Whether a patient with burn injury is an adult or child, contracture management should be the primary focus of burn rehabilitation throughout the continuum of care. Positioning and splinting are crucial components of a comprehensive burn rehabilitation program that emphasizes contracture prevention. The emphasis of these devices throughout the phases of rehabilitation fluctuates to meet the changing needs of patients with burn injury. Early, effective, and consistent use of positioning devices and splints is recommended for successful management of burn scar contracture.
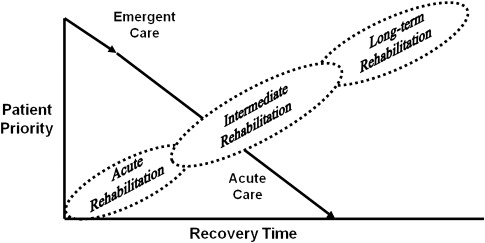
The development of burn scar contracture is a pathologic condition. Burn scar contracture is defined as a loss of motion of a joint or anatomic structure as a result of normal skin being replaced by inextensible scar tissue. The presence of a burn scar contracture has been shown to have a negative impact on a burn survivor’s quality of life, particularly in regards to physical functioning. A focus of burn rehabilitation should be to prevent or minimize contractures of the affected areas. Based on biomechanical considerations (discussed later), appropriate splinting and positioning is a critical component of any comprehensive burn rehabilitation program designed to attain optimal range-of-motion (ROM) outcomes. In 2008, a schema of burn rehabilitation phases (acute, intermediate, and long term) was developed to delineate the components of burn care treatment that are emphasized at different points in the continuum of care ( Fig. 1 ). Table 1 describes the primary goals for positioning and splinting of burn patients during each burn rehabilitation phase.
| Phase of Rehabilitation | Goal |
|---|---|
| Acute | Edema control and pressure relief |
| Intermediate | Tissue elongation and graft protection |
| Long term | Tissue elongation |
Biomechanics
Biologic tissue adapts to the mechanical influences of applied external forces. Placing stress on tissue can cause it to change shape or form. Excessive stress causes damage to the tissue while too little stress is insufficient to stimulate change beyond normal cellular turnover. When treating patients with burn injury, splinting or positioning interventions must strike a stress balance to be effective. Developing an understanding of the biomechanic principles that underlie these physical interventions in the management of burn scar contracture aids in improving burn rehabilitation practice, leading to improved patient outcomes.
Both skin and scar tissue are comprised of an extracellular matrix—a solid fibrous network with a viscous liquid component, herein referred to as ground substance. In natural skin, collagen and elastic fibers provide integrity and elasticity, respectively. These components interact to protectively limit extensibility and provide tissue recoil after elongation. In contrast, burn scar tissue is only composed of collagen fibers within an altered ground substance environment and elastic fibers are absent. The collagen fibers are arranged in no predictable pattern. The predominant subcomponent of ground substance is chondroitin sulfate A, a substance found in abundance in bone tissue. This biologic composition of burn scar tissue is thought to be a possible cause of the inextensibility seen in burn scar.
With joint movement, skin or scar needs to accommodate to a change in limb length. As limb length increases, collagen fibers unfurl and orient in the direction of force applied. As skin, more so than scar, is elongated further, additional collagen fibers sequentially align in the direction of the force applied. As collagen fibers move, the ground substance is displaced from between the fibrous network. When movement is reversed, the collagen fibers retract to their normal resting position while again having to redisplace the surrounding ground substance.
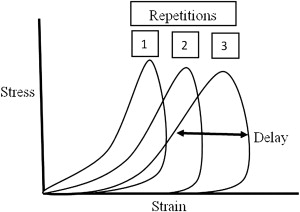
Successive length induction (SLI) or preconditioning of tissue, commonly referred to as stretching tissue, is an important concept to enlist whether fabricating a splint or setting up a positioning program for a patient. SLI entails repeatedly elongating a tissue until it reaches its safe maximal length ( Fig. 2 ). Maximal length of tissue has been reported to occur after 7 to 9 repetitions up to a tissue’s yield point ( Fig. 3 ). In a clinical situation, however, the yield point of tissue is rarely reached due to pain complaints in conscious patients. Safe, maximal preconditioning of tissue can be clinically determined when a patient’s ROM about a given joint ceases to increase with repeated repetitions. When preparing to fabricate or apply a splint, it is ideal to employ SLI until the tissue has achieved its maximal preconditioned length. At end range, this causes the tissue to be under tension. When tension is removed, tissue naturally retracts back to its desired resting length. Loading and unloading of tissue when plotted on a stress-strain curve produces a hysteresis type of pattern (see Fig. 2 ). With each successive lengthening, more and more ground substance is displaced from between the compacted fibers. The delay in tissue retraction is attributed to redistribution of the ground substance. It is important, however, to remember that all tissue wants to remain at its resting length. Much research is still needed in the area of biomechanics related to the burn injured population. Understanding basic biomechanical principles when applying rehabilitation techniques, however, helps burn therapists better understand the expected response to treatment.