Preaxial Polydactyly
CASE PRESENTATION
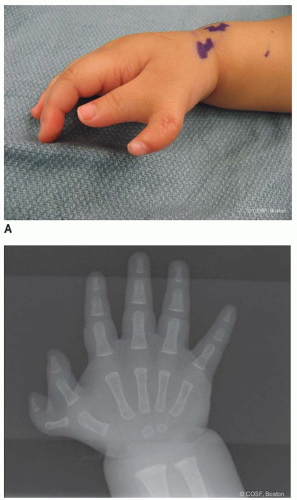
A 6-month-old male presents for evaluation of an “extra thumb” (Figure 4-1A). The family that reports this was present at birth. The child is otherwise healthy, and there is no family history of congenital hand differences. On examination, there are two well-formed thumbs, each with nail plates and flexion and extension creases over the interphalangeal (IP) joint. The metacarpophalangeal (MCP) joint appears broad but is stable. There appears to be active flexion and extension of the MCP joint of the more radial thumb, as well as abduction. No other abnormalities are seen. Plain radiograph is shown in Figure 4-1B.
CLINICAL QUESTIONS
What causes thumb duplication? How common is it?
Are there any associated syndromes or anomalies?
How is it classified?
What are the treatment principles?
What types of surgical procedures are done?
What are the expected results and potential complications of surgery?
THE FUNDAMENTALS
Preaxial polydactyly—often referred to as thumb duplication, thumb polydactyly, radial polydactyly, or split thumb—is among the most common congenital conditions presenting to the pediatric hand and upper extremity surgeon. Understanding of the pathoanatomy and principles of surgical reconstruction is critical to provide these patients with stable, mobile, functional, and aesthetically acceptable thumbs.
Etiology and Epidemiology
Preaxial polydactyly occurs in approximately 1:10,000 live births.1,2 It is more common in Asians and Native Americans and affects Blacks and Caucasians with equal frequency. Males are more commonly affected than females.
While most cases are sporadic, and unilateral, in some patients there may be an autosomal dominant inheritance pattern. Several syndromes have been identified that have been associated with thumb duplication.3 Wassel VII thumb duplications (see below) are the exception, as these anomalies have a higher hereditary predisposition and are associated with other hematologic, cardiovascular, or musculoskeletal conditions.3
The etiology of thumb duplication has been evaluated through a series of human and animal investigations.4, 5 and 6 Most have concluded that delayed involution of the apical ectodermal ridge on the preaxial border of the hand results in induction of thumb duplication. The single mesenchymal condensation along the preaxial border of the hand that is destined to form the thumb is therefore cleaved or split.
These embryologic observations confirm what is clinically seen. Rather than two separate well-formed digits, each of the thumbs is deficient, containing elements that combined account for the expected anatomy. For this reason, the term “thumb duplication” is a misnomer, and “split” or “bifurcated” thumb is more accurate.7
Clinical Evaluation
If you don’t look, you can’t see.
—Bob Knight
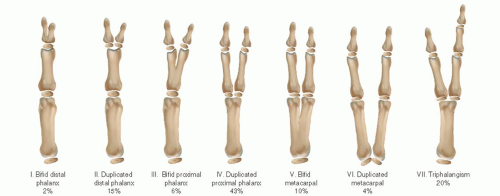
While a host of classification systems have been proposed, the Wassel classification has proven to be the most simple in application and helpful in surgical planning8 (Figure 4-2) (see Sidebar 1). This system classifies the deformity depending upon the level of duplication from distal to proximal, with odd numbers assigned to the bones and even numbers assigned to the joints. A bifid distal phalanx is type I, a duplicated distal phalanx is a type II, a bifid proximal phalanx is type III, and so on. (The easy way of remembering this is that the classification type refers to the number of abnormal bones.) Type VII, by definition, refers to any thumb duplication with a triphalangeal thumb.
Using the Wassel classification, type IV thumbs are the most common, representing approximately 40% to 45% of cases; Wassel type II is the second most common pattern (15%), followed by type VII.8
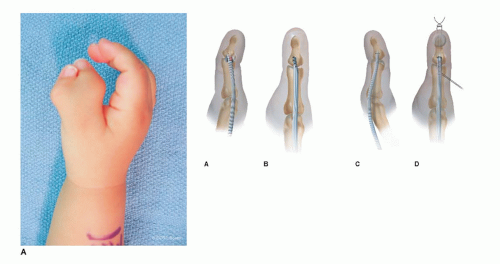
While the Wassel classification effectively describes the bony anatomy and guides surgical treatment, not all thumb duplications are the same. Practically, there is a great difference between divergent or parallel thumb duplications and the zigzag (or divergent-convergent) duplications (Figure 4-3). In the latter situation, angular deformity is caused by both abnormal bony alignment and eccentric tendon insertions. Recurrent deformity is more commonly seen in these situations, and greater care is needed to restore longitudinal bony alignment and dynamic muscle pull during surgical reconstruction.9
SIDEBAR 1
The History behind the Wassel Classification
I learn teaching from teachers. I learn golf from golfers. I learn winning from coaches. —Harvey Penick
Classification systems are most helpful for surgeons if they are simple to use, portend prognosis, and guide treatment. Based upon these criteria, it is no surprise that the Wassel classification is the most widely used and commonly accepted system for the characterization of preaxial polydactyly. Although many additional classification systems have been proposed, none have duplicated the simplicity or elegance of Wassel’s scheme.
It is fair and proper to recognize that Wassel’s original description of the classification and results of surgery for thumb duplication, published in 1969, was written when Wassel was a clinical fellow working with Dr. Adrian Flatt at the University of Iowa. Indeed, the observations and results described therein were directly the result of Dr. Flatt’s clinical efforts, careful documentation, and academic perspective. Although Flatt was appropriately acknowledged in a footnote on the 1969 publication, the classification system continues to bear Wassel’s name.
In addition, in cases in which there is considerable IP joint stiffness and abduction of the thumb, the presence of a pollex abductus should be considered (Figure 4-4). This abnormal connection between the flexor pollicis longus (FPL) and extensor pollicis longus (EPL) tendons has been reported in up to 20% of thumb duplications.10,11
Surgical Indications
Almost universally in the Western world, the presence of a thumb polydactyly is an indication for surgical reconstruction. There are some cultures, however, where this is not the case. Given that surgery and anesthesia can safely be performed in many parts of the world over the age of 6 months, the timing of reconstruction can precede fine motor development. Rudimentary grasp precedes pinch. Tip-to-tip pinch does not begin to develop until later, up to 15 months of age, and patterns of fine motor function do not become established until 3 years of age. Surgery may be safely and appropriately performed at 9 to 12 months of age in most advanced care settings.
SURGICAL PROCEDURES
The goals of surgery are to create a single, stable, mobile, straight thumb. As the radial thumb is typically most hypoplastic, it is the thumb that is most commonly removed. Based upon this observation, Kanavel is attributed as stating that simple amputation of the more hypoplastic thumb “…requires no ingenuity and creates no problem.”12 However, in the vast majority of situations, simple ablation is not sufficient.13 Amputation of the radial thumb, while tempting, is often doomed to failure, as the abductor pollicis brevis (APB), radial collateral ligament (RCL), and bifid tendons are not reconstructed and the longitudinal skeletal alignment is not corrected.
Preservation of vascularity is usually not an issue, as both thumbs are supplied by at least one digital artery in the vast majority of cases.14 Kitayama and Tsukada have previously shown that in 74% of cases, there is a digital artery to each thumb. In 12% of cases, there were two arteries to the ulnar and one artery to the radial thumb. In
9% of cases, each thumb is supplied by two digital arteries. There is a single digital artery—typically to the more ulnar thumb—in only 5% of cases. For these reasons, caution is needed when ablating the rare, hypoplastic ulnar thumb.
9% of cases, each thumb is supplied by two digital arteries. There is a single digital artery—typically to the more ulnar thumb—in only 5% of cases. For these reasons, caution is needed when ablating the rare, hypoplastic ulnar thumb.
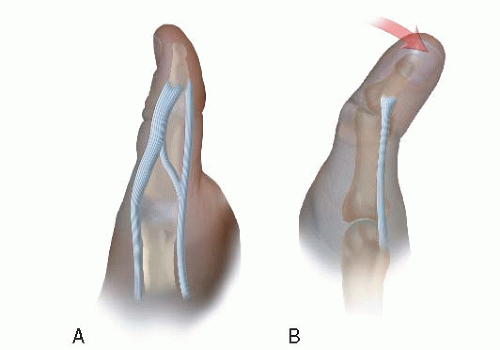 FIGURE 4-4 Schematic diagram of the pollex abductus as seen from the radial (A) and dorsal (B) aspect. Note the resultant thumb abduction and IPJ stiffness. |
Surgery should address all elements of the deformity at the initial procedure if at all possible. This includes skin, extrinsic tendon, and instrinsic muscle rebalancing along with longitudinal bone and joint realignment and stabilization. At times, this means wedge osteotomies of the reconstructed thumb with bone from the ablated thumb. This extensive surgery can be delicate so as to achieve anatomic restoration without vascular compromise. These principles are applied to simpler Wassel IIs and IVs, the more difficult divergent-convergent Wassel IVs and 50-50 IIs, the rarer Wassel VIs, and the assortment of Wassel VIIs. The bifid Is, IIIs, and Vs are a bit more straightforward due to stable, aligned joints.
• Simple Ablation
When you come to a fork in the road, take it.
—Yogi Berra
In rare situations, a simple soft tissue nubbin on the radial aspect of the hand can present as a thumb duplication (Figure 4-5). In these cases, there are no bony or clinically important soft tissue connections between the more developed “ulnar thumb” and the radial nubbin, which is often only connected by a skin stalk. Clearly in these situations, simple ablation of the nubbin can be performed without the need for bony work, ligamentous reconstruction, or muscle/tendon transfers.
A few technical steps should be considered during these simple ablations. First, despite the hypoplastic appearance of the nubbin, there is always a very real vascular pedicle within the soft tissue stalk, which should be identified and cauterized during ablation. In addition, to avoid a symptomatic neuroma, the accompanying digital nerve should be withdrawn, sharply transected, and allowed to retract into the soft tissues. Finally, an elliptical skin incision around the base of the soft tissue stalk should be made to allow for primary closure without “dog ears” or the aesthetically displeasing “nipple” of tissue that can form with careless or inexact skin incision or soft tissue resection. Also, always look for tendon or muscle insertion even in the most rudimentary thumbs. Surprisingly, there is often an intrinsic attachment that should be transferred.15