Posterior Pelvic-Ring Disruptions: Iliosacral Screws
Milton L. Chip Routt Jr
Pelvic fractures and dislocations are uncommon injuries that usually result from a high-energy traumatic event such as a motor vehicle or motorcycle accident, a fall from a significant height, or a heavy object crush. In elderly patients with poor bone quality, even lower energy accidents can cause pelvic-ring instability. Mechanical instability of the pelvic ring commonly occurs when normal physiological forces produce deformation at the pelvic injury sites. Pelvic-ring instability is difficult to treat successfully for many reasons. The osseus anatomy is complex, the injury sites can be numerous, the related soft-tissue injury is confusing, and most orthopedic surgeons lack sufficient experience treating these injuries. Classification schemes have attempted to categorize pelvic-ring injuries; however, the variety and complexity of these injuries has frustrated any grouping method. Experienced clinicians realize that the most effective pelvic classification system is simply an anatomical description of the injury sites and their displacements/deformities. An anatomical description is exact, easy to remember, reproducible, reliable, and helps to guide accurate treatment. For the patient with an unstable pelvic-ring injury, pelvic-related bleeding as well as the other organ system injuries due to the traumatic event can cause hemodynamic instability. The physiologically unstable patient with a mechanically unstable pelvic-ring injury therefore demands an early and coordinated management strategy. A multidisciplinary and dynamic team approach facilitates an efficient resuscitation as well as definitive treatment that is tailored to the patient’s specific injuries and evolving clinical course. Over time, many different treatments have been used to stabilize pelvic-ring injuries without adversely affecting the overall patient condition. Modern treatment techniques have improved patient care due to numerous factors including clinical experience, biomechanical research, implant development, and imaging techniques. Despite these advancements, patients with unstable pelvic-ring injuries continue to challenge clinicians as we seek even better methods to resuscitate, reduce, stabilize, and rehabilitate these complex injuries and patients.
INDICATIONS AND CONTRAINDICATIONS
Iliosacral screw fixation is indicated for patients with unstable posterior pelvic-ring injuries including sacroiliac (SI) joint dislocations, sacral fractures, certain posterior iliac “crescent” fracture-SI disruptions, and combinations of these injuries. Iliosacral screw fixation is applied using osseus fixation pathways (OFP) within the upper-sacral segments. The sacral osteology, pelvic instability severity, and specific injury patterns determine how many and at what exact sites the screws are located. Iliosacral screws are used alone or in conjunction with other forms of pelvic internal or external fixation. They can be resuscitative devices providing lag screw-dependant compressive reductions and temporary as well as definitive fixation. The timing of internal fixation for displaced pelvic-ring injuries depends on numerous factors such as the patient’s overall clinical condition, fracture pattern, local skin condition, hemodynamic status, patient age and body habitus, and abdominal or urologic injuries.
The surgeon must meet certain criteria to insert iliosacral screws safely. The surgeon must completely understand normal posterior pelvic anatomy, as well as its variations, especially the upper-sacral osseus structure and the fluoroscopic imaging of these bony details. High-quality consistent fluoroscopic imaging of the entire
pelvis must be available during surgery. The surgeon must completely understand the specific injury and the displacement patterns of the posterior pelvic ring and be able to correlate normal and altered pelvic pathologic conditions as seen on radiographic images. Based on the preoperative plan, radiographs, and computed tomography (CT) of the pelvis, the surgeon must be confident that the patient’s upper-sacral anatomy will allow safe screw placement. Finally, the surgeon must possess the technical skill to reduce the posterior pelvic deformity accurately by closed or open techniques. Iliosacral screws should not be used unless the injured area is accurately reduced. Accurate reduction improves stability as well as the area available for the screws.
pelvis must be available during surgery. The surgeon must completely understand the specific injury and the displacement patterns of the posterior pelvic ring and be able to correlate normal and altered pelvic pathologic conditions as seen on radiographic images. Based on the preoperative plan, radiographs, and computed tomography (CT) of the pelvis, the surgeon must be confident that the patient’s upper-sacral anatomy will allow safe screw placement. Finally, the surgeon must possess the technical skill to reduce the posterior pelvic deformity accurately by closed or open techniques. Iliosacral screws should not be used unless the injured area is accurately reduced. Accurate reduction improves stability as well as the area available for the screws.
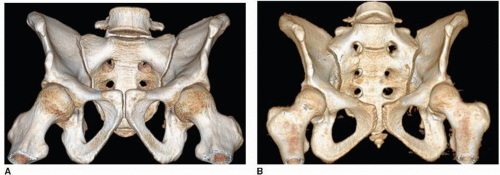
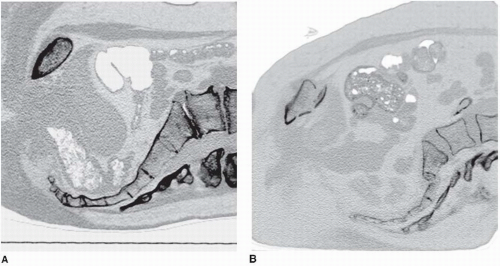
Dysmorphism of the upper sacrum is a relative contraindication for the insertion of iliosacral screws. Dysmorphism is a common lumbosacral spinal segmentation variant. The dysmorphic upper-sacral segment typically has a diminished and angular alar osseous area available for safe iliosacral screw passage into the sacral body. The dysmorphic upper-sacral segment has obliquely oriented alar OFP. The distinct osseus features of sacral dysmorphism are easily identifiable on the preoperative imaging studies. These upper-sacral segment dysmorphic “abnormalities” occur in approximately 40% of patients and are best identified on the pelvic outlet plain radiograph and CT scan. These abnormalities result from in utero segmentation variation and are most often symmetrical, but can also have asymmetrical and even unilateral patterns in some patients. The radiographic hallmarks of upper-sacral segment dysmorphism are best visualized on the pelvic outlet plain film and include the following: (a) the lumbosacral disc space is essentially colinear with the iliac crests, (b) the ventral foramen of the upper-sacral nerve root are not circular in appearance, (c) residual disc space is noted between the upper and second sacral segments, (d) the dysmorphic ala decline acutely from the cranial-posterior-medial upper-sacral body toward the SI joints in a caudal-anterior-lateral sloping in both the sagittal and coronal planes, and (e) mamillary processes (underdeveloped transverse processes) are seen along the dysmorphic ala. On the CT scan of the pelvis, sacral dysmorphism is noted by accentuated, undulating SI surfaces; an obliquely oriented, anterior, alar cortex relative to the iliac cortical density (ICD); and a narrowed alar zone available for screw insertion (Fig. 39.1A,B).
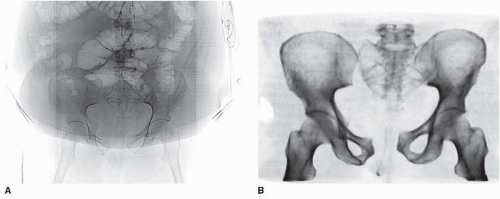
Obesity is a relative contraindication to iliosacral screw fixation for several reasons. Intraoperative fluoroscopic imaging in obese patients is compromised by the excessive abdominal panniculus, which may obstruct inlet and outlet images of the pelvis (Fig. 39.2A,B). Lateral pelvic flank obesity obstructs predictable true lateral sacral imaging. Fluoroscopic detail in obese patients may be inadequate for safe screw placement. In addition, extra-long instruments such as drills, taps, and screwdrivers are necessary for treating the obese patient.
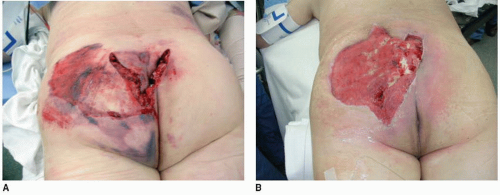
In the recent past, fluoroscopic imaging of the pelvis was also complicated in some polytraumatized patients because of contrast agents that were used during the initial abdominal evaluations. These agents and techniques are rarely used today and should be avoided when possible. In patients with open fractures or compromised posterior skin and soft tissues, iliosacral screw placement should be done percutaneously when possible, rather than through an open approach. In a common mistake, the surgeon enters and inadvertently decompresses a pelvic degloving injury during the process of iliosacral screw insertion. In such situations, the screw is inserted, the degloving area irrigated and débrided, and the dead space closed over suction drains. In severe cases, the dead space is packed open, or a vacuum-assisted closure device is selected (Fig. 39.3A,B).
PREOPERATIVE PLANNING
History and Physical Examination
In the hemodynamically unstable patient with an unstable pelvic-ring injury, resuscitation using advanced trauma life support protocols has been shown to reduce morbidity and mortality rates. Large-bore intravenous access allows rapid volume infusion, and the patient is kept warm. The potentially injured pelvis can be immobilized at the accident scene before patient transport through use of a variety of simple techniques. In the past, vacuum beanbags and military antishock trousers were used. More current and less complicated, a simple circumferential pelvic sheet is recommended for initial temporary stabilization of the unstable pelvic-ring injury. Pelvic-wrapping devices are also commercially available but are costly, and they often add to an overloaded inventory. Sheets are readily available, inexpensive, and can be adjusted in width to fit any body habitus. They can be reused or discarded, require no additional inventory, and can be positioned or trimmed to allow groin, perineal, flank, abdominal, or combination access for other resuscitation or evaluation procedures. For some traumatic pelvic-ring injury patterns, the circumferential pelvic sheet produces a perfect manipulative closed reduction when applied snugly. When this occurs, an appropriately located and sized hole in the sheet is cut allowing iliosacral screw insertion and pelvic external fixation pin applications as needed. The sheet is then removed once the fixation devices are applied. Regardless of the technique chosen, pelvic overcompression should be avoided.
The pelvic instability physical examination is a single mechanical and visual evaluation performed by an experienced physician and then communicated to the rest of the treatment team. Repetitive examination of pelvic mechanical instability is avoided because it produces pain and can potentially interfere with clot formation. A detailed neurologic examination is documented in alert patients. During the examination of the pelvic area, the surgeon identifies abrasions, contusions, degloving injuries, deformed skin, or open wounds. Obvious contamination is removed, and sterile pressure dressings are applied to open pelvic wounds to diminish ongoing bleeding. Packing an open pelvic wound decreases bleeding but the packing material should be sterile and easily retrievable. Kerlix rolled sterile gauze allows the open wound to be packed, and a portion of the roll should extrude from the wound so that it is easily identifiable. So that the pelvic packing material is always accounted for, the ends of the Kerlix rolls are tied securely together if more than one roll is necessary to pack the open wound. The lumbosacral palpation and visual, along with the digital rectal examinations, are performed during the posterior spine assessment after the patient has been log rolled by a team of assistants.
The mechanical evaluation of the pelvis is ideally performed under fluoroscopic imaging. Pelvic-ring instability is noted as gentle manual pressure is applied simultaneously toward the midline over each iliac crest. This maneuver produces significant pain in alert patients with pelvic-ring instability, iliac fractures, and certain acetabular fractures. Local pain during iliac manual compression can also be due to iliac area contusions in the absence of pelvic-ring osseous injury. To prevent fracture-surface clot disruptions (among other potential consequences), vigorous and repetitive, manual, pelvic examinations are not recommended. Digital rectal, prostatic, and vaginal examinations are performed to test for both gross and occult blood. The vaginal and rectal exams are initially done with the patient supine or log rolled into the lateral position. A more thorough speculum vaginal exam is deferred until pelvic stability is achieved so the patient can be placed safely in the lithotomy position.
Imaging Studies
The radiographic assessment begins with a screening, anteroposterior (AP), plain radiograph of the pelvis. A complete radiographic series include orthogonal views (inlet/outlet), and a lateral sacral image should be obtained especially in patients whose screening AP films show a “paradoxical inlet” of the upper-sacral area. The “paradoxical inlet” appearance indicates either traumatic upper-sacral transverse fractures or normal yet excessive lumbosacral lordosis. A CT scan of the pelvis is essential to further delineate the fracture anatomy. The CT scan images of the pelvis indicate the patient’s body habitus, reveal related soft-tissue abnormalities, such as hematoma, as well as degloving injuries and their extent, and also show contrast extrusions reflecting bladder, vascular, or other injuries. The pelvic CT images also show the lumbosacral nerve-root positions as well as sacral alar fractures. The iliac vessels and their relationship with displaced, superior-pubic ramus fractures are often seen clearly on the images. With similar clarity, displaced inferior-ramus fractures can be identified as they intrude on the vagina or are displaced anteriorly. The CT scan details subtle osseous injuries missed on the plain films and shows the hemipelvic displacement patterns. Similar to the CT findings for an open pelvic wound, an ipsilateral pneumothorax can often be seen on CT scans of the pelvis because the subcutaneous air extends to the iliac area (Fig. 39.4).
Timing of Surgery
The timing of pelvic reduction and fixation is primarily dependent on the clinical condition of the patient, institutional capabilities, and surgeon availability and expertise. Many patients with unstable pelvic-ring injuries have other injuries that may require urgent surgery. For these patients, pelvic reduction and fixation should be accomplished at the same anesthesia using a coordinated plan with the other surgical teams. Planning would include patient positioning, operating table selection, necessary imaging, procedure prioritization and sequencing, and other details. For example, if the urology consultants are planning urgent repair of the patient’s bladder injury, the orthopedic surgeon could use the opportunity to reduce and stabilize the anterior and posterior unstable pelvic-ring injuries when possible. Hemodynamically unstable patients with unstable pelvic-ring injuries require some form of rapid pelvic stabilization. Anterior-pelvic external-fixation frames and posterior-pelvic antishock clamps have been advocated to stabilize the pelvic ring rapidly. When possible, the pelvic external-fixation system is applied through use of iliac crest or pelvic brim pins inserted after a closed reduction is obtained and maintained by the circumferential pelvic wrap. Access holes are cut in the sheet overlying the iliac crest. The skin is prepped, and the pins are inserted between the iliac cortical tables or within the pelvic brim from the anterior inferior iliac spine. We recommend application of such external devices using the fluoroscopy unit in the operating room when possible. The circumferential wrap can also be adjusted through use of the same imaging unit to assess and adjust the pelvic closed-manipulation reduction (Fig. 39.5). If the reduction has been achieved, iliosacral screws can also be inserted using access portals in the sheet. In selected hemodynamically unstable patients, pelvic angiographic embolization is helpful in controlling pelvic arterial bleeding.
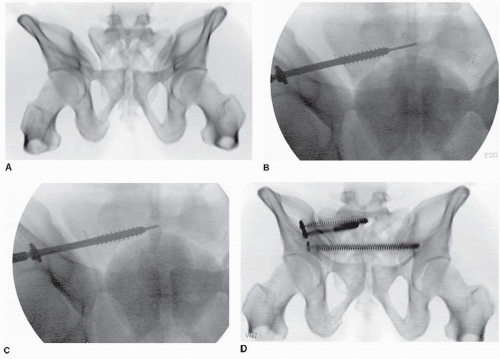
Emergency, pelvic, open reduction and internal fixation induces the risk of bleeding and has a higher complication rate, but for certain patients and injury patterns, the benefits may outweigh the risks. Percutaneous, posterior-pelvic, internal fixation through the use of iliosacral screws minimizes the bleeding risk, is quick, and is useful when an accurate closed-manipulated reduction of the posterior pelvic-ring injury can be accomplished. For some injuries such as SI disruptions, the iliosacral lag screw is inserted as a reduction and fixation device (Fig. 39.6).
Percutaneous iliosacral screws may be used in emergency resuscitation situations in combination with standard anterior-pelvic external fixation. In patients who are hemodynamically stable, operative pelvic stabilization should be done early. Before surgery, distal femoral traction improves the reduction and provides patient comfort.
Surgical Tactic
During the preoperative planning phase, the surgeon should consider the mechanism of injury, associated major-system injuries, and the local soft-tissue conditions. Special attention is given to an analysis of the plain films and CT scans. On occasion, iliac and obturator oblique radiographs of the pelvis are obtained in patients with concomitant acetabular fractures. A two-dimensional (2D) CT scan further delineates the specific sites of injury and direction of displacement. Just as important as detailing the injury and local anatomy, the 2D CT scan also is used preoperatively to determine the number of screws that can be inserted, the upper-sacral anatomy, the planned starting point on the lateral ilium, and the screw direction and length needed to achieve stable and balanced fixation. The CT scan sagittal reconstructions demonstrate the specific upper-sacral anatomy facilitating planning such as the amount of intraoperative tilt needed for inlet imaging (Fig. 39.7A,B).
Some clinicians prefer three-dimensional (3D) CT scans to improve their understanding of the osteology, fracture details, and deformity patterns, but these should not be studied alone and instead must be correlated with the axial images (Fig. 39.8A,B).
Based on the mechanism of injury, the physical examination, and the radiographic studies, the surgeon formulates a plan. The preoperative plan includes all of the surgical details including timing, coordination with other surgical treatment teams, equipment needs, patient positioning, prepping and draping, exposures, reduction strategies, clamp application sites, fixation techniques, and treatment alternatives. Even the anticipated rehabilitation goals are planned preoperatively; they are especially important for polytraumatized patients.
Not all posterior pelvic fractures, especially certain larger crescent iliac fractures, are amenable to iliosacral screw fixation, and the surgeon should be familiar with various anterior-pelvic and posterior-pelvic operative exposures and fixation techniques as well as percutaneous reduction and fixation strategies. The treatment plan must be tailored to the individual patient. Insertion of iliosacral screws can be performed with the patient in the supine, lateral, or prone position; each patient position has advantages and disadvantages. The lateral position complicates both anterior-pelvic and posterior-pelvic surgical exposures and is not recommended for patients with potential spinal injuries. Prone positioning allows posterior surgical exposures but denies the surgeon simultaneous anterior-pelvic surgical access. Anterior-pelvic external-fixation frames further complicate prone and lateral patient positioning for surgery.
If the supine position is selected, strict attention to detail during patient positioning, as well as skin preparation and draping, is mandatory. For most and especially polytraumatized patients, the supine position is simple and familiar; provides easy face-airway-chest-abdominal-perineal access; allows several teams to work simultaneously on injured extremities if needed; and also provides anterior pelvic access. With the supine approach, patient position adjustments and repeated drapings are avoided; thus valuable time is saved.
Computer guidance systems have been available for two decades and, like neurodiagnostic monitoring, are intended to simplify the procedure by making it safer. Unfortunately, computer navigation systems are not a substitute for the surgeon’s thorough knowledge of the sacral anatomy and radiology. Current navigation systems are still being refined in attempts to help surgeons, but the surgeon’s knowledge should always be more extensive than any artificial intelligence device.
 FIGURE 39.8 A,B. Critical information necessary for preoperative planning is not always available on the 3D pelvic CT surface-rendered images. The routine 2D pelvic axial CT images reveal details beyond the bone surface. A. This 3D pelvic image demonstrates the sacral fracture, lumbosacral disc injury, and displacement pattern. B. The contrast-enhanced 2D axial image alerts the surgeon to the relationships between the sacral fracture and both the iliac vascular and lumbosacral neural structures. The axial image also provides information regarding the upper-sacral OFP’s size and orientation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|