Ponseti Casting
Blaise Nemeth
Kenneth J. Noonan
DEFINITION
Clubfoot, also known as congenital talipes equinovarus, occurs in approximately 1 in 1000 live births.
The clubfoot contains four identifiable components that are easily remembered using the acronym CAVE (cavus, adductus, varus, and equinus). Idiopathic clubfoot contains each of the four components to varying degrees.
The so-called postural clubfoot is held by the infant in an equinovarus position, but all components are nearly completely correctable with gentle manipulation and resolve over time without intervention.
A small proportion of clubfeet are teratologic, occurring as part of other neuromuscular diseases, such as Larsen syndrome, any of the arthrogryposis syndromes, and spina bifida.
The complex clubfoot, a severe type of idiopathic clubfoot, has a tighter hindfoot and plantar structures.
In 1948, Dr. Ignacio Ponseti began manipulating clubfeet through serial casting, completely correcting the clubfoot deformity. The principles of Ponseti casting lay in gently stretching the soft tissue structures and gradually inducing remolding of the primarily cartilaginous bones of the hindfoot during immobilization.
For the definitive publication on clubfoot and the Ponseti technique, the reader is referred to Dr. Ponseti’s book.7
The success of the treatment protocol that bears his name has been borne out through over 30 years of follow-up, establishing it as the standard for initial treatment of clubfoot.1
In 2006, Dr. Ponseti published a modification to his original casting technique that addresses the specific deformities characteristic of the complex clubfoot.8
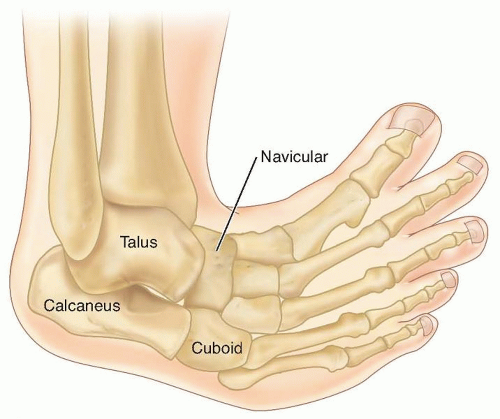
ANATOMY
The Achilles and posterior tibialis tendons, as well as the posterior and medial ligaments of the foot between the calcaneus, talus, and navicular, are thickened and fibrotic.7
The clubfoot contains a number of changes in bony alignment and shape (FIG 1).
Relative to normal foot anatomy, the first ray is plantarflexed, generating the cavus deformity. By comparison, all rays are plantarflexed in the complex clubfoot, resulting in full-foot cavus.
The navicular is medially displaced on the talus, and the cuboid is medially displaced on the calcaneus as part of the adductus deformity. The medial corners of the head of the talus and the anterior calcaneus are flattened.
The calcaneus is inverted under the talus, creating the hindfoot varus, while also being in equinus and elevated in the fat pad of the heel.
In children with unilateral clubfoot, the affected foot usually is smaller, as is the lower leg, relative to the unaffected side.
Up to 85% of clubfeet have an insufficient or absent anterior tibial artery.6
NATURAL HISTORY
The exact cause of the fibrotic changes in clubfoot is unknown. Recently, candidate genes have been identified in familial clubfoot, including Pitx1 and Tbx4.3
Left uncorrected the weight-bearing surface in a clubfoot becomes the dorsolateral surface.
Thick callosities develop, and the positioning of the foot creates significant functional disability.
PATIENT HISTORY AND PHYSICAL FINDINGS
Clubfoot may be identified on prenatal ultrasound as early as 12 to 13 weeks (FIG 2).
Half or more of fetuses with clubfeet identified on second trimester ultrasounds are found to have other anomalies (most commonly cardiac, neurologic, and/or urogenital) or are syndromic/teratologic.9
The exact sensitivity and specificity of prenatal ultrasound are unknown. False positives are rare on 20-week ultrasounds but may be as high as 40% during the third trimester (when false negatives are rare).9 Cases not found on prenatal ultrasound are readily identifiable at birth.
All children with clubfeet should be examined for other findings that may suggest a syndromic or neuromuscular association, such as other contractures or joint dislocations (especially hip dislocation), cutaneous lesions, spinal abnormalities, and abnormal facial features.
The clubfoot is easily identified by the combined deformities of cavus, adductus, varus, and equinus.
Consider complex clubfoot if a deep midfoot crease and cavus extend transversely across the entire plantar aspect of the foot, and the foot appears short and broad.
The ability to abduct or dorsiflex the foot completely on examination suggests etiologies other than idiopathic clubfoot, such as isolated metatarsus adductus, neuromuscular disease, or focal anatomic abnormalities.
The fat pad of the heel will feel empty upon palpation due to equinus positioning of the calcaneus. This is especially dramatic in the complex clubfoot.
The lateral head of the talus is easily palpable over the dorsolateral surface of the foot. More laterally, the anterior calcaneal tuberosity is also palpable. Care must be taken in differentiating these two structures because Ponseti casting necessitates stabilizing the foot over the lateral head of the talus, allowing free motion of the calcaneus under the talus, whereas pressure at the calcaneal tuberosity blocks calcaneal rotation, allowing only forefoot abduction.
The complex clubfoot has a crease that extends transversely across almost the entire plantar aspect of the foot accompanied by full-foot cavus with plantarflexion of all metatarsals. Also, the heel crease is deeper than that of most other clubfeet. During the initial one or two casts, as the adductus is corrected, the first ray in the complex clubfoot becomes retracted, if not noticeably retracted at presentation. The cavus also persists, with all metatarsals remaining plantarflexed.
It is important to examine the clubfoot before each casting to evaluate for the adjustments that must be made during casting to correct residual deformities or to identify and modify casting for a complex clubfoot.
A number of classification systems have been introduced as an attempt to predict outcome, but the ability of these systems to evaluate correction, predict recurrence and final function is still unclear.5
The degree of dorsiflexion and abduction, and the distance of the navicular anterior to the medial malleolus, provide other objective measurements of deformity and correction.
Some children are born with one or both feet held in an equinovarus deformity at birth that is nearly completely correctable on examination. Nearly complete dorsiflexion (more than 20 degrees) is present, although abduction may be slightly limited. The calcaneus is also readily palpable in the fat pad of the heel. These feet may be thought of as “postural” in nature, and most will resolve spontaneously or with parental stretching over 1 to 2 months.
If persistent, one or two casts usually correct the deformity, and Achilles tenotomy is rarely required. Feet corrected with casting may require maintenance in a foot abduction orthosis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Clinical examination is sufficient to diagnose the congenital clubfoot.
Plain radiographs at birth are not helpful in diagnosing clubfoot because the ossific nuclei of the talus and calcaneus are spherical, so orientation and relationship are not discernible, and the other tarsal bones are unossified.
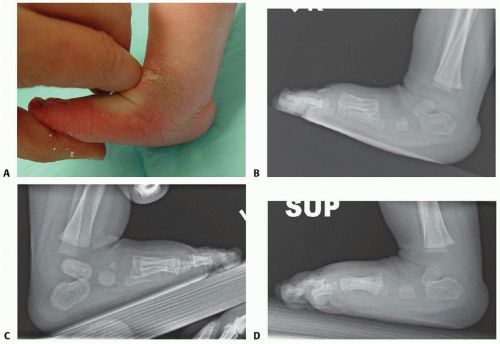
Once full abduction is obtained by casting, if dorsiflexion of more than 10 degrees is present, forced dorsiflexion lateral films are helpful in differentiating midfoot breach, producing apparent dorsiflexion, from true dorsiflexion occurring at the ankle, obviating the need for a percutaneous Achilles tenotomy (FIG 3).
DIFFERENTIAL DIAGNOSIS
Metatarsus adductus
Neurologic equinovarus or cavovarus deformity
Both deformities may be differentiated from clubfoot by absence of the other components of clubfoot.
Teratologic or syndromic clubfeet (including neuromuscular disorders)
Clubfoot deformity may be more difficult to correct and tends to recur.
Postural clubfoot
Complex clubfoot
NONOPERATIVE MANAGEMENT
Ponseti casting of the idiopathic clubfoot involves a specific sequence of corrective maneuvers that correct the deformities of the clubfoot in combination.
Each manipulation is maintained with a plaster cast.
Ponseti casting ideally begins during infancy, although good results are achievable through toddlerhood. Casting in older children can also produce good results or at least reduce the amount of surgery required for complete correction.
An open tendo Achilles lengthening may be more appropriate than a percutaneous tenotomy in children older than 2 years old.
Long-leg casts should always be used to prevent cast slippage and maintain rotational control of the lower leg.
Initially, applying a short-leg cast allows focused attention on maintaining foot position and molding before extending the cast above the knee.
Padding should be minimal, and plaster is preferable for its ability to be molded precisely to the contours of the foot and ankle.
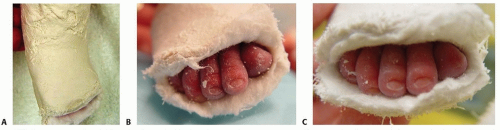
Four to six casts should correct the cavus, adductus, and varus deformities. If correction is not achieved in eight casts or the child pulls back in the casts (FIG 4A), the possibility of an unrecognized complex clubfoot or improper casting technique should be considered.
Casting is facilitated by the child being relaxed and calm. Feeding the infant during casting assists in this.
For breast-fed infants, it is helpful if the family introduces, and uses once daily, a bottle so the child may feed during casting. If a bottle is not tolerated, other calming measures may be necessary.
For older children, music, television, or playing with toys often proves helpful, as does casting with the child sitting upright or on the parent’s lap.
Before leaving the clinic, the toes should be checked to make sure they are pink and well perfused.
Some toes will become reddish-purple as the casts cool (appearing much like the acrocyanosis present at birth) but will become pink if the child is bundled and monitored over 1 hour or so (FIG 4B,C).
Toes that become more purple and dusky indicate that the cast is too tight and should be reapplied.
Casts are changed every 5 to 7 days. The final cast, following percutaneous Achilles tenotomy, is left in place for 3 weeks.
Almost all clubfeet will require a percutaneous Achilles tenotomy to correct the residual equinus deformity once the other components are corrected.
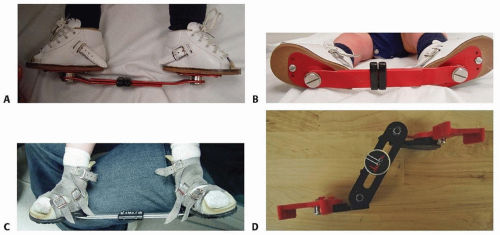
Once complete correction is obtained, correction must be maintained by placing the feet in a foot abduction orthosis (FIG 5A-D).
Constructs include straight last shoes, soft ankle-foot orthoses (AFO), or rigid AFOs mounted on rigid or articulating bars (see Postoperative Care).
SURGICAL MANAGEMENT
Percutaneous Achilles tenotomy is required in almost all idiopathic clubfeet to correct the residual equinus.
About 20% of patients require anterior tibialis tendon transfer at 3 to 4 years old to correct recurrent or persistent dynamic varus deformity (see Chap. 116).
Preoperative Planning
Degree of dorsiflexion
If dorsiflexion is less than 10 degrees, a percutaneous Achilles tenotomy is required to correct the residual equinus.
If dorsiflexion is more than 10 degrees, forced dorsiflexion lateral foot radiographs help to differentiate midfoot dorsiflexion, with residual calcaneal equinus, from true dorsiflexion occurring at the hindfoot (see FIG 3).
Location
The risk of anesthesia must be balanced against the perceived pain and duration of the procedure as well as the degree of sedation necessary for safe performance of the procedure and optimizing posttenotomy casting. Approximately half of pediatric orthopedists report performing the percutaneous tenotomy under general anesthesia or conscious sedation.10
Local analgesia, with 1% lidocaine, affords the opportunity to perform the tenotomy in the clinic setting and avoids any potential risk of general anesthesia.
Positioning
The child should be supine on the table with the contralateral leg held out of the way by the parent or an assistant during tenotomy and casting.
Approach
A medial approach is used to remain posterior to medial neurovascular bundle.
TECHNIQUES
▪ Casting
Stretching
Before casting, the foot should be stretched in the same manner as used for immobilization during casting (TECH FIG 1A,B).
The thumb of the examiner’s contralateral hand (eg, the left hand when manipulating the right foot) should be placed over the head of the talus, and the index finger of the other hand should lie along the medial aspect of the first ray with the second through fourth fingers under the plantar aspects of the forefoot.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree