Burns are ubiquitous injuries in modern society, with virtually all adults having sustained a burn at some point in their lives. The skin is the largest organ of the body, basically functioning to protect self from non-self. Burn injury to the skin is painful, resource-intensive, and often associated with scarring, contracture formation, and long-term disability. Larger burns are associated with morbidity and mortality disproportionate to their initial appearance. Electrical and chemical burns are less common injuries but are often associated with significant morbidity.
Burns are ubiquitous injuries in modern society, with virtually all adults having sustained a burn at some point in their lives. The skin is the largest organ of the body, basically functioning to protect self from non-self. Burn injury to the skin is painful, resource-intensive, and often associated with scarring, contracture formation, and long-term disability. Larger burns are associated with morbidity and mortality disproportionate to their initial appearance. Accurate assessment of the burn patient and appropriate institution of early care are critical to optimal outcomes. Initial evaluation uses the “ABC” precepts of the Advanced Trauma Life Support (ATLS) course: airway, breathing, and circulation. Additional burn-specific care is noted in the Advanced Burn Life Support (ABLS) course.
Nearly all burns are completely preventable, requiring conscious thought to occur. Approximately one-third of patients admitted to burn centers are children. Most pediatric injuries are scald burns and are related to cooking, with hot beverages, soups, and microwaved foods frequent offenders. Keeping children out of the kitchen during cooking would minimize these burns. Tap water burns in both young and elderly individuals are caused by the temperature of the water heater being set too high (>120°F), and can be completely avoided by simply resetting the water heater’s thermostat. Inappropriate use of highly flammable liquids, such as gasoline and lighter fluid, is a significant cause of burn injury in adults. Smoking, intoxication, suicide attempts, and assaults provide continuing sources of burn injury. Electrical and chemical burns are primarily adult injuries.
Determinants of severity
Although burn size and depth are obvious factors in determining burn severity, the location (body part) of the burn, age of the patient, preexisting disease, and presence of trauma, including an inhalation injury, may complicate treatment.
Burns to the head and neck, hands, feet, and perineum and genitalia confer significant morbidity and mortality to the injury disproportionate to burn size. The airway originates and passes through the head and neck, requiring continual vigilance and need for airway protection, in addition to the obvious changes in appearance engendered by these burns. Hand burns require significant available skin grafts, operating time, and therapy resources disproportionate to their relatively small size. Because of the proximity of tendons and joints to the skin surface, injury is common in these structures, which are critical for normal function. Foot burns render patients immobile, and grafts in these areas are at risk for wear and tear from footwear. The perineum and genitalia are areas that are at risk for infection during burn treatment, and are also nearly impossible to immobilize for adequate graft take.
Patients younger than 2 years or older than 50 years are at higher risk of complications and death than the remaining population. In babies, thin skin, limited reserves, and high surface area–to–mass ratios contribute to this risk, whereas thinning skin and medical problems commonly associated with aging are major factors in older individuals. Young children are also at risk for burns caused by abuse. These injuries are most often scald burns from tap water, and are deeper than those seen in the general pediatric burn population and commonly involve the lower extremities, buttocks, and genitalia. Bathroom training and soiling are frequently involved as precipitating factors. Fortunately, these burns often have characteristic patterns of injury, aiding in appropriate diagnosis.
Burns are not evenly distributed throughout the general population. Groups with higher-than-expected frequency of injury include the ill and disabled. These especially include the neurologically impaired, at risk for both occurrence and extreme depth. Seizures, paraplegia, and quadriplegia place these patients at special danger for both contact and scald burns. Diabetes mellitus, which makes medical care more difficult because of glycemic control, is also a risk factor for burn injury. Neuropathic pain relief through hot soaks or neuropathy insensate to heat cause patients to sustain burns from soaking or from walking on hot surfaces with inadequate foot protection. Associated chronic obstructive pulmonary disease and cardiovascular disease adversely affect outcomes. Smoking while on medically prescribed home oxygen creates a unique flash burn with minimal deep injury.
Traumatic injuries occur in addition to the burn in 5% to 15% of admitted patients. The most common causes are motor vehicle accidents, explosions, and falls sustained while escaping from the burn site. Evaluation and treatment of traumatic injuries takes precedence over treatment of the burn, with the caveat that maintenance of body temperature, airway protection, and appropriate burn fluid resuscitation must be achieved.
Burn Depth
Burn depth is a product of temperature, duration of exposure, and skin thickness, with depth being described in degrees based on its relationship to total skin thickness. Most burns have areas that are of mixed depth, with deeper burns often occurring in areas of thinner skin thickness.
First-degree burns involve only the epidermis or topmost layer of skin. They are recognized by their erythematous appearance and lack of blisters or skin separation. When rubbed with the gloved finger, the burn tissue does not separate from the underlying dermis (ie, negative Nikolsky’s sign). Although more commonly used for dermatologic diseases, Nikolsky’s sign is also a reliable differentiator of first-degree burns from deeper ones that have not had time to blister. The classic first-degree injury is the sunburn or superficial scald burn from spills. These burns have no morbidity other than pain, and are therefore not calculated into burn size. Treatment includes oral pain medications, cool water compresses for the first day, and then application of any bland emollient to remoisturize the skin, such as aloe vera, cocoa butter, Eucerin cream, vitamin D, vitamin E, Aveeno, Lubriderm, and even Udder Butter, Bag Balm, or lard. Thicker ointments and those that are not quickly absorbed into the skin generally maintain lubrication for longer periods. Antimicrobial ointments need not be used on these burns.
Second-degree burns are synonymous with partial-thickness burns (those that burn only part way through the dermis). Epithelial elements remain in the undestroyed dermal appendages and spontaneous healing occurs in 7 to 28 days. Second-degree burns are very painful and are usually blistered. The blister fluid is clear and the underlying skin is wet and pink. The most common causes are spill scalds and flash burns. Treatment of these burns is protection with a biologic dressing. Deep partial-thickness burns are those that take more than 3 weeks to heal and have the potential to scar worse than grafted third-degree burns. If the patient’s condition permits, these deeper burns are best treated with excision and skin grafting. When depth is uncertain or the burn is of mixed depth, these injuries are treated as third-degree burns, because biologic dressings generally do not adhere to these deeper wounds and provide little to no microbial control when not adherent.
Third-degree or full-thickness burns are those that extend through the dermis, destroying all epidermal and dermal elements. They require skin grafting for wound closure. When debrided, these burns appear deep red or white in color and are relatively insensate, although presence or absence of pain is an unreliable indicator of depth. They may initially have blisters containing hemorrhagic fluid. The resultant dead tissue is called eschar and must be removed before skin grafting. The prototype of these burns is the flame burn. Treatment is with topical antimicrobials and surgery.
Fourth-degree burns (deep burn necrosis) are those that extend into deep soft tissue, muscle, or bone such that closure with simple skin grafts is usually not possible. Electrical burns and deep thermal burns of the hands, anterior lower legs, and feet predominate (body parts where vital structures are very close to the skin surface). These burns often require surgical flap closure (free or pedicled) or extremity amputation.
Burn Size
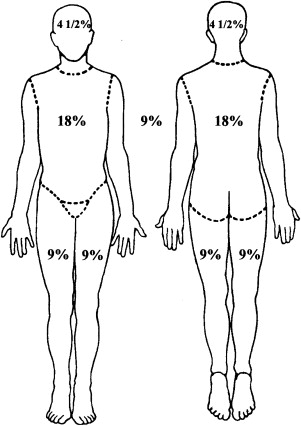
Accurate initial assessment of burn size is essential for optimal patient care. Burn size is expressed as total body surface area (TBSA) or body surface area (BSA), wherein approximately 1% of a patient’s surface area is equal to that of the palmar surface of the patient’s hand with the fingers closed. This measurement is most useful for small (<5% TBSA) or spotty burns. For larger areas, the rule of nines ( Fig. 1 ) provides a simple and rapid estimation of burn size in the adult. When calculating burn size using any method, first-degree burns are not counted and only the proportion of area actually burned is calculated. Thus, for an upper extremity to be considered 9% TBSA, the entire extremity from the shoulder to the finger tips must be burned at least to the blistering level. If only the posterior half of the upper extremity is burned, then burn size is considered to be 4.5% TBSA.
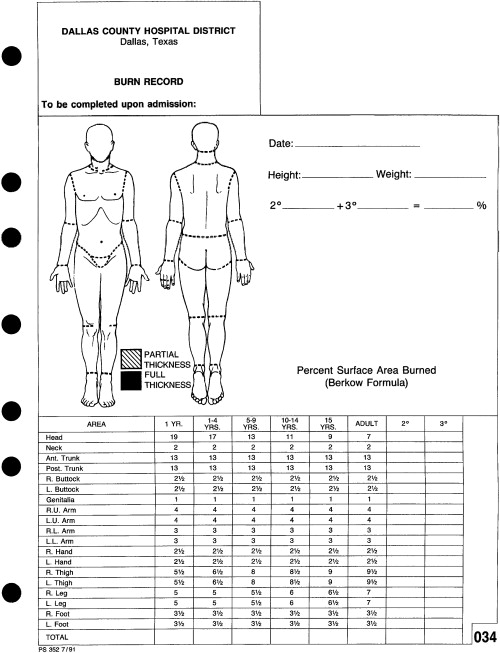
More accurate evaluation of burn size is made with a Berkow ( Fig. 2 ) or Lund Browder chart, which identifies the different body proportions according to age of the patient (with children having larger heads and smaller lower extremities than adults) and through dividing the body into smaller units, such as dividing the upper extremity into the upper arm, lower arm, and hand (see Fig. 2 ). More recently, the use of computerized drawings simplifies calculations of size in both pediatric and adult patients and will even estimate fluid requirements. A version is also available for hand-held devices.
Resuscitation
Fluid resuscitation is the cornerstone of early burn care. The microvascular structure beneath a burn wound develops increased permeability immediately after injury, which lasts through the first day post-burn. This capillary leak is up to molecular weight (MW) 30,000 d, effectively making the body two and a half fluid compartments instead of the normal three. The intravascular and extravascular extracellular compartments become one, except for the larger globulins and formed elements of the blood, which remain intravascular. This capillary leak is roughly directly proportional to burn size and becomes hemodynamically significant in burns larger than 20% TBSA (10% TBSA in young children or elderly patients). The objective of resuscitation is to replace this lost intravascular fluid with the minimal amount of fluid required to maintain normal bodily function.
Various formulas have been proposed to replace these fluids, which are either third spaced or completely lost into the burn dressing. These formulas replace 0.7 to 0.8 mEq of sodium per kilogram per percent burn in the first 24 hours, given at various rates and concentrations. The most commonly used formula is the Parkland formula, which suggests 4 mL of Ringer’s lactate per kilogram of body weight per percent BSA burned during the first 24 hours post-burn. Using Ringer’s lactate, electrolyte concentration is not a problem during resuscitation and values are not even measured. Underresuscitation is met with renal failure, hypotension, and multiple organ dysfunction, whereas overresuscitation results in pulmonary and cardiac overload and excessive edema formation. The extremes of age are especially sensitive to misestimation of fluid needs. Resuscitation requires an accurate estimation of the time of burn, burn size, and measurement of patient weight. Factors that increase fluid requirements include inhalation injury, late initiation of resuscitation, deep burns, acute intoxication, and preexisting malnutrition. All burn formulas are only starting points in resuscitation. Individual changes to fluid administration rates must be made hourly (or half-hourly in infants and small children) based on urine output and vital signs. Use of invasive vascular monitoring is seldom necessary. Non-burn fluid maintenance in children is added into the burn resuscitation as necessary, with maintenance in small children given as 5% dextrose/Ringer’s lactate solution. Hypertonic resuscitation and timing for administration of colloids continue to be areas of research interest. All of the burn resuscitation formulas work well in experienced hands. The best formula is the one used by the burn center to which the patient is being transferred.
Inhalation Injury
Inhalation injury may be classified in several different ways, the simplest of which is division into carbon monoxide poisoning and upper and lower airway injuries.
Carbon monoxide is an odorless, tasteless gas that is very slightly lighter than air. It is produced by the incomplete combustion of carbon containing materials and causes more deaths in the United States than all other poisons. It binds with hemoglobin in the red blood cell, forming carboxyhemoglobin (COHb), which has 210 times the bond for oxygen as normal hemoglobin, shifting the hemoglobin/oxygen dissociation curve to the left. In burn patients, the sometimes-subtle signs of cherry red lips or mucosa and symptoms of nausea and headache are absent, and therefore COHb levels should be measured in all patients who were trapped in a smoke-filled space. Optimal treatment is with 100% oxygen, which decreases the half-life of COHb from 4 hours to approximately 40 minutes. In the presence of elevated P ao 2 of COHb, measured and cutaneous saturations are meaningless. COHb levels do not correlate with patient outcomes.
Upper airway injury is a misnomer, and is really the result of swelling problems caused by external burns. These conditions do not necessarily imply pulmonary injury, because they also occur with scald burns. Edema formation in the posterior pharynx and glottic and subgottic areas associated with deep burns of the upper chest, neck, and lower face has the potential to catastrophically occlude the upper airway, most often at the level of the vocal cords in adults. Elevation of the head of the patient’s bed helps minimize swelling until the airway is controlled. Upper airway stridor and increased work of breathing are very late signs of impending airway obstruction. Protection is accomplished through endotracheal intubation, with the tube carefully secured in place to avoid dislodgement once successfully placed. The endotracheal tube is left in position until swelling decreases to the point at which an airleak occurs when the tube cuff is deflated.
Lower airway or true smoke inhalation injury is caused by the patient inhaling the products of combustion, often as a result of being trapped in a closed space. Carbonaceous material is commonly suctioned from the airway. Fiberoptic bronchoscopy is the preferred diagnostic procedure. Early grading of inhalation injury severity is very inaccurate. The injury is basically a chemical burn from which resulting edema of the small airways creates distal microatelectasis and a clinical picture identical to acute respiratory distress syndrome (and with the same definition). Significant injuries are those necessitating endotracheal intubation and mechanical ventilation for more than 4 days. Inhalation injury increases mortality for any given size burn and patient age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







