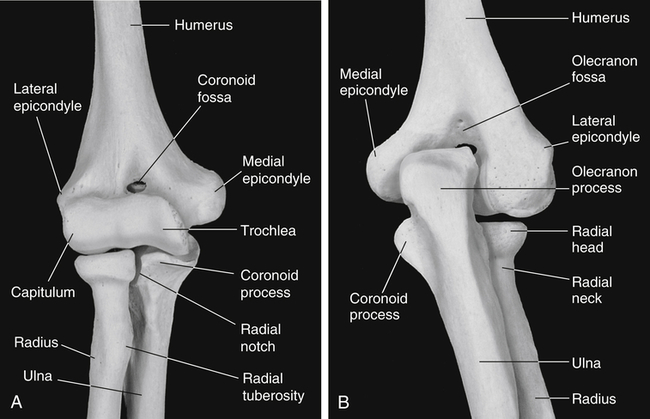
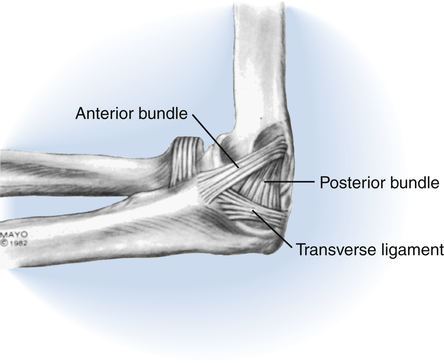
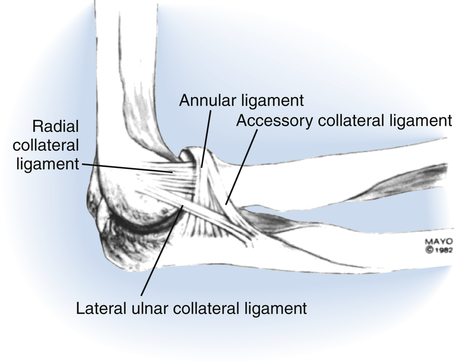
The elbow serves as the essential functional link between the hand and the shoulder, allowing the hand to be brought inward toward the body and outward into the surrounding environment. It also transfers force through the upper extremity (UE) during weight bearing on the hand. The functional range of motion (ROM) required at the elbow is reported to be 30° of extension, 130° of flexion, and 50° each of pronation and supination.1 However, because functional demands vary, the range required will differ somewhat among individuals. In general, it is easier to compensate for limited extension by moving closer to objects during reach than it is to compensate for limited flexion. Because the most common complication of elbow trauma is stiffness, it is essential that therapists treating individuals with elbow injuries be well versed in effective treatment approaches. To “push harder” or “be more aggressive” is not an effective solution and may instead cause more damage and stiffness. In addition to being mobile, the elbow must also be stable so that it can withstand the forces of daily activities. Maintaining the most effective balance between minimizing stiffness through early motion, preserving stability, and protecting healing structures is a challenge even for experienced therapists. Three bones contribute to the elbow joint, the distal humerus, proximal ulna, and proximal radius (Fig. 23-1). They form the three articulations of the elbow: the ulnohumeral, radiohumeral, and proximal radioulnar joints. The distal humerus has two articular surfaces: the spool-shaped trochlea medially and the convex capitellum (also known as the capitulum) laterally. The ulnohumeral joint is the close articulation of the trochlea with the rounded trochlear notch formed by the coronoid and olecranon of the proximal ulna. In full elbow flexion the coronoid fossa on the anterior distal humerus receives the coronoid process of the anterior trochlear notch. In full extension, the olecranon fossa on the posterior distal humerus receives the olecranon process of the posterior trochlear notch. The radiohumeral joint is the articulation of the capitellum of the distal humerus with the shallow concavity on the proximal aspect of the radial head. The radial head and the radial notch of the ulna form the proximal radioulnar joint. Due to the oblique orientation of the trochlea of the humerus, in full extension the elbow has a valgus angle, known as the carrying angle. It has been widely reported that men have a carrying angle of approximately 5° to 10°, while women have a slightly greater carrying angle of approximately 10° to 15°. However, measured radiographically, the normal carrying angle in adults is reported to be 17.8° on average with no significant difference between men and women.2 The three elbow articulations share a common joint capsule. The medial and lateral collateral ligament complexes of the elbow are essentially thickenings of the joint capsule. Portions of the collateral ligament complexes remain taut throughout elbow flexion and extension, making an essential contribution to static elbow stability. The medial collateral ligament complex (Fig. 23-2) has three components, the anterior bundle, posterior bundle, and the transverse ligament. This ligament complex, particularly the anterior bundle, stabilizes the elbow against valgus (abduction) forces. The lateral collateral ligament complex (Fig. 23-3) has four components, the lateral ulnar collateral ligament (LUCL), the radial collateral ligament, the annular ligament, and the accessory lateral collateral ligament. The lateral collateral ligament complex is considered to be one of the primary stabilizers of the elbow. It provides restraint from varus (adduction) forces. The LUCL, one of the four components of this ligament complex, also provides posterolateral stability to the ulnohumeral joint. Fractures of the distal humerus are relatively uncommon, accounting for only 2% of all fractures. They occur most frequently in young males and in females over 80 years of age. In younger individuals, distal humeral fractures are usually associated with higher velocity injuries, such as motor vehicle and sports-related accidents. In the elderly with poor bone stock, they can occur from a simple fall onto an outstretched hand.3 Displaced radial head fractures with comminution or mechanical block to forearm rotation require operative treatment. The presence of one or more associated injuries at the elbow including capitellum fracture, olecranon fracture, ligamentous injuries, and elbow dislocation, is also an indication for operative treatment. Approximately one in three radial head fractures is associated with another injury.4 Options for the operative treatment of radial head fractures include internal fixation with plate and screws, radial head excision, and radial head replacement. Comminuted fractures are treated with radial head excision or replacement. Displaced fractures with mechanical block to forearm rotation are treated with internal fixation or radial head excision. Note that due to important stabilizing function of the radial head, it must be replaced rather than excised in radial head fractures with associated injuries that compromise elbow stability. Most olecranon fractures require open reduction and internal fixation. A posterior approach is typically used. The type of internal fixation is chosen depending on the individual characteristics of the fracture. Options include Kirschner wires, tension band wiring, compression screws, and plate fixation. With appropriate management, outcomes of olecranon fractures are typically good to excellent.5 In addition to the complications common to all elbow fractures, hardware on the posterior aspect of the elbow is not always well tolerated. Chronic irritation can result in olecranon bursitis and may require excision of the hardware.6 Distal humeral fractures that are comminuted, displaced, involve the trochlea or capitellum, or have neurovascular involvement require operative treatment. There is a higher risk of complications in high-energy mechanisms of injury, open fractures, and non-operatively managed fractures. In addition to the complications common to all elbow fractures, heterotopic ossification, bone in nonosseous tissues, may develop following fractures of the distal humerus. Although these fractures are frequently challenging to manage, the majority heal within 12 weeks without significant complications.3 Most are stabilized surgically with open reduction and internal fixation with plates and screws. A posterior surgical approach is most commonly used for visualization of the fracture. The triceps is split or elevated and reflected, or an olecranon osteotomy is performed. Following an olecranon osteotomy, the olecranon is reattached with Kirschner wires and screws or plating.7 An anterior ulnar nerve transposition is sometimes performed during surgery for fracture repair to lessen the likelihood of postoperative ulnar neuropathy. Elderly individuals with complex distal humerus fractures and osteoporotic bone present a particular challenge to the surgeon. Total elbow arthoplasty may be necessary in these individuals if screws cannot obtain adequate bony purchase for fracture fixation.8 Radial head fractures that are non-displaced or minimally displaced are treated non-operatively, unless there is a mechanical block to forearm rotation. These fractures have a favorable prognosis as long as motion is begun early. Active motion is usually initiated within the first several days following injury. Be sure to emphasize elbow extension, because this motion is most frequently lost after radial head fracture. Immediate mobilization has been shown to result in less pain and better elbow function at 1-week follow-up as compared to motion initiated 5 days following radial head fracture; although results were similar with respect to pain, ROM, and function at 4-week follow-up.9 Non-displaced and minimally displaced radial head fractures treated non-operatively do not require as long of a period of protective immobilization as other elbow fractures and radial head fractures treated operatively. The use of a sling or orthosis for comfort during the first week is usually sufficient. Not all individuals with non-operatively managed radial head fractures require repeated therapy visits to achieve good results. However, to minimize the risk of elbow flexion contracture, it is important to provide a structured therapy program to individuals who are reluctant to move or who are stiff after several weeks of performing a home exercise program. Most distal humeral fractures require operative treatment. However, some non-comminuted, stable fractures with minimal or no displacement can be treated with closed reduction followed by immobilization in a cast or orthosis. To minimize the risk of stiffness, gentle motion must be started after no more than 2 weeks of full-time mobilization. If the distal humerus is not stable enough to tolerate motion after this period of initial immobilization, it is best treated surgically to achieve the necessarily stability to allow early motion.6 When treating a patient referred to you following surgery for a distal humerus fracture, initiate elbow motion exercises with passive or gravity-assisted extension and active flexion. Depending on the type of surgical exposure that was used, either the triceps mechanism or the olecranon osteotomy may require protection for the first 6 weeks or so. Therefore, check with the surgeon before beginning active elbow extension and passive elbow flexion.
Elbow Diagnoses
Function of the Elbow
Elbow Anatomy
Ligaments
Elbow Fractures
Distal Humeral Fractures
Operative Treatment
Diagnosis-Specific Information That Affects Clinical Reasoning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Elbow Diagnoses

