Plantar Interdigital Neuroma Resection: Primary and Revision
Harold B. Kitaoka
Numerous disorders can cause central forefoot pain such as a plantar interdigital neuroma (Fig. 12.1). It usually affects the third webspace region and is more common in females who are in their middle-age years (1,2). The cause is unclear. Some believe there is an anatomic predisposition such as a communicating branch to the third interdigital nerve from the fourth, which could cause a tethering effect on the nerve, to the extent that it is more sensitive to irritation from the transverse metatarsal ligament. Others believe it is due to nerve compression from the intermetatarsal bursa, or nerve compression from the superficial and deep intermetatarsal ligaments, or a vascular disorder causing neurofibrosis.
Patients complain of burning pain or aching in the region of the second, third, and fourth metatarsophalangeal (MTP) joints plantarward. Patients can sometimes point to a specific webspace where the pain is most intense, and at other times, it is a more ill-defined, diffuse aching. The pain can extend into the toes. Patients may complain of numbness and/or paresthesias extending into the lesser toes. It is often more bothersome with footwear. The pain is relieved by rest, removing the shoe, and rubbing the foot; but absence of this historical description does not exclude interdigital neuroma. There may be vague, slowly progressive forefoot pain that persists for months to years. Pain may be localized to a specific webspace, but patients may have difficulty in localizing the pain and may describe it by pointing to the entire forefoot. Sometimes, the only area where the patient perceives pain is in a toe adjacent to the involved webspace. Other complaints are the sensation of a mass under the forefoot, described as a pebble in the shoe. It may cause splaying between two of the lesser toes: a nonspecific sign, because there are other causes of splayed toes, such as MTP synovitis. Patients may have a forefoot avoidance gait and walk on the lateral border of the foot.
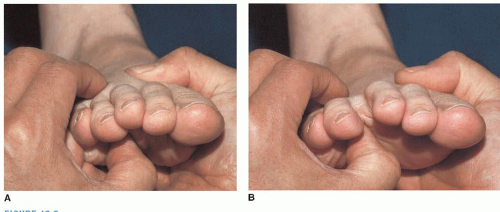
The various disorders that cause forefoot pain can often be differentiated by examination. It is sometimes difficult to determine a specific diagnosis when the patient is not having severe symptoms at the time of the examination, and one should try to recreate the pain during examination. Examination should include range of motion of the MTP joints, stability testing of the MTP joints with a Lachman-type test, palpation of the metatarsal heads, tenderness of metatarsals dorsally, tenderness of an MTP joint dorsally, and tenderness of the webspace. Swelling, erythema, toe deformities, and plantar keratoses should be noted. A Mulder’s click is a provocative test that is useful in supporting the diagnosis. It is performed by pressing the thumb of one hand from plantar to dorsal, distal to the metatarsal heads, The forefoot is compressed with the opposite hand, resulting in a palpable and even audible click as the mass is forced plantarward (Fig. 12.2) with reproduction of pain and sometimes paresthesias extending into the two adjacent toes. The presence of the click in association with re-creation of the patient’s symptoms supports the diagnosis,
but when it is not present, a diagnosis of interdigital neuroma is not excluded. A nonpainful click can be observed in asymptomatic feet. Examination on more than one occasion can help ensure accurate localization of the pain. Sensory and motor function testing should be performed.
but when it is not present, a diagnosis of interdigital neuroma is not excluded. A nonpainful click can be observed in asymptomatic feet. Examination on more than one occasion can help ensure accurate localization of the pain. Sensory and motor function testing should be performed.
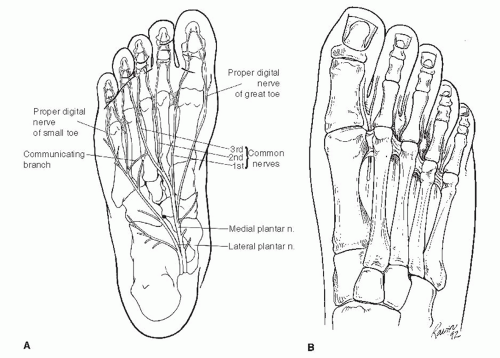 FIGURE 12.1 A: Central forefoot anatomy. B: Anteroposterior view of the foot shows a neuroma in the second webspace and its location relative to the intermetatarsal ligaments. |
Occasionally, patients have hypesthesia in the distribution of the affected common digital nerve. Percussion in the region of the common digital nerve usually does not cause paresthesias, but it is useful in other areas such as the posterior tibial nerve when other diagnoses are being considered, such as tarsal tunnel syndrome.
The diagnosis is based primarily upon clinical assessment with imaging studies used to exclude other disorders. Standing anteroposterior, lateral, and oblique radiographs of the foot detect any bony pathology. Rarely, other studies are helpful, if there is a question of the diagnosis such as a technetium bone scan to exclude occult bony processes that may be suspected, such as early Freiberg infraction or stress fracture. Special imaging such as magnetic resonance imaging (MRI) and ultrasound are usually not required. Signal abnormalities are often interpreted as Morton neuroma in feet that are asymptomatic (3). Electromyographic nerve conduction studies may be helpful in ruling out other neurologic causes of the forefoot pain, but they are rarely indicated for establishing a diagnosis of neuroma.
Other sources of forefoot pain can be misdiagnosed as an interdigital neuroma, including MTP synovitis, rheumatoid arthritis, synovial cyst, local infection, metatarsalgia, plantar keratosis, lesser metatarsal stress fracture, and Freiberg disease. More proximal neurologic problems such as lumbar radiculopathy or tarsal tunnel syndrome can occur. Nerve tumors such as neurilemmoma and neurofibroma may occasionally occur in the forefoot. It is not unusual for patients to have forefoot pain from more than one source. Symptoms related to other problems such as MTP synovitis or metatarsalgia should be treated before considering operative treatment. In some instances, it is possible to avoid surgery if appropriate treatment of the other disorder is initiated and the patient experiences enough relief. The history and physical examination are the most helpful tools in distinguishing between the various sources of pain before and after primary interdigital neuroma excision.
Recurrent pain after neuroma resection is occasionally due to recurrent neuroma. In addition to the webspace pain and burning that radiates into the adjacent toes, there is often hypersensitivity to the plantar skin in the metatarsal head region. Even light touch or stroking of the plantar skin in this area causes discomfort. Recurrence needs to be distinguished from other problems such as peripheral neuropathy or reflex sympathetic dystrophy. There may be exquisite tenderness that is greater than the webspace tenderness present preoperatively. If the persistent pain is localized to another interspace in the same foot and the symptoms are still characteristic of a primary neuroma, the wrong webspace may have been operated on or very rarely a second neuroma in the same foot may be present. Thompson and Deland (4) reported that a second neuroma in the same foot was a rare entity, occurring in only 3 (3%) of 89 patients studied. However, they also reported that 2 (40%) of the 5 failed neuroma resections were caused by the initial surgery having been done on the wrong interspace. Hypersensitivity of the dorsal scar occasionally results from an incisional neuroma of a cutaneous branch of the superficial peroneal nerve supplying the dorsal webspace and may have no relation to a recurrence of the interdigital neuroma. If dorsal hypersensitivity and pain is the major symptom causing dissatisfaction after primary neuroma excision, webspace reexploration would not provide relief, and treatment of the incisional neuroma might be indicated. Prior to embarking upon a revision operation in a dissatisfied patient, it may be necessary to obtain other diagnostic tests to rule out other causes of persistent pain if the history and physical examination findings are not characteristic for a recurrent neuroma. A bone scan is helpful to rule out an occult bone or joint abnormality in the foot, and an MRI scan may be necessary to rule out a space-occupying lesion. However, an MRI scan is not very helpful in determining whether a recurrent neuroma is present in the area of the previous surgery because of the difficulty in distinguishing neuroma from scar tissue. An MRI scan using a small forefoot surface coil might detect a signal abnormality at an adjacent webspace, but correlation with clinical symptoms is needed to make a diagnosis of a neuroma.
Treatment includes nonoperative measures for a Morton neuroma such as footwear modification: wide, soft-soled shoes, metatarsal pads, and prefabricated or custom orthotics. Injection of corticosteroid and local anesthetic can be useful for treatment and for providing support for the diagnosis of interdigital neuroma from dorsal-distal to plantar-proximal directions, starting in the webspace, using bupivacaine and cortisone. If the symptoms are not relieved by injection, excising the affected nerve has less predictable results, or the needle placement was not accurate. Flooding the central forefoot with a local anesthetic in one or more webspaces will relieve pain due to a variety of causes and is not diagnostic. Most patients experience initial pain relief from the injection but symptoms recur to the extent that one half eventually undergo third webspace neuroma resection (5) and symptoms often persist in the remaining patients who do not have surgery; but not to the extent that surgery is required. Injection cannot be recommended as a cure for plantar interdigital neuroma, but it can be offered as a temporizing measure or in patients who are not ideal candidates for surgery because of local or general medical conditions. Rarely, problems such as fat pad atrophy or varus/valgus toe deviation may result from an injection.
Despite these measures, it has been estimated that about one half of patients who have corticosteroid injection ultimately require excision of the interdigital neuroma as the definitive treatment. Resection is standard operative treatment. Neurolysis may be performed with results similar to resection, with 72% to 92% success (6,7). An advantage to the latter procedure is the elimination of the stump neuroma and preservation of sensation.
INDICATIONS AND CONTRAINDICATIONS
The indication for resection of an interdigital neuroma is forefoot pain and impairment recalcitrant to nonoperative measures.
The pain is usually localized to the third webspace, representing over 95% of interdigital neuromas.
The second webspace accounts for the other 5%, not in the first or fourth webspace.
Contraindications are patients with diffuse forefoot pain or symptoms in a webspace other than the third or second. When considering a diagnosis of second webspace neuroma, other causes must also be evaluated.
Indication for reoperation of an interdigital neuroma is after failed primary resection, and absence of other sources of central forefoot disorders.
Contraindications to reoperation for persistent pain after a primary interdigital neuroma excision include peripheral vascular disease, peripheral neuropathy, pain not characteristic of a recurrent neuroma of the interdigital nerve such as pain at multiple areas, inconsistent physical findings, reflex sympathetic dystrophy, unrealistic patient expectations, or diffuse peripheral neuritis.
Dorsal forefoot pain and hypersensitivity due to an incisional neuroma of the dorsal sensory branches of the superficial peroneal nerve will not respond to reexploration of the interdigital nerve for a neuroma. An incisional neuroma may respond to nerve exploration with neurolysis or neurectomy if initial nonsurgical treatment fails.
The patient with a multiply operated neuroma may have little to gain by further nerve exploration unless there is a likelihood that an incompletely resected neuroma is the cause of the continued pain and nonsurgical treatments are indicated. In recalcitrant cases, an implantable tibial nerve stimulator or spinal cord stimulator may provide significant relief from pain (6).
PREOPERATIVE PLANNING
The diagnosis must be correct.
The patient should be advised as to the probability that symptoms due to concomitant etiologies will likely persist even after successful neuroma surgery, such as metatarsalgia.
Patients with diagnosis of second webspace neuroma, neuromas in multiple webspaces, or previously failed operations should be reexamined to confirm the diagnosis.
Patients should be advised that a small patch of hypesthesia will result from surgery on the plantar aspect of the toes adjacent to the affected webspace.
SURGICAL TECHNIQUES
Technique 1: Primary Neuroma Resection
The patient is placed in the supine position, facilitating the dorsal approach.
A 4-inch Esmarch rubber bandage is wrapped around the foot and ankle for exsanguination, and released over the foot.
Local anesthesia is usually performed in the forefoot, proximal to the affected webspace, and light sedation.
A dorsal longitudinal incision is started in the appropriate webspace between the toes and extended proximally 2 to 3 cm to about the level of the metatarsal heads (Fig. 12.3). It is important not to follow the extensor tendons, but to keep the incision between the metatarsals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree