Posterior and Multidirectional Instability: Arthroscopic Solutions
Robert E. McLaughlin
Felix H. Savoie III
Larry D. Field
R. E. McLaughlin: Mississippi Sports Medicine & Orthopaedic Center, Department of Orthopaedic Surgery, University of Mississippi School of Medicine, Jackson, Mississippi.
F. H. Savoie: Mississippi Sports Medicine & Orthopaedic Center, Department of Orthopaedic Surgery, University of Mississippi School of Medicine, Jackson, Mississippi.
L. D. Field: Mississippi Sports Medicine & Orthopaedic Center, Department of Orthopaedic Surgery, University of Mississippi School of Medicine, Jackson, Mississippi.
INTRODUCTION
Posterior and multidirectional instabilities are complex entities that affect the shoulder. Diagnosis and management of these problems can be difficult. Patients affected by these conditions are usually young, active people who are highly motivated to improve, and conservative therapy is usually successful in controlling symptoms. More frequently, however, surgical stabilization is required for these patients to comfortably participate in activities of daily living and sports.
POSTERIOR INSTABILITY
Posterior instability was first described by Rowe and Yee in 1944.32 Recurrent posterior instability has become a more frequent diagnosis over the last decade, but its treatment has proven less successful than its anterior counterpart. This problem, unlike anterior instability, is due to no one essential lesion appearing responsible for posterior instability. In addition, many patients with multidirectional instability have a primary posterior component, further confusing the picture. Until recently, diagnosis and treatment of posterior instability was made difficult by the lack of differentiation between unidirectional versus multidirectional conditions, traumatic versus atraumatic versus microtraumatic causes, voluntary versus involuntary instability, and dislocations versus subluxations. Recent advances in arthroscopic examination techniques, and increased understanding of the anatomy of the shoulder stabilizers, have allowed improved comprehension of posterior shoulder instability.
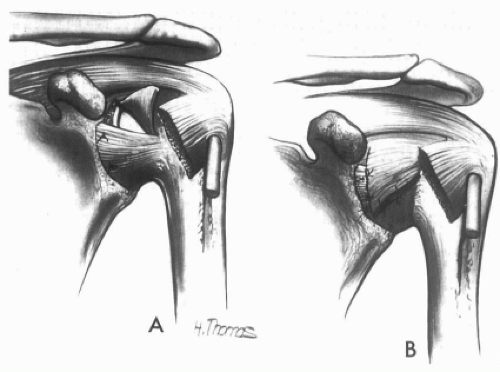
Numerous open operative procedures for treatment of recurrent posterior instability have been reported with failure rates of 30% to 50%. These include bone block (reverse Eden-Hybbinette), glenoid osteotomy, and McLaughlin-type procedures with lesser tuberosity and subscapularis transfer into the reverse Hill-Sachs defect.16 Posterior capsular procedures include reverse Bankart repair, reverse Putti-Platt procedures with or without the infraspinatus tendon, Neer posterior inferior capsular shift, and the Boyd-Sisk procedures.5,16 Combination procedures have tended to give better overall results than pure soft-tissue procedures. Overall, however, the success rate reported with open procedures for posterior instability has not approached the success rate reported for anterior instability.35
MULTIDIRECTIONAL INSTABILITY
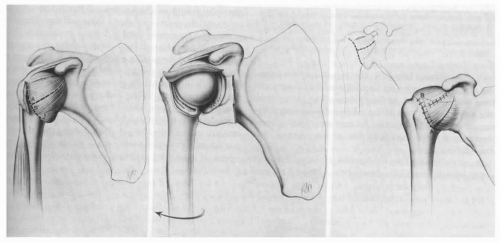
Multidirectional instability (MDI) was originally described by Neer and Foster in 1980.26 They reported on a population of patients that had recurrent shoulder instability and pain associated with instability in all three directions: posterior, anterior, and inferior. A large redundant inferior capsule was identified intraoperatively in all cases, and they reported good results with an inferior capsular shift procedure based laterally on the humeral head. Their procedure, in which the lateral insertion of the inferior half of the shoulder capsule is shifted superolaterally and the superior half is shifted inferolaterally, simultaneously eliminates excessive anterior, inferior, and posterior capsular laxity (Fig. 3-1). Altchek and Warren developed a T-plasty modification in which the shift was based on a medial capsular plication with a superomedial shift of the capsule (Fig. 3-2). The intermediate and long-term results of their superomedial capsular shift have been good, with excellent outcomes occurring in 75% to 100% of cases.2
Caspari developed the first arthroscopic techniques for the treatment of MDI.8,24 This technique shifts the anterior, inferior, and posterior glenohumeral ligaments superiorly with a multiple suture technique. Arthroscopic repair of multidirectional glenohumeral instability has been gaining favor over the last decade with good short-term results being reported by a number of authors.1,37,43
Arthroscopic treatment of both posterior and multidirectional instability has been described, and early results are promising.3,46 This chapter describes patient evaluation and diagnosis, nonoperative treatment, current arthroscopic techniques, and rehabilitation for the treatment of both disorders.
ADVANTAGE OF ARTHROSCOPIC VERSUS OPEN REPAIR
The use of arthroscopy in the diagnosis and treatment of shoulder pathology has grown rapidly over the last decade. There are several advantages to using the arthroscope compared to the open approach. First, arthroscopic surgery is less invasive and produces less musculotendinous damage, aiding in recovery. Second, use of the arthroscope allows for less disturbance of intra-articular anatomy, allowing for more accurate viewing of normal as well as pathological conditions. The entire subacromial space, as well as the intra-articular space, can be visualized with the arthroscope, providing for the simultaneous diagnosis and correction of pathology. In addition, intraoperative modification and final inspection of the repair is also possible. Arthroscopy, therefore, allows pan-articular access to the joint for both diagnosis and stabilization, as well as evaluation, of the repair in the shoulder with minimal soft-tissue morbidity.
ETIOLOGY
The unifying pathomechanical condition of shoulder instability is an increase in glenohumeral translation leading to the development of symptoms. Shoulder stability primarily comes from the glenohumeral ligaments and the rotator interval. Secondary stabilizers include the bony architecture and kinematics, negative intra-articular pressure, glenoid labrum, biceps brachii, rotator cuff muscles, and scapular rotator muscles.
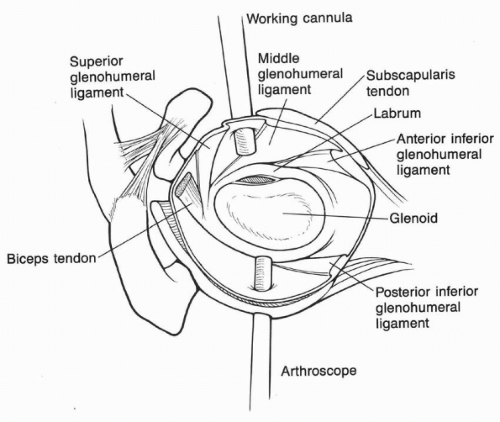
The constraints to posterior instability have been studied by a number of investigators. O’Brien et al. found that the inferior glenohumeral ligament complex (IGHLC), with the posterior inferior capsule, acts as a ligamentous hammock supporting the humeral head and is the primary static stabilizer against posterior instability with the arm in 90 degrees of glenohumeral abduction.28 The relative contributions of the components of the IGHLC change with flexion/extension or rotation of the arm. With the shoulder in 90 degrees abduction and 30 degrees
extension, the anterior band of the IGHLC becomes the prime stabilizer against both anterior and posterior translations. When the 90-degree abducted arm is forward flexed to 30 degrees, the posterior band of the IGHLC becomes the primary anterior-posterior stabilizer (Fig. 3-3). Proper function of each of the three components of the IGHLC is believed to be necessary for normal stability in the position of abduction.29
extension, the anterior band of the IGHLC becomes the prime stabilizer against both anterior and posterior translations. When the 90-degree abducted arm is forward flexed to 30 degrees, the posterior band of the IGHLC becomes the primary anterior-posterior stabilizer (Fig. 3-3). Proper function of each of the three components of the IGHLC is believed to be necessary for normal stability in the position of abduction.29
Schwartz and Warren noted that damage to both the anterior and posterior capsuloligamentous structures was necessary to allow posterior dislocation of the humeral head.36 They found that posterior subluxation occurred with cutting posteriorly from 12 o’clock to 6 o’clock and that dislocation occurred only when the anterior superior portion was also cut. Posterior subluxation also occurred when the entire inferior capsule was cut to include the anterior inferior glenohumeral ligament and posterior inferior glenohumeral ligament (PIGHL). Bigliani et al. found that IGHLC stretching occurs with plastic deformation.7 Ligament failure occurs most commonly at the glenoid insertion and infrequently at the humeral insertion, or midsubstance, of the ligament. Webber and Caspari found that, in patients with posterior instability, the posterior capsule was split horizontally and the labrum was avulsed from the posterior glenoid in the region of the posterior inferior glenohumeral ligament.42
In our review of capsular disease, we support the concept that the anterosuperior and posteroinferior capsuloligamentous structures are the primary contributors to posterior shoulder stability and that there is no “essential lesion” responsible for all cases of posterior instability. We believe that laxity develops in the anterosuperior aspect of the shoulder, as well as in the posteroinferior capsular complex, leading to symptomatic subluxation, also known as the circle concept of posterior instability.
