CHAPTER 7 Preoperative Planning and Imaging
Although the majority of cases of unconstrained shoulder arthroplasty are routine, certain patients have unique characteristics that merit special consideration. Preoperative planning identifies patients who may require deviation from routine unconstrained shoulder arthroplasty. Preoperative planning should be done well in advance of the surgical procedure and not be an afterthought the morning of surgery. The surgeon should review the patient’s clinical history and physical examination, radiographs, and any secondary imaging studies. This chapter presents our approach to preoperative planning for unconstrained shoulder arthroplasty.
CLINICAL HISTORY AND EXAMINATION
Any symptoms of infection, especially in patients who have previously undergone surgery or injections, should be investigated further. If patients have a history of infection after shoulder surgery or have had symptoms suggestive of infection (systemic fever; shoulder warmth, redness), a preoperative infection workup, including hematologic evaluation with a complete blood cell count and differential, a sedimentation rate, and C-reactive protein, is indicated. Additionally, a fluoroscopically guided shoulder aspirate is obtained and the specimen submitted for aerobic, anaerobic, fungal, and mycobacterial culture. If the findings are suggestive or diagnostic of infection, shoulder arthroplasty is postponed or canceled until infectious disease consultation is obtained and the infection is appropriately treated (Table 7-1).
Table 7-1 WORKUP FOR INFECTION BEFORE UNCONSTRAINED SHOULDER ARTHROPLASTY
| Test | If Abnormal |
|---|---|
| White blood cell count with differential | Increase suspicion for infection; consider arthroscopic biopsy |
| Sedimentation rate | Increase suspicion for infection if combined with an abnormal white blood cell count or C-reactive protein; consider arthroscopic biopsy |
| C-reactive protein | Increase suspicion for infection; consider arthroscopic biopsy |
| Fluoroscopically guided aspiration | Consider the shoulder as actively infected and treat as such; arthroscopic biopsy is unnecessary |
| Arthroscopic biopsy | Consider the shoulder as actively infected and treat as such |
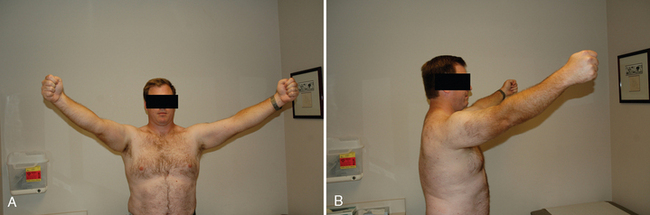
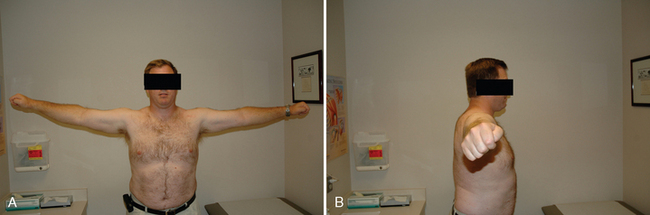
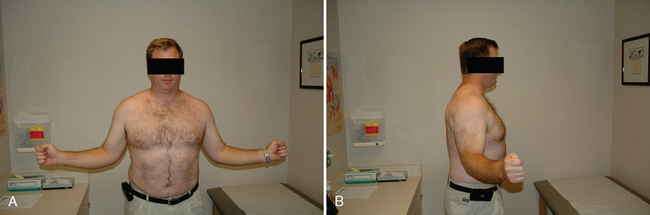
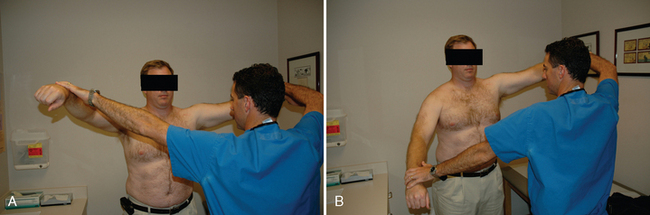
All our patients undergo a thorough shoulder examination. Motion and rotator cuff strength are of critical importance. Both active and passive mobility is recorded. Mobility parameters recorded are elevation in the plane of the scapula (Fig. 7-1), abduction (Fig. 7-2), external rotation with the arm at the side (Fig. 7-3), external rotation with the arm abducted 90 degrees (when possible) (Fig. 7-4), and internal rotation as determined by the vertebral level reached with an outstretched thumb (Fig. 7-5). Any incongruity of the glenohumeral joint as indicated by the presence of glenohumeral crepitus with motion is noted, as is any discrepancy in active and passive mobility.
Rotator cuff examination consists of testing each tendon of the rotator cuff by isolating it as much as possible. Jobe’s test is used to test supraspinatus integrity (Fig. 7-6).1 The external rotation lag sign and evaluation of external rotation strength with the arm at the side are used to test the infraspinatus (Figs. 7-7 and 7-8).2 The teres minor is tested via the horn blower’s sign (Fig. 7-9).3 The subscapularis is tested with the belly press test and, when mobility allows, the lift-off test (Figs. 7-10 and 7-11).4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree