Posterior and Multidirectional Instability: Open Solutions
Suzanne Miller
Evan L. Flatow
S. Miller: University of Pittsburgh Medical Center, Center for Sports Medicine, Pittsburgh, Pennsylvania.
E. L. Flatow: Mount Sinai School of Medicine, New York, New York.
INTRODUCTION
Posterior and multidirectional shoulder instability are challenging shoulder problems to treat. This is due, in part, to the difficulty we encounter making correct diagnoses. For example, distinguishing between asymptomatic laxity and true symptomatic instability may be difficult. Arthroscopy and magnetic resonance imaging (MRI) have documented a wide variety of labral lesion, ligament variations, and associated rotator cuff injuries, the significance of which are debated. Once diagnosed, posterior and multidirectional instability can be difficult to treat. The frequently large degree of capsular redundancy may be hard to rebalance without asymmetric tightening, and healing in patients with generalized laxity can be unpredictable. Finally, motivational problems, especially voluntary or positional components of the symptoms, are more common with posterior instability and can frustrate attempts at surgical correction.
PATHOANATOMY
The static stabilizers of the glenohumeral joint include the bony architecture, capsuloligamentous structures, and the labrum. The dynamic stabilizers include the biceps and rotator cuff musculature.
The bony architecture of the glenohumeral joint is such that the two surfaces are almost congruent due to the thicker articular cartilage at the periphery of the glenoid.33,46 Because the articular surface of the humeral head is three times that of the glenoid, only 25% to 30% of the humeral head is in contact with the glenoid at any one position of the shoulder. This helps explain why the glenohumeral joint has the greatest range of motion of any joint in the human body and thus has a greater tendency to be susceptible to instability. Any change in the contour or orientation of the glenoid can disrupt the normal relationship between the articular surfaces and, subsequently, lead to instability. Some have attributed etiologies, such as anterior humeral head defects (reverse Hill-Sachs lesion), increased proximal humerus retroversion, glenoid abnormalities (hypoplasia and increased retroversion), or glenoid fracture to shoulder instability.41
It is unclear how much of a role increased glenoid retroversion accounts for in recurrent posterior subluxation.
Several series have found increased retroversion on computed tomography (CT) imaging in patients with posterior subluxation10,27 while others have not.19,43 In one series, localized glenoid hypoplasia was seen as an incidental finding in 18% of a New York population. Criteria for diagnosis was deficiency less than 1.2 cm below the scapular spine on axial CT imaging.13 Using the same criteria in a prospective manner, the study found that 9 of 12 patients with multidirectional instability had localized hypoplasia at the posteroinferior glenoid. Still, at the present time, most investigators feel that the bony architecture probably plays a relatively small role in instability.
Several series have found increased retroversion on computed tomography (CT) imaging in patients with posterior subluxation10,27 while others have not.19,43 In one series, localized glenoid hypoplasia was seen as an incidental finding in 18% of a New York population. Criteria for diagnosis was deficiency less than 1.2 cm below the scapular spine on axial CT imaging.13 Using the same criteria in a prospective manner, the study found that 9 of 12 patients with multidirectional instability had localized hypoplasia at the posteroinferior glenoid. Still, at the present time, most investigators feel that the bony architecture probably plays a relatively small role in instability.
Despite the controversy over bony architecture as the etiology of instability, numerous bony surgical procedures have been described to treat instability. Most are of historical interest. Osseous procedures, including proximal humeral rotation osteotomy and opening-wedge glenoid osteotomy, have had historically poor results with recurrence rates up to 50%.26 Most of these procedures addressed unidirectional (either anterior or posterior) instability, leaving a large redundant inferior capsular pouch, which may account for high failure rates in patients with posteroinferior or multidirectional instability.
The glenoid labrum also plays a role in glenohumeral stability by increasing the depth of the glenoid and by acting as an anchor for the capsuloligamentous structures. Lippitt31 reported that the loss of the labrum reduced resistance to inferior and posteroinferior translation is approximately 20%. The superior labrum has also been shown to add inherent stability to glenohumeral translation in the anteroposterior plane of motion. In a cadaveric study, lesions created in the superior labrum anterior posterior, “SLAP tears,” led to increases in glenohumeral translation.40
The capsuloligamentous restraints to the glenohumeral joint have been studied extensively. The ligaments are thickenings of the capsule and are primarily comprised of type 1 collagen. The stability that the ligaments provide is complex and changes according to arm position and direction of load. When the shoulder is in midrange the capsular ligaments are relatively lax, whereas in extreme positions of internal and external rotation, they become more taught, thus limiting translations and excessive rotation.48 The anatomy of the inferior glenohumeral ligament is more constant, whereas that of the superior and middle glenohumeral ligaments is more variable. Recently, a biomechanical study,9 with the arm at 90 degrees of forward flexion, found that the coracohumeral ligament was a contributor to posterior stability with the arm in neutral rotation, and the inferior glenohumeral ligament (IGHL) was an effective contributor to posterior instability in internal humeral rotation.
The material properties of the capsuloligamentous structures have also been investigated. Bigliani et al.,7 in a cadaveric model, found that the IGHL undergoes significant deformation before failure, which supports the clinical finding that repetitive microtrauma can stretch the capsule and lead to instability. This finding may also help explain acquired laxity that allows certain athletes, to function at such extreme ranges of motion with no pain. Warren showed in a cadaver sectioning study that for posterior dislocation to occur there must be injury at the anterior superior portion of the capsule.52 He termed the injury the “circle concept,” meaning that during a severe subluxation or dislocation episode, capsular injury takes place on both the anterior and posterior aspects of the glenohumeral joint.
There are several dynamic stabilizers of the glenohumeral joint. The rotator cuff musculature provides joint compression and acts as a humeral head depressor resisting the upward pull of the deltoid. The biceps also helps to maintain stability39; with the shoulder in internal rotation, the biceps stabilizes anteriorly, and, in external rotation, posteriorly.
Currently, capsular laxity is felt to be the primary etiology of recurrent multidirectional or posterior instability and has been the most common finding at surgery in the majority of series.6,35 This is often seen as a manifestation of recurrent microtrauma in athletes who use their arm in the provocative position. For example, a predominantly posterior instability pattern may manifest in an athlete who spends a lot of time with the shoulder in flexion, adduction, and internal rotation. Injury can occur as both an impact loading mechanism, which can be seen in offensive lineman, weightlifters, and boxers, and as a traction mechanism, seen in the follow-through phases of throwing and swimming. Recently, two series of patients with shoulder contact injuries reported posterior labral detachment 100% of the time with no capsular injury.32,53 Otherwise, posterior labral detachment has been an uncommon finding in most series.6
SURGICAL INDICATIONS AND OTHER OPTIONS
The primary indication for surgery in patients with posterior or multidirectional instability is in patients with prolonged disability or pain due to recurrent dislocation or subluxation who have undergone a trial of nonoperative treatment. It must be emphasized that most patients should improve with a trial of physical therapy that focuses on rotator cuff and scapulothoracic strengthening. For a successful surgical outcome, patients must be able to tolerate postoperative immobilization and follow physical therapy guidelines.
With newer arthroscopic techniques, capsular plication and labral repair are now possible.1,55 The literature on
arthroscopic posterior plication is still relatively new, but success rates reported are in the range of 84% to 90%.3,34,55
arthroscopic posterior plication is still relatively new, but success rates reported are in the range of 84% to 90%.3,34,55
Stiffness is not usually a common complication after an open procedure to address posterior or multidirectional instability; recurrent instability, however, is.23,24,29 In addition, with both arthroscopic and open surgical techniques to address multidirectional instability, immobilization of the arm for 6 weeks is fairly standard. Open capsulorrhaphy also allows thickening and overlap of the capsular flaps and frees the external surface of capsule from adjacent structures, allowing more substantial shifting. With this in mind, the indications for arthroscopic treatment are less clear.
In primary cases, open repair can address bony deficiency and osseous abnormalities. In addition, we feel it is advantageous in those who wish to return to contact sports, those with inferior capsular laxity, and those who wish the best success and least chance of recurrence with only one operation.