ROTATOR INTERVAL
The rotator interval is also an important structure in maintaining stability of the glenohumeral joint. The rotator interval occupies a triangular space with its apex centered at the transverse humeral ligament over the biceps sulcus and its greatest width located at the base of the coracoid process. The interval space is bordered superiorly by the anterior margin of the supraspinatus tendon and inferiorly by the superior border of the subscapularis tendon, and is usually bridged by the glenohumeral joint capsule. The rotator interval capsule is then structurally enhanced by the coracohumeral ligament (CHL) and superior glenohumeral ligament (SGHL) as it courses from the anterosuperior labrum deep to the substance of the rotator interval capsule and the CHL to insert near the lesser tuberosity (Fig. 3-3).
Harryman et al. have studied the role of the rotator interval in glenohumeral stability in a cadaveric model.15 They found that sectioning the rotator interval capsule allowed for significantly increased laxity in all three directions: anterior, posterior, and inferior. Imbrication of the rotator interval capsule was shown to decrease inferior and posterior humeral head translation to less than that measured in the intact state.
Several clinical studies have also shown the rotator interval capsule’s contribution to stability. Nobuhara and Ikeda reported on a series of patients in whom rotator interval plication was performed for symptomatic glenohumeral instability with good results.27 Rowe and Zarins identified holes in the rotator interval capsule in 20 of 37 patients undergoing open stabilizations for transient subluxations of the shoulder.33 Field et al. reported on 15 patients with clinical examination compatible with MDI in whom the only operative finding at open surgical stabilization was an isolated hole or defect in the rotator interval capsule.11 Closure or imbrication of this rotator interval capsule hole provided for adequate intraoperative stability, and no other stabilization procedures were performed. All of the patients had good or excellent results after an average follow-up of 3.3 years.
LABRUM/BONE DYSPLASIAS
Instability can also be caused by glenoid and/or humeral head dysplasia. When viewing the glenoid en face, its normal shape is similar to a pear, with the lower half being significantly wider than the upper half (Fig. 3-4A). With a large bony Bankart lesion, or even a Bankart lesion without out an associated bone fragment but with a significant impression defect, the shape of the glenoid changes to an
“inverted pear” (Fig. 3-4, B and C), where the superior half of the glenoid is wider than the lower half. In a normal glenoid, a “bare spot” is equidistant between the anterior and posterior rims of the glenoid. Locating this bare spot can be useful when estimating the amount of bone loss arthroscopically. Similarly, an “inverted pear” configuration may be created if a large bony Bankart fragment is removed and the capsulolabral complex is repaired to the remaining glenoid. Both situations require a bony solution to avoid creating a serious containment problem for the shoulder.
“inverted pear” (Fig. 3-4, B and C), where the superior half of the glenoid is wider than the lower half. In a normal glenoid, a “bare spot” is equidistant between the anterior and posterior rims of the glenoid. Locating this bare spot can be useful when estimating the amount of bone loss arthroscopically. Similarly, an “inverted pear” configuration may be created if a large bony Bankart fragment is removed and the capsulolabral complex is repaired to the remaining glenoid. Both situations require a bony solution to avoid creating a serious containment problem for the shoulder.
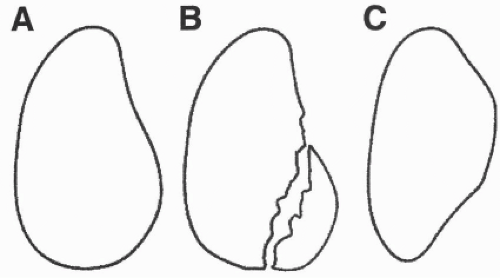 Figure 3-4 (A) Outline of pear-shaped glenoid. (B) Outline of bony Bankart. (C) Deficient anterior inferior glenoid rim. |
Two geometric factors exist with regard to containing the humeral head by the glenoid. First, the anterior rim and labrum serve to “deepen the dish” of the glenoid by increasing the length of arc and widening the glenoid. Loss of the anterior rim creates a shallower “dish” and, in effect, a shorter arc of motion with less resistance to shear forces. Therefore, less shear force is required to cause a dislocation. Second is the arc length required to resist axial forces; the bony portion of the glenoid resists axial forces until the anterior rim is reached. At this point, axial forces are resisted by the capsulolabral structures. With an “inverted pear” type glenoid, a shorter arc of bony buttress exists to resist the axial loads than that of a normal glenoid. Subsequently, the repaired glenohumeral ligaments are subjected to higher loads and predisposed to disruption and recurrent instability.
The anterior labrum plays a key role in anterior stability. The role of the posterior labrum, however, is less well defined. In general, Harryman et al. have shown the entire labrum to contribute to shoulder stability, providing 10% of the stabilization by deepening the concavity of the glenoid.14 We believe that the intact or reconstructed labrum provides a biofeedback to the rotator cuff musculature, stimulating increased contraction and stabilization of the shoulder during activities that potentially could subluxate the glenohumeral joint.
Many authors believe in the importance of distinguishing between patients with acute posterior dislocation versus those with recurrent posterior subluxation.4,30,39 Posterior instability can develop from several different entities: congenital laxity or hyperlaxity, chronic overuse, traumatic disclocation/subluxation, or a combination of all of these. Therefore, any previous injuries as well as athletic endeavors should be elicited. Traumatic instability develops from a fall or impact on a flexed, adducted, internally rotated arm. Atraumatic instability usually has a congenital component and is often associated with generalized ligamentous laxity. Recurrence following an acute dislocation is felt to be rare, and symptomatic instability seldom develops. This contrasts patients who develop insidious laxity, which predisposes to recurrent instability.
MULTIDIRECTIONAL INSTABILITY
The primary pathology of multidirectional instability appears to be hyperelasticity of the joint capsule, mainly secondary to dysfunction of the inferior glenohumeral ligament. This laxity can be acquired, congenital, or both. This laxity can progress due to a variety of causes, converting a functionally stable, lax shoulder into one with multidirectional instability.
Neer and Foster described three groups of patients with multidirectional instability. The first group included those with anterior inferior dislocation with posterior subluxation, the second had posterior and inferior dislocation with anterior subluxation, and the third had a recurrent dislocation in all directions.26
Additionally, there appear to be two separate populations that develop multidirectional instability. The first group includes those with congenital, generalized hyperelasticity, and the second group is composed of those who develop multidirectional instability due to repetitive activities. In all groups, elimination of the laxity of the capsule is necessary to achieve adequate stability.
HISTORY
A thorough and detailed history is essential in treating patients with shoulder instability. Classification of the instability as acute or chronic, traumatic or atraumatic, anterior, posterior, or multidirectional is of paramount importance. In addition, it is important to ascertain athletic participation because athletes involved in specific sports, namely weightlifting, swimming, throwing, and archery, are more likely to develop instability. Volitional instability must be identified early because these patients tend to do poorly with surgical repair. Volitional instability occurs in two groups. One group represents patients with good muscle control who can subluxate and relocate their shoulder from an early age, which may lead to capsular laxity and subluxation that begins to occur at inopportune times,
producing symptoms. The other group represents true voluntary dislocators with psychiatric problems; operative treatment for this population is rarely successful.
producing symptoms. The other group represents true voluntary dislocators with psychiatric problems; operative treatment for this population is rarely successful.
Patients with posterior instability usually present in their late teens or twenties. On initial presentation, patients will often complain of mild, unspecific shoulder pain with a feeling of looseness or instability in certain positions, mainly in the flexed, adducted, and internally rotated positions. Many patients associate the onset of symptoms to a specific event, and so a history of trauma with the arm in this position should raise suspicion for posterior shoulder pathology.
Hawkins et al. reported that nearly 40% of their patients with posterior instability reported no pain in the involved shoulder, even though they experienced daily episodes of subluxation.17 They reported that activities of daily living were unhindered in almost all patients, with most problems reported as sports related. In their study group they reported a low incidence of patients who had instability associated with a history of trauma, which has been contradicted by other studies.46
Most patients diagnosed with multidirectional instability present in their late teens or twenties. The presenting symptom is usually pain, most commonly occurring during activities of daily living with the glenohumeral joint in the midrange of function. Symptoms may also include a feeling of instability and transient neurologic symptoms.
Neer feels that patients with multidirectional instability possess two key clinical features. First, their symptoms of pain occur during the midrange of glenohumeral motion. Second, the physical examination shows the ability to subluxate, or dislocate, the joint anteriorly, inferiorly, and posteriorly with reproduction of symptoms in one or more of these directions.26
Often, patients with MDI present with an insidious onset of shoulder discomfort. There may be a history of injury, but the degree of trauma is often not considered significant enough to produce the patient’s symptoms. In both posterior and multidirectional instability, activity-related complaints are common and range in severity from frank dislocation to subtle episodes of painless instability. Often patients will report a constant dull ache between episodes of intense pain or instability. Intermittently, neurologic symptoms may be the patient’s presenting complaint, or it may not occur at all.
It is important to identify the frequency and severity of the symptoms, as well as the force involved in causing the discomfort. If the patient is experiencing multiple dislocations, the method of reduction and effort involved in reducing the shoulder is important to elicit. The position in space of the affected extremity when symptoms occur is also helpful to determine the predominant direction of instability, if one exists. If dislocations occur during sleep, this represents an end-stage disease process, and nonoperative treatment is likely to be ineffective.
PHYSICAL EXAMINATION
The physical shoulder examination for a patient suspected of having shoulder instability begins with inspection. The patient’s entire shoulder girdle, as well as the entire involved extremity, needs to be unclothed. Inspecting for muscle atrophy from the front and back is important. The deltoid of patients with MDI may have a squared-off appearance due to inferior subluxation of the humeral head. Scapulothoracic motion should be observed, looking for any excessive scapular protraction or dyskinesia, during both passive and active range of motion for the shoulder. The cervical spine’s range of motion needs to be evaluated to rule out referred pain and weakness patterns.
Many patients with MDI show signs of generalized ligamentous laxity, which include metacarpophalangeal hyperextension, genu recurvatum, patellar subluxation, elbow hyperextension, and the ability of the abducted thumb to reach the ipsilateral forearm. Generalized laxity has been reported to occur in 45% to 75% of patients undergoing surgery for MDI.9 It is important to identify patients with known connective tissue disorders, such as Marfan’s syndrome and Ehlers-Danlos syndrome. These patients tend to respond poorly to soft-tissue-only repairs and may need to undergo extensive preoperative testing to rule out any vascular or ocular abnormalities.
The exam begins with a thorough neuromuscular exam of the affected extremity, including range of motion, vascular integrity, and strength in all muscle groups, including scapulothoracic. A sensory exam is carried out in all dermatomes.
Palpation of the shoulder girdle follows. Bigliani et al. reported that two-thirds of the patients they treated with posterior instability had posterior glenohumeral joint-line tenderness, a finding not supported by other authors.5
Active and passive range of motion of the shoulder in all directions should be recorded. In assessing patients with posterior instability, a few provocative tests have been described. The first is the jerk test, where the affected arm is placed in forward flexion, adduction, and internal rotation. The examiner then stabilizes the scapula with one hand while providing a posterior and inferior directed force on the elbow. A positive test occurs when the humeral head is able to be subluxed over the posterior glenoid rim to a greater degree than the contralateral side (Fig. 3-5). Often this reproduces the patient’s symptoms. Shoulder abduction and external rotation tend to reduce the subluxed humeral head back into the concavity of the joint.
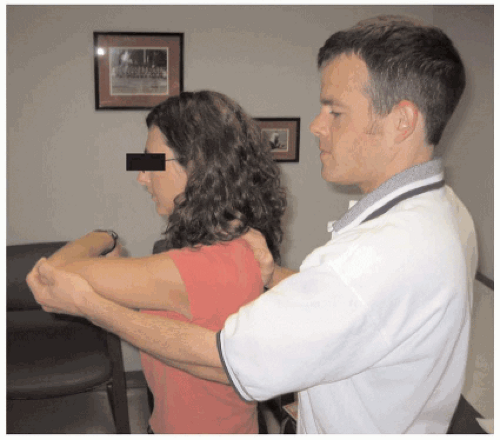
The load and shift test (described later in this chapter) should also be performed. A positive test occurs when the humeral head fails to relocate with the tightening of the posterior ligaments. Increased scapular winging with any provocative test indicates scapulothoracic dyskinesia and should be noted. The Whipple test is also performed, initially unsupported, and then repeated, with the scapula
supported (Fig. 3-6). A positive test for instability is indicated by painful buckling during the unsupported test and then decreased pain and increased strength when the scapula is stabilized.
supported (Fig. 3-6). A positive test for instability is indicated by painful buckling during the unsupported test and then decreased pain and increased strength when the scapula is stabilized.
The exam continues with an assessment of inferior laxity. With the arm by the patient’s side, the examiner places inferior traction on the humerus. A positive test occurs when the skin dimples just inferior to the acromion, and the inferior translation of the humerus is at least 2 to 3 cm. With the arm in adduction and neutral rotation, the superior glenohumeral ligament is the primary stabilizer to inferior translation. However, with the arm externally rotated, the rotator interval is the primary stabilizer; therefore, the test should be done in both positions.
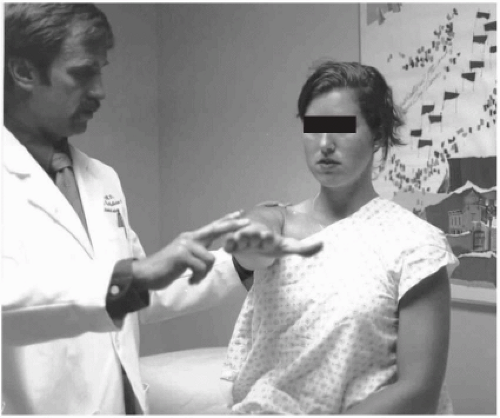 Figure 3-6 Whipple test. The examiner applies a downward force onto the hand with the shoulder flexed to 90 degrees and adducted. |
Testing for inferior laxity should also be performed in the 90-degree abducted position to test for laxity of the inferior capsule. An inferior translation force is applied to the superior proximal humerus in the abducted arm, with inferior subluxation greater than 1 cm considered abnormal.
The exam continues with the patient in the supine position on the exam table. The patient is asked to position the shoulder slightly off the edge of the table. The arm is then placed in 20 degrees of abduction in the plane of the scapula; the examiner then places one hand on the patient’s elbow and the other on the proximal humerus and applies a compressive load to the humerus. Anterior- and posterior-directed forces are then applied to the humerus, and the amount of subluxation of the humeral head in the fossa is recorded (Fig. 3-7). This should be done in varying degrees of abduction and external rotation to assess different degrees of tension in the capsular ligament. It is important to remember that up to 50% subluxation of the head in any direction is considered normal. The subluxation is graded according to the following classifications: (a) 1+ indicates that there is excessive translation compared to the contralateral shoulder; (b) 2+ indicates that the humeral head can be subluxated over the rim of the glenoid but spontaneously reduces when the examiner releases pressure; and (c) 3 + indicates frank dislocation of the humeral head over the rim of the glenoid without spontaneous reduction. If subluxation is present, it is important to note whether the patient has a predominant direction of subluxation, which can affect surgical treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree