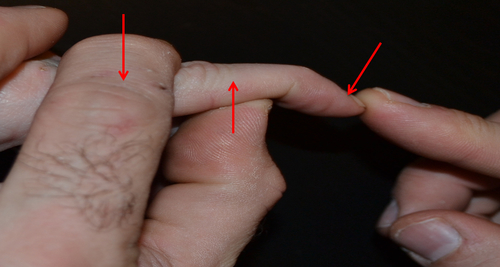
These tests are most commonly used when proximal interphalengeal (PIP) joint passive flexion is limited and the therapist wants to determine if extrinsic finger extensor, intrinsic (lumbrical), or joint capsule tightness are responsible. If posturing in metacarpophalangeal (MP) flexion lessens available passive PIP flexion, there is extrinsic extensor tightness (Fig. 38-2) whereas when a posture of MP extension lessens passive PIP flexion, there is intrinsic (lumbrical) tightness.8 Fig. 38-3 illustrates the testing procedure for this. If the posture of the MP joint does not at all influence passive PIP joint flexion yet passive PIP motion is still limited, a contracted joint capsule is likely the problem. A similar process can be followed when attempting to determine the source of PIP extension contractures. In this case, the therapist measures the available passive PIP extension with MP extension and compares to MP flexion. If the values remain unchanged, capsular tightness is likely responsible;9 if there is greater than 5° difference in PIP passive extension, extrinsic finger extensor tightness is likely responsible. Extrinsic tightness is commonly experienced by those with spasticity, forearm fractures, or those who have had immobilized wrists or elbows. Intrinsic tightness is commonly experienced by those who have sustained hand crush injuries, metacarpal fractures, and those with rheumatoid arthritis. In addition to the reduced grasp associated with intrinsic tightness, there is evidence to support that this tightness may, at times, be partially responsible for the development of carpal tunnel syndrome.10
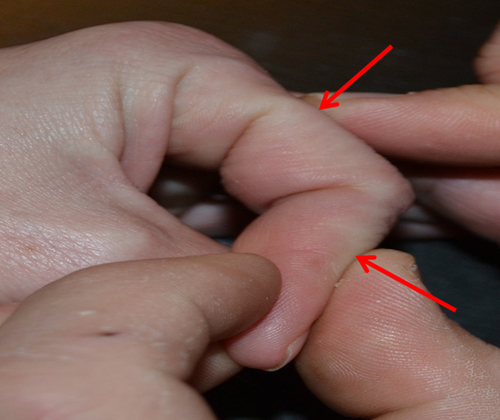
Position: Place MP joint in maximal flexion. Test: Passively flex the PIP joint. Rule out PIP joint contracture by repeating with the MP joint extended. Interpret: Extrinsic extensor muscle tightness is present if PIP joint motion is greater when MP is extended than when is flexed. PIP joint contracture is present if position of MP does not influence PIP flexion.
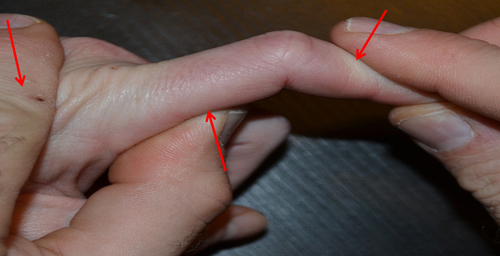
Position: Place MP joint in full extension. Test: Passively flex the PIP joint. Rule out PIP joint contracture by repeating with the MP joint flexed. Interpret: Intrinsic muscle tightness is present if PIP joint motion is greater when MP is flexed than when is extended. PIP joint contracture is present if position of MP does not influence PIP flexion.
Distal Interphalangeal Joint Stiffness
Extrinsic finger flexor tightness (tested by comparing passive distal interphalangeal [DIP] extension with wrist in flexion to passive DIP flexion with wrist in neutral) or capsular (joint) tightness can restrict DIP passive extension. Conversely, DIP passive flexion is typically hindered by either a contracted joint capsule or oblique retinacular ligament (ORL) tightness (Fig. 38-4) An ORL tightness test (Fig. 38-5) determines the source of limited passive flexion. If by placing the PIP in extension your client’s passive DIP flexion measurements become more impaired, then ORL tightness is present. If changing the posture of the PIP joint does not alter your DIP flexion measurements, then the joint capsule is likely contracted. A tight ORL often accompanies a boutonnière deformity and, along with the management of a PIP flexion contracture, requires therapeutic attention.
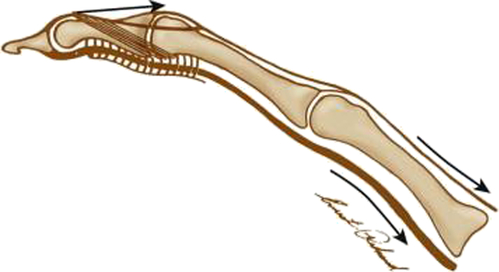
The ORL originates from the volar surface of the A2/C1 pulleys of the proximal phalanx and travels “obliquely” toward the dorsum of the distal phalanx where it inserts into extensor mechanism. (Adapted from Skirven TM, Osterman AL, Fedorczyk JM, et al, editors: Rehabilitation of the hand and upper extremity, ed 6, Philadelphia, 2011, Mosby).
Position: Place PIP joint in full extension. Test: Passively flex the DIP joint. Rule out PIP joint contracture by repeating with the PIP joint flexed. Interpret: ORL tightness is present if DIP joint motion is greater when PIP is flexed than when extended. DIP joint contracture is present if position of PIP does not influence DIP flexion.
Wrist Stiffness
• Passive wrist extension that is not impaired with fingers in flexion but is impaired when adding finger extension indicates extrinsic finger flexor tightness
• Passive wrist flexion that is not impaired with fingers in extension but is impaired when adding finger flexion indicates extrinsic finger extensor tightness
• Passive wrist movement that is impaired but not impacted by the posture of the digits is likely capsular in origin or due to tightness of the prime movers (for example, extensor carpi radialis brevis, or flexor carpi radialis). If the posture of the elbow (flexed versus extended) influences wrist movement, the prime wrist movers may be tight; if not, capsular tightness is likely responsible
• Passive wrist flexion less than the unaffected side regardless of finger or elbow posturing and further impaired by finger or elbow posturing in extension or flexion indicates both capsular tightness and muscular tightness
Extrinsic Tendon Adherence and Muscular Tightness
Tendon-incisional scar adherence may be a source of passive joint limitations. In such cases, adherence of extrinsic tendons presents slightly differently than does muscular shortening. Extrinsic tightness will likely influence the mobility of all joints crossed by the muscle-tendon unit; however scar adherence impacts only joint mobility distal to the site of adhesion. This is because there is muscular elasticity proximal to the site of adherence yet, because a tendon has little elasticity, there is minimal motion from the point of tendon adherence distally. Likewise, tendon-tendon adherence may occur; particularly in the case of the extrinsic flexors. In this situation, the passive excursion of these tendons would be unaffected yet active composite fisting would be challenging because the adhered FDP and flexor digitorum superficialis (FDS) tendons are less capable of differentially gliding relative to one another.11 Differential gliding may be compromised after flexor tendon repairs, with carpal tunnel syndrome, or following carpal tunnel release surgery. Active tendon gliding exercises (Fig. 38-6) are often prescribed, when not contraindicated, to prevent or remediate problems with differential gliding in such cases. Differential tests for joint motion are very detailed and typically involve modifying the posture of joints that are proximal or distal to the joint of interest. Therapists need to be intentional and consistent in positioning the joints proximal and distal to those that are measured. If therapists are not consistent in their goniometric assessment, interrater reliability suffers and so does our ability to document the effectiveness of our interventions.

Edema Evaluation
With any client who has stiffness resulting from trauma, an inflammatory condition, dependency, weakness, or nonuse, an evaluation for the presence of edema is critical. See Chapter 3 for a more details on the process of edema assessment and intervention. Early attention to edema when present or when expected is crucial.
Hand Therapy (Non-Operative) Interventions
Soft Tissue Mechanics
While each form of soft tissue has its own unique properties, the mechanics of soft tissue are generally applicable to all types. The therapist’s ability to stretch or prevent tightness relies heavily on the relationship between stress and strain (Fig. 38-7). Stress is the amount of force per unit area (that is, pressure) applied to soft tissue. Strain is a result of stress and is expressed mathematically as the change in length of soft tissue/original length × 100. Most biological materials have elastic and plastic properties. Materials that are elastic return to their original form when stress is removed, whereas material that is plastic undergoes a change in composition that remains stable when stress is eliminated. To safely elongate or maintain the length of a soft tissue, strain must occur only in the elastic range. Stress that results in elongation of soft tissue into its plastic range will lead to microtearing, inflammation, and fibrosis. It has been suggested that 200 g (1/2 lb) of force12 is sufficient to adequately stress the PIP joint. However, these types of torque measurements are seldom performed clinically and thus therapists typically rely on subjective report from the client and changes in objective measures (for example, goniometry) to determine if the “just right” force administered by, for example, an orthotic intervention has been achieved. Ideally, your client should report the sensation of stretching but not pain while wearing a mobilizing orthosis.8 This brings us to the next important concept, strain rate, or the amount of tissue elongation per unit of time. Although the amount of stress is critical, so is the duration that this stress is longer than the total end range time (TERT) or amount of time a contracted joint is placed at its maximal length, the better the results.13 This combined low stress, long TERT or low load, long duration (LLLD) approach is believed to be best practice when attempting to resolve soft tissue contracture, because it promotes reorganization of collagen fibers within their elastic range without undue strain.13 (Table 38-1) highlights intervention options that are specific to a given impairment as well as a given phase of healing.
TABLE 38-1
Intervention Highlights across Phases of Healing and Physiological Barriers
| Healing Phase | Physiologic Barriers | Therapist Interventions | Orthotic Option(s) | |
| Inflammatory (2 to 5 days post-injury in optimal circumstances) | Edema | Get Clinical Tree app for offline access 
| ||