For revision instability surgery, the current literature regarding results of arthroscopic treatment is sparse. Antoniou reported poor results with arthroscopic posteroinferior shift as a revision procedure. Only 2 of 9 patients had no postoperative instability, and 7 of 9 said that the shoulder felt stiffer. Simple Shoulder Test improved from 5.2 ± 3.9 to 6.9 ± 4.2, which was not significant. Open revision surgery for instability has also had less success than primary cases.6 When primary surgery has failed, it is often the case that a more extensive procedure is necessary, requiring bone grafting or extra-articular augmentation with either allograft or autograft as an open procedure. Recently, thermal necrosis as a complication of thermal capsulorrhaphy has necessitated open surgery to augment insufficient tissue with either autograft or allograft.
Nonetheless, the decision for open versus arthroscopy capsulorrhaphy is controversial when the bony architecture is “normal” and the capsular tissue is “adequate.” The arthroscope is a useful instrument when addressing cases that deal with true multidirectional instability, where an anterior and a posterior shift will be necessary. For example, if the primary pathology or direction of instability is posterior, addressing any anterior laxity or a Bankart lesion might be best done through the arthroscope followed by an open posteroinferior capsular shift. This can potentially lead to decreased morbidity (cosmesis, stiffness) from having both an open anterior and posterior instability procedure. With increasing awareness of superior labral lesions, the arthroscope is also a useful adjunct to treatment, using a combined arthroscopic and open approach. The drawback of this approach is the swelling that occurs after an arthroscopic procedure, making the open procedure more difficult. In addition, if the arthroscopy is performed in the seated position, the open posterior approach would require the surgeon to perform this in the seated position, which is more difficult, or to reposition the patient into the lateral decubitus position.
Contraindications
Voluntary dislocators with underlying psychiatric illness have high rates of failure and are best managed nonoperatively. Patients with locked posterior dislocations can have large defects in the humeral head, which should be managed with muscle transfer or arthroplasty or with osteochondral allografts (see Chapter 5). In addition, active infection and paralysis of the rotator cuff muscles (infraspinatus, teres minor) are contraindications to open instability repair.
PREOPERATIVE PLANNING
History
Careful and thorough history is mandatory because the spectrum of disease is so variable and treatment must be individualized in every case. It is important to determine whether the primary complaint is pain, instability, or both. This is often difficult because complaints can be vague. It is also important to elicit any family history of instability in any joint or any known collagen disorder. Does the patient have a history of subluxations or dislocations in any other joint in the body (patellofemoral, metacarpophalangeal)? Eliciting the timing of the instability and arm position is extremely helpful in making a correct diagnosis. Symptoms with the arm flexed and internally rotated (e.g., pushing open doors) are most likely indicative of posterior instability, whereas pain while carrying heavy bags with the arm in neutral rotation can be a sign of inferior instability. Are the episodes subluxations or dislocations? Was there a traumatic event involved, and what specifically happened? Did the symptom occur after a violent blow in a contact sports situation, or did it occur while reaching for something on a shelf? Voluntary dislocaters with underlying psychiatric illness are very important to identify because surgical treatment in this subset of patients can be less than gratifying. Patients presenting with posterior or multidirectional (posteroinferior) instability have often had anterior instability repairs after being initially misdiagnosed or other procedures to address the posterior instability. Knowledge of the details of previous surgical procedures is imperative. Often hardware, such as staples or screws, have been placed that may need to be removed. The competency of the capsulolabrum must always be questioned when dealing with revision surgery. It is important to restore or correct any abnormal scapulothoracic winging, as this can be a cause of posterior instability. Fortunately, most cases of scapulothoracic winging caused by long thoracic nerve injuries resolve spontaneously. If the winging is persistent, and subsequently causing posterior instability, a pectoralis transfer with or without posterior capsulorhaphy may be necessary to alleviate symptoms.43
Physical Examination
When evaluating the shoulder for posterior or multidirectional instability, it is important to examine for generalized ligamentous laxity as well. Testing is considered positive when the patient can perform 3 of 5 tasks, including approximating the thumb to the volar aspect of the forearm, hyperextension of 2nd metacarpophalangeal (MCP) joint greater than 90 degrees, hyperextension of elbow greater than 10 degrees, knee hyperextension, and the ability to touch the palm to the floor with knees straight. Specific to the shoulder, contour should be observed. For example, if there is infraspinatus atrophy, one might suspect a suprascapular nerve palsy. Observation of any prior surgical scars is important for preoperative planning. Active and passive range of motion should be documented and compared side to side. It is especially important to record whether there is any apprehension throughout the range of motion.
Specific subluxation testing has been described by a number of different methods. We feel the “load and shift” test, with patient supine, is most useful in our hands. To test for posterior instability stabilize the medial border of the scapula and direct the patient’s humerus posteriorly while flexed to 90 degrees, adducted, and internally rotated.
Another useful posterior apprehension test is the jerk test. With the patient sitting supine, the arm is flexed to 90° and internally rotated. The examiner stabilizes the scapula and axially loads the humerus in a posterior direction while moving the arm across the body. A jerk indicates the head has slid off the glenoid posteriorily. A second jerk may occur when the arm is returned to the original location, indicating relocation.
Often the patient feels pain posteriorly rather than a sense of apprehension. The circumduction maneuver for posterior subluxation is also useful, but one must keep in mind that this can be bilateral and is a normal finding in up to 30% of the population. The test is an active one that can be performed by having the patient flex, adduct, and internally rotate. Subluxation occurs between 90 and 120 degrees, with the head spontaneously reducing between 120 and 180 degrees as the arm is abducted. The key point, regardless of the specific maneuver, is to demonstrate any subluxation that recreates symptoms. On the other hand, patients may guard against the exam so significantly as to leave the examiner unsure. The stability of the contralateral shoulder should be assessed for comparison.
It is also important to test for a sulcus sign by pulling on the humerus in a neutrally positioned arm, which is indicative of an inferior component to the instability.38 The sulcus should diminish with external rotation of the humerus due to physiologic tightening of the rotator interval tissues, superior glenohumeral ligament (SGHL) and the coracohumeral ligament. If the sulcus does not diminish, one should be suspicious of a rotator interval injury. The neurovascular status of the patient should always be evaluated and documented. This is particularly true in cases of revision surgery where the secondary surgeon is different from the primary surgeon. The patient should be checked for concomitant lesions, such as acromioclavicular joint arthritis, impingement, rotator cuff pathology, or cervical spine problems. Confusing examinations can be clarified with subacromial or acromioclavicular anesthetic injections.
The scapulothoracic joint should also be examined for any winging. Patients with instability often use the scapulothoracic musculature to try and stabilize the glenohumeral joint,37 which often leads to pain, crepitation, or winging in the scapulothoracic joint. Scapula winging can also be a cause or an exacerbating element of the posterior instability pattern. In some cases, inadequate treatment (strengthening program or muscle transfer) (see chapter 31) may result in failure to achieve a stable glenohumeral joint.
Diagnostic Tests
Plain radiographs can be useful to determine dislocation, humeral or glenoid fractures, bony defects, and old hardware still remaining from prior procedures. Most often in posterior or multidirectional instability, radiographs are usually normal. Usually, plain radiographs in three orthogonal planes are obtained: anteroposterior views in the scapular plane, a lateral view of the scapula (“Y” view), and an axillary view. Additional instability views can be obtained to facilitate preoperative planning. The West Point axillary view is useful to determine whether there are any glenoid rim defects or to see a hypoplastic glenoid. Computed tomography can be useful in assessing the size of reverse Hill-Sachs lesions, glenoid fractures, glenoid size, or version.
Computed tomography arthrography has not correlated well with intraoperative capsular and labral pathology. Magnetic resonance imaging with or without arthrogram is becoming more accurate in assessing the labrum and capsule.
SURGICAL TECHNIQUE
Positions, Special Instruments, and Examination Under Anesthesia
General anesthesia or an interscalene block with supplemental regional anesthesia is administered. Examination under anesthesia is critical because patient guarding while awake often limits the physical examination. The direction of maximal instability should be reconfirmed. An exam of the contralateral shoulder should always be performed
because some translation is often within a normal range for an individual and can be equal on both left and right sides. The patient should be placed in the modified beach chair with a bump under the medial border of the scapula. Draping should allow access to the medial border of the scapula posteriorly, the acromioclavicular joint superomedially, and the coracoid anteriorly. A McConnell arm positioner (McConnell Orthopedic Manufacturing Company, Greenville, TX) can be used to maintain arm position.
because some translation is often within a normal range for an individual and can be equal on both left and right sides. The patient should be placed in the modified beach chair with a bump under the medial border of the scapula. Draping should allow access to the medial border of the scapula posteriorly, the acromioclavicular joint superomedially, and the coracoid anteriorly. A McConnell arm positioner (McConnell Orthopedic Manufacturing Company, Greenville, TX) can be used to maintain arm position.
Open Surgical Procedure
This section will present a modification of the technique of inferior capsular shift originally described for multidirectional instability by Neer and Foster in 1980.38 The technique was designed to reduce capsular volume on the side of instability and to tighten the capsule on the opposite side of the glenohumeral joint.
We perform the approach on the greatest side of instability, which is determined from a combination of the history, physical exam, and an exam under anesthesia (EUA). The majority of the time, as a confirmatory step, we make our determination after the history and physical exam with the EUA.
The advantages of a lateral, T-based shift are that the surgeon can adjust the degree of takedown around the humeral neck while feeling the extent of the inferior pouch. Second, because the capsule is shaped like a funnel, the larger circumference is positioned laterally. A lateral-based shift provides a greater distance for shifting tissue and more capsular overlap. Third, the axillary nerve is not as close. Fourth, independent adjustment of tension, using a “T” capsulorrhaphy, is allowed medial to lateral and superior to inferior. Finally, humeral capsule avulsions can occur, occasionally, and are best treated laterally. In addition, a recent biomechanical cadaveric study compared glenoidversus humeral-based shifts. Using the glenoid-based shift, a significant loss of external rotation at 45 degrees and 90 degrees of glenohumeral elevation was found.14
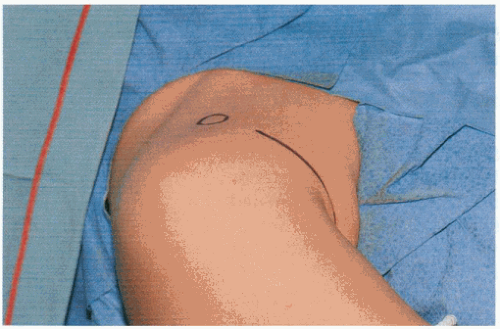 Figure 4-1 A concealed axillary incision begins approximately 3 cm below the coracoid and extends inferiorly for 8 cm into the axillary crease. |
Anterior Shift
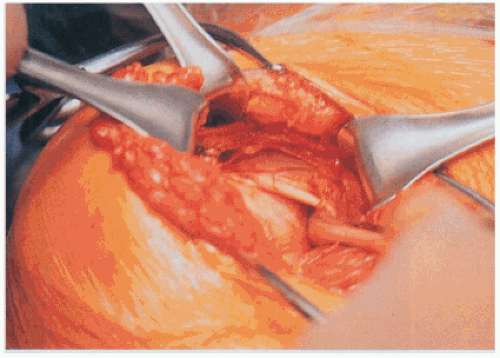
A concealed anterior axillary skin incision, measuring 7 to 8 cm, is made and is used to gain access to the deltopectoral interval (Fig. 4-1). The deltopectoral interval is developed, and the cephalic vein is retracted laterally. Occasionally, 1 cm of the sternal head of the pectoralis may need to be released for visualization. The clavipectoral fascia is incised lateral to the coracoid (Fig. 4-2). A small wedge of the coracoacromial ligament may be removed to better visualize the rotator interval (Fig. 4-3). In revision cases, there can often be extensive scarring in the plane between the clavipectoral
fascia and the subscapularis. Staying lateral to the short head of the biceps facilitates identifying the correct plane.
fascia and the subscapularis. Staying lateral to the short head of the biceps facilitates identifying the correct plane.
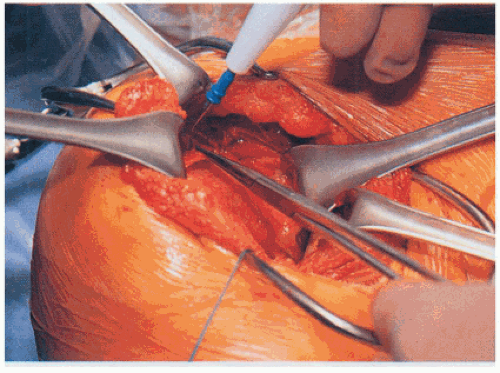 Figure 4-3 A wedge-shaped portion of the coracoacromial ligament is excised for improved exposure on the rotator cuff and upper border of the subscapularis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|