Posterolateral Rotatory Instability
Russell M. Nord
Marc R. Safran
BACKGROUND/ANATOMY/ETIOLOGY
Posterolateral rotatory instability (PLRI) of the elbow was first described by Osborne and Cottrell (18) and the pathoetiology elucidated and diagnosis was popularized by O’Driscoll et al. (14). PLRI is defined by subluxation of the proximal radius from the distal humerus resulting in a posteriorly subluxated radial head. This is different from a radial head dislocation because in PLRI, the proximal radioulnar joint remains intact. It is also differentiated from acute elbow dislocation because in an elbow dislocation, the lateral structures (and occasionally medial structures) are disrupted, while PLRI is reserved as a description of chronic lateral-sided rotatory instability.
The lateral side of the elbow is supported by four structures: the lateral ulnar collateral ligament (LUCL), radial collateral ligament (RCL), annular ligament, and accessory RCL (Fig. 3.1). The LUCL originates on the lateral epicondyle and inserts on the ulnar supinator tubercle and crest. The RCL originates on the lateral epicondyle and inserts on the annular ligament. The annular ligament both originates and inserts on the proximal ulna, enveloping the proximal radius (9). The accessory RCL runs from the inferior portion of the annular ligament to the supinator crest of the ulna (12). Other authors have failed to find discrete ligamentous structures on cadaveric specimens and have instead suggested that one confluent capsule or “conjoint ligament” with various thickenings provides stability to the lateral side of the elbow (3). The overlying muscles and underlying bony architecture also contribute to both dynamic and static stability Table 3.1.
O’Driscoll and colleagues initially implicated the LUCL as the essential anatomic lesion that led to PLRI (14). However, more recently, this has been challenged as the importance of the RCL (4,8) and overlying musculature of the common extensors (3,8) have also been shown to play an important role in lateral-sided elbow stability. Further, Seki and colleagues hypothesized and demonstrated that the lateral ligament complex functions as a Y-shaped structure. Disruption of the anterior band of the Y led to significant laxity to varus torque, while further sectioning of the posterior band resulted in gross instability (Seki). This suggests that isolated distal RCL or LUCL injury (the upper and lower arms of the “Y”) may not result in PLRI. However, a proximal injury off of the lateral epicondyle (the base of the “Y”) will disrupt the function of the other two arms and can result in PLRI.
The etiology of PLRI is typically posttraumatic. PLRI is most commonly a late sequela of elbow dislocation or subluxation, when the lateral-sided structures are stretched or torn and fail to heal with nonoperative treatment (13). It may also result from a posttraumatic condition where the coronoid is insufficient (16). PLRI may also result from gradual stretching of the lateral structures as a consequence of a malunited pediatric supracondylar humerus fracture that produces cubitus varus (15).
The etiology of PLRI may also be the result of iatrogenic injury. PLRI has been described after radial head resection where an unrecognized LUCL injury was likely (5). Additionally, it has been described after multiple steroid injections for lateral epicondylitis in a series of three middle-aged females (6). Lastly, PLRI has also been described as a consequence of overly aggressive surgery for lateral epicondylitis (11).
DIAGNOSTIC MODALITIES
The diagnosis of PLRI can be elusive. Patients will often present with vague symptoms, though they may note catching, snapping, recurrent instability or apprehension (2,13). Occasionally, the patient may note locking or catching when turning the car steering wheel, with their forearm going into supination.
Once the patient’s complaints have raised suspicion for PLRI, confirming the diagnosis is paramount. While the gold standard diagnostic examination is the pivot shift maneuver (Fig 3.2), its usefulness in the office,
without anesthesia, is limited, as patients will often guard against subluxation and the examiner may only appreciate apprehension or patient discomfort. The pivot shift test is most reliable when done under anesthesia and the subluxation can actually be appreciated. The pivot shift test is most easily performed with the patient supine, starting with the affected limb overhead and the forearm in full supination and shoulder in full forward elevation. The elbow begins in extension and an axial load with valgus is applied, resulting in posterior subluxation of the radial head, which is often recognized by a prominence of the radial head and a dimple just proximal to it (Fig. 3.2). The elbow is slowly flexed as the axial load and valgus force are applied. As the elbow is flexed, there is a clunk of radial head reduction. This usually occurs at approximately 40 degrees, as the triceps becomes taut and causes the reduction, which is felt by the examiner as a clunk. With greater degrees of laxity of the posterolateral structures of the elbow, greater degrees of elbow flexion are necessary to produce the reduction.
without anesthesia, is limited, as patients will often guard against subluxation and the examiner may only appreciate apprehension or patient discomfort. The pivot shift test is most reliable when done under anesthesia and the subluxation can actually be appreciated. The pivot shift test is most easily performed with the patient supine, starting with the affected limb overhead and the forearm in full supination and shoulder in full forward elevation. The elbow begins in extension and an axial load with valgus is applied, resulting in posterior subluxation of the radial head, which is often recognized by a prominence of the radial head and a dimple just proximal to it (Fig. 3.2). The elbow is slowly flexed as the axial load and valgus force are applied. As the elbow is flexed, there is a clunk of radial head reduction. This usually occurs at approximately 40 degrees, as the triceps becomes taut and causes the reduction, which is felt by the examiner as a clunk. With greater degrees of laxity of the posterolateral structures of the elbow, greater degrees of elbow flexion are necessary to produce the reduction.
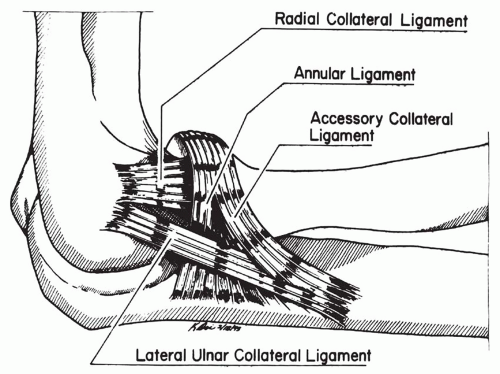 FIGURE 3.1 Ligamentous anatomy of the lateral aspect of the elbow. Note the lateral ulnar collateral ligament, RCL, accessory RCL, and annular ligament. |
A recent study supports the difficulty of the pivot shift test in the conscious patient. Of eight patients with PLRI, only three had a positive pivot shift test while awake. However, all eight had a positive exam under anesthesia (20).
Other tests performed in the awake patient may suggest a preliminary diagnosis of PLRI, including palpation for posterior radial head subluxation, the chair test, the push-up test, and the table top test. We have found that simply supinating the forearm gently with the elbow at 90 degrees of flexion may lead to a palpable posterior subluxation of the radial head. Regan has shown the efficacy of the chair and push-up tests in aiding the diagnosis of PLRI. These tests are alike in that they position and load the elbow in a fashion similar to the pivot shift test. For the chair test (chair sign), the patient is seated in a chair with arms and the patient puts his or her hands on those arms with the elbows at 90 degrees, forearms supinated and arms abducted slightly beyond shoulder width (Fig. 3.3). The patient then rises from the chair using only the upper extremities for power. Apprehension, reluctance to extend the elbows fully, or subluxation is considered positive. When the forearms are pronated and the test repeated, the patient’s symptoms should disappear. In Regan’s study, this test was positive in seven out of eight patients with PLRI (20).
TABLE 3.1 Results after Ligament Reconstruction of the Lateral Ulna Collateral Ligament | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
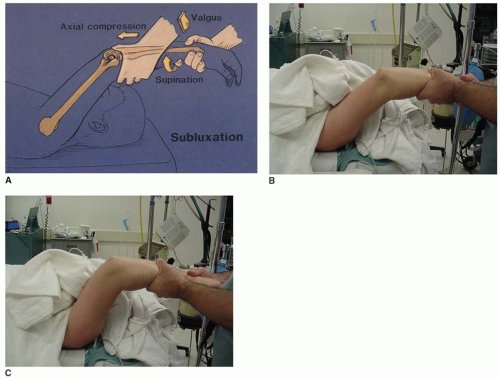 FIGURE 3.2 Pivot shift maneuver of the elbow to assess for posterolateral rotatory laxity and instability. A: The patient is supine with the arm in full forward elevation. The extended elbow is supinated and a valgus stress applied. The radial head is subluxated posteriorly in this position when there is laxity or injury to the posterolateral ligamentous structures (B). As an axial load is applied, the elbow is flexed, and there is usually a clunk associated with reduction of the radial head (C). This usually occurs at 40 degrees of elbow flexion but may occur in greater degrees of flexion with more ligamentous laxity or injury. In the awake patient, the patient may be apprehensive and may not allow completion of this maneuver. (Taken from O’Driscoll SW, Morrey BF. Surgical reconstruction of the lateral collateral ligament. In: Morrey BF, ed. The Elbow. Master Techniques in Orthopaedic Surgery. 2nd Ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002—Fig. 15.3B.) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








