Chapter 57 Posterior Cruciate Ligament Reconstruction
Transtibial Double-Bundle Technique
Posterior cruciate ligament (PCL) surgical reconstruction may be unsuccessful because of failure to recognize and treat associated ligament instabilities (posterolateral instability and posteromedial instability), failure to treat varus osseous malalignment, and incorrect tunnel placement.32–34 The keys to successful PCL reconstruction are to identify and treat all pathology, utilize strong graft material, accurately place tunnels in anatomic insertion sites, minimize graft bending, use a mechanical graft tensioning device, use primary and backup graft fixation, and employ the appropriate postoperative rehabilitation program. Adherence to these technical points results in successful single- and double-bundle arthroscopic transtibial tunnel (TTT) PCL reconstruction, documented by stress radiography, arthrometer, knee ligament rating scales, and patient satisfaction measurements.7–9,11,13–16,18–25,29 The purpose of this chapter is to describe our surgical techniques for arthroscopic TTT PCL reconstruction and posterolateral reconstruction.
The incidence of PCL injury is reported to range from 1% to 40% of acute knee injuries. Incidence is dependent on the patient population reported and is approximately 3% in the general population and 38% in reports from regional trauma centers.3,6,17 Our practice at a regional trauma center has a 38.3% incidence of PCL tears in acute knee injuries, and 56.5% of these PCL injuries occur in multiple-trauma patients. Of these PCL injuries, 45.9% are combined anterior cruciate ligament (ACL)/PCL tears, and 41.2% are PCL/posterolateral corner tears. Only 3% of acute PCL injuries seen in our trauma center are isolated.
Surgical Indications
Double-bundle/double–femoral tunnel (DB/DFT) TTT PCL reconstruction approximates the anatomy of the PCL by reconstructing the anterolateral and posteromedial bundles of the PCL. This double-bundle reconstruction more closely approximates the broad femoral insertion of the PCL, enhancing the biomechanics of PCL reconstruction.30 Although the DB/DFT TTT PCL reconstruction does not perfectly reproduce the normal PCL, certain components lead to success with this surgical technique:
Surgical Timing
The surgical timing guidelines outlined previously should be considered in the context of the individual patient. Many patients with multiple-ligament injuries of the knee are severely injured multiple-trauma patients with multisystem injuries. Modifiers to the ideal timing protocols outlined earlier include the vascular status of the involved extremity, reduction stability, skin condition, open or closed injury, and other orthopedic and systemic injuries. These additional considerations may cause knee ligament surgery to be performed earlier or later than desired. We have previously reported excellent results with delayed reconstruction in the multiple ligament–injured knee.*
Posterior Cruciate Ligament Reconstruction Surgical Technique
The patient is positioned on the operating table in the supine position, and the surgical and nonsurgical knees are examined under general or regional anesthesia. A tourniquet is applied to the operative extremity, and the surgical leg is prepped and draped in a sterile fashion. Allograft tissue is prepared before the surgical procedure is begun, and autograft tissue is harvested before the arthroscopic portion of the procedure is undertaken. Standard arthroscopic knee portals are used. The joint is thoroughly evaluated arthroscopically, and the PCL is evaluated using the three-zone arthroscopic technique.4,25 The PCL tear is identified, and the residual stump of the PCL is débrided with hand tools and the synovial shaver.
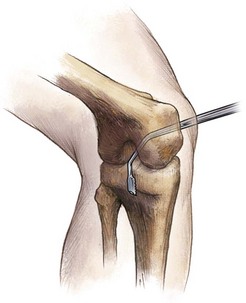
An extracapsular posteromedial safety incision approximately 1.5 to 2.0 cm long is created.9,11,13–16,18–25,29 The crural fascia is incised longitudinally, with precautions taken to protect the neurovascular structures. The interval is developed between the medial head of the gastrocnemius muscle and the posterior capsule of the knee joint, which is anterior. The surgeon’s gloved finger is positioned so that the neurovascular structures are posterior to the finger, and the posterior aspect of the joint capsule is anterior to the surgeon’s finger. This technique enables the surgeon to monitor surgical instruments such as the over-the-top PCL instruments and the PCL/ACL drill guide as they are positioned in the posterior aspect of the knee. The surgeon’s finger in the posteromedial safety incision also confirms accurate placement of the guide wire before tibial tunnel drilling is begun in the medial-lateral and proximal-distal directions (Fig. 57-1). This is the same anatomic surgical interval that is utilized in the tibial inlay posterior approach.
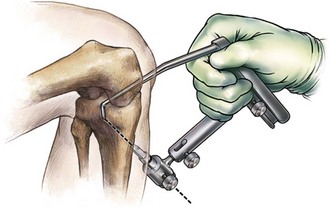
Curved over-the-top PCL instruments are used to elevate the posterior knee joint capsule away from the tibial ridge on the posterior aspect of the tibia. This capsular elevation enhances correct drill guide and tibial tunnel placement (Fig. 57-2).
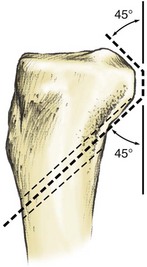
The arm of the Biomet Sports Medicine PCL-ACL drill guide (Biomet Sports Medicine, Warsaw, Ind) is inserted into the knee through the inferior medial patellar portal and is positioned in the PCL fossa on the posterior tibia (Fig. 57-3). The bullet portion of the drill guide contacts the anterior medial aspect of the proximal tibia approximately 1 cm below the tibial tubercle, at a point midway between the tibial crest anteriorly and the posterior medial border of the tibia. This drill guide positioning creates a tibial tunnel that is relatively vertically oriented and has its posterior exit point in the inferior and lateral aspect of the PCL tibial anatomic insertion site. This positioning creates an angle of graft orientation such that the graft will turn two very smooth 45-degree angles on the posterior aspect of the tibia (Fig. 57-4).
The PCL femoral tunnel may be created from outside in or from inside out. When the PCL femoral tunnel is created from outside in, the PCL/ACL drill guide is positioned to create the femoral tunnel. The arm of the guide is introduced through the inferomedial patellar portal and is positioned in such a way that the guide wire will exit through the center of the stump of the anterior lateral bundle of the PCL (Fig. 57-5A and B). The spade-tipped guide wire is drilled through the guide, and just as it begins to emerge through the center of the stump of the PCL anterior lateral bundle, the drill guide is disengaged. Accuracy of placement of the wire is confirmed arthroscopically with probing and visualization. By arthroscopically examining the patellofemoral joint prior to drilling, care is taken to ensure that the patellofemoral joint has not been violated, and that the distance between the femoral tunnel and the medial femoral condyle articular surface is adequate. An appropriately sized standard cannulated reamer is used to create the femoral tunnel. A curette is used to cap the tip of the guide wire, so no inadvertent advancement of the guide wire occurs; this movement may damage the ACL or the articular surface. As the reamer is about to penetrate interiorly, the reamer is disengaged from the drill and the final reaming is completed by hand. This provides an additional margin of safety. The reaming debris is evacuated with a synovial shaver to minimize fat pad inflammatory response with subsequent risk of arthrofibrosis. The tunnel edges are chamfered and rasped.
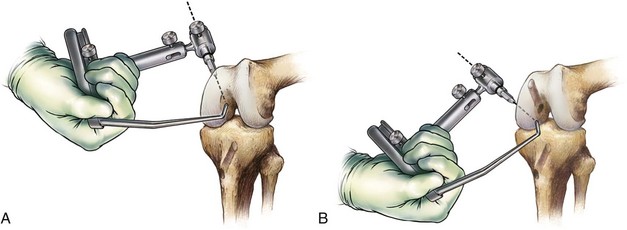
The author’s preferred method is to perform a double-bundle PCL reconstruction by making the PCL femoral tunnels from inside out. PCL single-bundle or double-bundle femoral tunnels are made from inside out using the Biomet Sports Medicine double-bundle aimers. Inserting the appropriately sized double-bundle aimer through a low anterior lateral patellar arthroscopic portal creates the PCL anterior lateral bundle femoral tunnel. The double-bundle aimer is positioned directly on the footprint of the femoral anterior lateral bundle PCL insertion site. An appropriately sized guide wire is drilled through the aimer, through the bone, and out a small skin incision. Care is taken to ensure that there is no compromise of the articular surface. The double-bundle aimer is removed, and an acorn reamer is used to endoscopically drill from inside out the anterior lateral PCL femoral tunnel. The tunnel edges are chamfered and rasped. The reaming debris is evacuated with a synovial shaver to minimize fat pad inflammatory response with subsequent risk of arthrofibrosis. The same process is repeated for the posterior medial bundle of the PCL. Care must be taken to ensure that an adequate bone bridge (approximately 5 mm) will be present between the two femoral tunnels prior to drilling. This is accomplished using the calibrated probe and direct arthroscopic visualization (Fig. 57-6A and B).
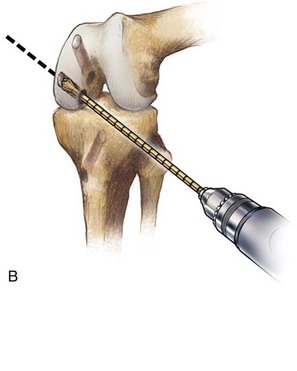

Figure 57-6 A, Biomet Sports Medicine double-bundle aimer positioned to drill a guide wire for creation of the posterior cruciate ligament (PCL) posteromedial bundle femoral tunnel through the low anterolateral portal. B, Endoscopic acorn reamer is used to create the posterior cruciate ligament (PCL) posteromedial bundle through the low anterolateral patellar portal.
(With permission, Biomet Sports Medicine, Inc., Warsaw, Ind.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree