Posterior Cervical Fusion with Instrumentation
Raj Rao
Satyajit V. Marawar
SURGICAL MANAGEMENT
Operative intervention in the posterior subaxial cervical spine is frequently carried out for decompression or stabilization.
Fusion and instrumentation of the posterior cervical spine may be required for unstable fractures or after extensive decompressive procedures.
Instrumentation reduces the need for postoperative immobilization and orthosis wear, augments fusion success, and allows better maintenance of sagittal alignment of the cervical spine.
Interspinous Wiring
Interspinous wiring can be an alternative to lateral mass or pedicle screw fixation in stabilization of the posterior cervical spine.
Although it resists flexion reasonably well, it is generally not as strong in resisting extension, axial load, rotation, and lateral bending.
The most commonly used implants are 18- or 20-gauge stainless steel wire or 1- to 1.2-mm titanium braided cable.
Alternatives include braided stainless steel or polyethylene cable. Multistrand braided steel, titanium, or polyethylene cables show superior fatigue resistance, greater flexibility, and improved stability on flexion-extension testing compared to a single-filament stainless steel wire.38,44
In modern spine surgery, wiring techniques are g enerally limited to cases in which biomechanically superior techniques such as lateral mass fixation cannot be used, a somewhat less invasive midline-only exposure is desired, or the additional rigidity of lateral mass fixation is not necessary (eg, for posterior repair of relatively stable pseudarthroses or to provide a tension band effect as an adjunct to anterior instrumentation).
Techniques of wiring include simple interspinous wiring (eg, Rogers), Bohlman triple wiring (can be used also for occipitocervical fixation), and oblique wiring.
As a result of the direction of its stabilizing forces, oblique wiring may counter rotational instability better than simple interspinous wiring.
Lateral Mass Screw Fixation
The lateral mass of the subaxial cervical vertebra is a quadrangular column of bone formed by the complex of the superior and inferior articular processes and the intervening bone.
Lateral mass screws are the most commonly used and widely evaluated implants for posterior fixation of the subaxial cervical spine.
Lateral mass screws are versatile in that they can be used when the spinous processes and laminae are unavailable as fixation points (eg, from trauma, tumors, or surgical resection for decompression).
Lateral mass screw fixation techniques provide superior flexion and torsional stiffness compared to posterior wiring.8,42
The improved strength of fixation allows instrumentation to be limited to the levels of fusion. When wiring techniques are used, the construct occasionally needs to be extended proximally or distally to obtain additional points of fixation.
A lower incidence of postoperative kyphosis is achieved with lateral mass screws versus wiring techniques.13
Lateral mass screws are easier to insert and have a low incidence of complications when compared to pedicle screws.
The Magerl technique of lateral mass screw fixation has been shown to have superior pullout strength and higher load to failure when compared to screws inserted with the Roy-Camille technique.30 This may be related to the longer screw length generally possible with the Magerl technique.
Anatomic variations in screw lengths occur at each subaxial level, with either technique; from C3 to C6, the Magerl technique can safely afford a screw length of 14 mm as compared to the Roy-Camille technique which can afford a screw length of 12 mm. At C7, the reported screw lengths are 2 mm shorter for the Roy-Camille technique and 3 to 4 mm shorter for the Magerl technique. Screw lengths are greater in males compared to females at all levels. Assessment of lateral masses on preoperative computed tomography (CT) scans is recommended to ascertain screw lengths while using either technique.9,39
Pullout strength is significantly greater with a bicortical screw than with a unicortical purchase.
Because bicortical purchase engenders potential risk to nerve roots and the vertebral artery, unicortical purchase is used in most cases.
Pedicle Screw Fixation of the Cervical Spine
Pedicle screw fixation allows simultaneous stabilization of all three columns of the cervical spine and has been reported to be biomechanically superior to lateral mass fixation.20
Although cervical pedicle screws are commonly used in Asian countries, they are not as popular in United States. The risk of neurovascular injury from broaching the walls of the small cervical pedicles from C3 to C6 and variability in pedicle size sometimes even at the same level (FIG 1) makes this procedure technically difficult and restricts its widespread use.12,21,32,33
Pedicle screws are most commonly used at C2 and C7 where the pedicles are largest in the cervical spine and the risk of neurovascular injury is lower.
At C7, most patients do not generally have a vertebral artery in the foramen transversarium, making pedicle screw fixation safer at this level.
At C2, the vertebral artery is generally lateral to the insertion site and trajectory of the pedicle, making pedicle screw fixation feasible.
From C3 to C6, the proximity of the vertebral artery and the small diameter of the pedicles make pedicle screw fixation challenging and not feasible for routine use.
Whenever pedicle screw fixation in the cervical spine is contemplated, careful scrutiny of preoperative CT and magnetic resonance imaging (MRI) scans is essential to measure the dimensions and angulation of the pedicles and rule out congenital anomalies.
The cervical pedicle is generally taller than it is wide, with the mean height of all cervical pedicles around 7 mm (range 6 to 11 mm).12,32,33
The width of the pedicle is the critical dimension for feasibility of pedicle screw placement.
Pedicle outer diameters less than 4 mm generally preclude pedicle screw insertion.12
Multiple morphologic studies have found that the mean cervical pedicle outer width varies from 4 to 7 mm, with significant variation in the width at different levels (Table 1).12,28,32,33
The pedicles of C2 and C7 are however generally large enough to accommodate either 3.5- or 4-mm screws.
The length of the pedicles from C3 to C6 ranges from 12 to 18 mm.12,33 Screw lengths are generally slightly longer to obtain purchase within the vertebral body.
The axial angle of the pedicle (medial angle to the sagittal plane) is the least at C2 (25 to 30 degrees)10 and increases to a mean of 44 degrees (25 to 55 degrees) at C3. From C3 to C7, it gradually reduces to a mean of 37 degrees (33 to 55 degrees).28
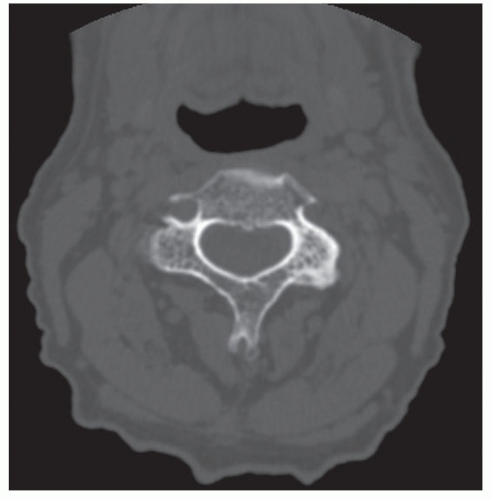 FIG 1 • Axial CT image of a subaxial cervical vertebra depicting variability in the pedicle diameter at the same level. |
Table 1 Cervical Pedicle Outer Width | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TECHNIQUES
▪ Posterior Cervical Fusion
Although it is tempting to focus on instrumentation techniques, performing a meticulous fusion technique is just as important, if not more so, to the success of surgery.
In virtually all cases, posterior fusion is supplemented by some form of instrumentation.
To maximize the surface area for fusion, all posterior bony surfaces that do not need to be resected for the decompression should be left intact for fusion.
Following exposure, all soft tissues, including the interspinous ligaments and muscles, facet joint capsules, and paraspinal soft tissue, are meticulously resected so that the posterior cortical surfaces lie exposed.
In patients who require a laminectomy, the lateral masses and facet joints form the fusion bed.
Facet joint cartilage is removed with a curette or 3-mm burr within the facet joint. It is easier to decorticate the facet joints if done before the insertion of lateral mass screws.
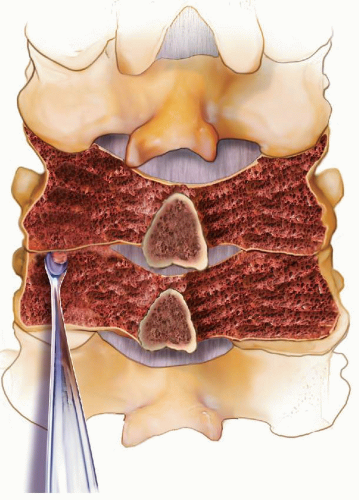
The posterior cortical surfaces of the lateral masses, laminae, and spinous processes are decorticated with a 3-mm burr to expose bleeding subcortical bone (TECH FIG 1).
Bone graft obtained from the iliac crest or local bone from laminectomy is morselized into small cancellous and corticocancellous chips and onlaid over the bleeding bone.
Cancellous chips of bone are inserted directly into the facet joint.
▪ Interspinous Wiring
Simple Interspinous Wiring
The spinous processes and laminae at the level to be instrumented should be confirmed to be intact and instrumentable on preoperative imaging studies.
Closed or operative reduction of spinal fracture-dislocations should be carried out before instrumentation if possible.
In some cases of flexion-distraction injury, sequential tightening of the wires can be done to reduce the spine.
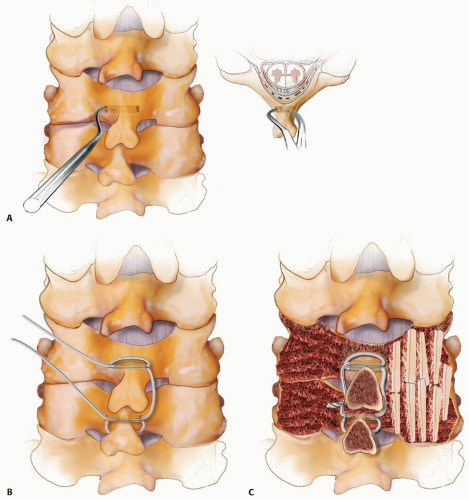
Two- to 3-mm drill holes are made through the cortex at the junction of the spinous process and laminae bilaterally at the levels to be included in the fusion.
Attention should be paid to the ventral location of the dural sac, and the drill should be directed coronally to minimize the risk of inadvertent spinal cord injury (TECH FIG 2A).
The drill holes should be positioned at the proximal aspect of the cephalad spinous process and the distal aspect of the caudal spinous process to provide the widest margin of safety against the wire cutting through the spinous process.
The tips of a towel clip or a tenaculum clamp are placed in the cortical holes on either side of the base of the spinous process.
A gentle side-to-side rocking movement is used to create a continuous tract in the cancellous bone at the base of the spinous process.
The wire or cable selected for use is passed through and around the base of the cranial spinous process (TECH FIG 2B).
One end of this wire is similarly passed through and around the base of the caudal spinous process so that both the ends of the wire end up on the same side of the spine.
The free ends of the wire are tightened (TECH FIG 2C).
Cancellous bone graft is placed bilaterally on the decorticated laminae and spinous processes and within the facet joint at the fusion levels.
Modification of the technique can include a plate of corticocancellous bone graft harvested from the iliac crest and placed under the wire or cable bilaterally prior to tightening.
Triple Wire Technique
The wire or cable selected is passed through and around the spinous processes at the cephalad and caudal ends of the fusion levels, as with routine interspinous wiring.
A pair of corticocancellous plates of bone graft including the full thickness of the cancellous bone of the iliac crest but excluding the inner cortical table is harvested from the posterior iliac crest.
The length of the bone block should be adequate to span the fusion construct and wide enough to cover the decorticated laminae within the fusion levels.
Two- to 3-mm drill holes are created in the proximal and distal portions of the harvested bone grafts.
Two additional 22-gauge wires are passed through the holes in the proximal and distal spinous processes.
These wires are then passed on either side through the holes made in the bone graft.
The wires are tightened over the grafts on both sides to hold the bone graft rigidly against the decorticated lamina and spinous process (TECH FIG 3).
Oblique Wiring
A periosteal elevator is carefully inserted into the facet joint to slightly distract and clearly identify the plane of the facet joint.
A 2-mm drill bit is used to make a channel in the sagittal plane through the midportion of the inferior articular process, exiting through the articular surface into the joint.
The periosteal elevator within the joint confirms penetration by the drill and prevents overpenetration by the drill (TECH FIG 4A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree