Chapter 8 Physical therapies
Treatment options in rheumatology
KEY POINTS
 Physical therapies aim to control pain, minimise joint stiffness and limit joint damage with the least adverse treatment effects
Physical therapies aim to control pain, minimise joint stiffness and limit joint damage with the least adverse treatment effects There is some evidence that TENS, thermotherapy and acupuncture can relieve pain in some rheumatic conditions but insufficient evidence for the efficacy of many electrotherapy interventions and manual therapy
There is some evidence that TENS, thermotherapy and acupuncture can relieve pain in some rheumatic conditions but insufficient evidence for the efficacy of many electrotherapy interventions and manual therapyTHE AIMS OF PHYSICAL THERAPIES IN RHEUMATIC DISEASES
It is important our assessment and management of patients with rheumatic disease is holistic. This means therapists should consider the person with the rheumatic condition rather than the structure (e.g. synovial joint) or the pathological process (e.g. rheumatoid arthritis) prior to selecting any therapy. This holistic perspective has been conceptualised as the biopyschosocial model (see Chs 5 & 11) and suggests there is far more than just the pathology or structure which has an impact on the outcome of the disease. Therefore, a detailed subjective and objective patient assessment, which includes psychosocial factors (Kendall 1997) and health related quality of life, should be obtained (Ch. 4) and a collaborative process used to develop realistic, achievable, measurable patient orientated goals. As all patients with rheumatic disease are different, starting from a different baseline and with different needs, the physiological and psychological impact of each physical therapy should be considered on an individual basis.
ELECTROPHYSICAL AGENTS
SENSORY STIMULATION FOR PAIN RELIEF
Sensory stimulation means applying electrical stimulation with the intention of increasing the afferent nerve input. This effects a change at the spinal or supraspinal level of the neurological system (centrally), which can be used to alter pain perception. The rationale for this treatment is provided by the pain gate theory (Melzack & Wall 1965). This theory proposes that pain perception is regulated by a ‘gate’ at the level of the dorsal column of the spinal cord, which may be opened or closed by means of other inputs from peripheral nerves or the central nervous system (see Ch. 5). Essentially, electrical stimulation is aimed at modifying the peripheral input (stimulation of the A beta mechanoreceptor fibres at the skin) which inhibits nociceptor activity of C and A delta fibres (at the posterior horn) thus changing the level of excitability of the central components of the neurological system, e.g. central nociceptive transmission cells, wide dynamic range neurons (Robertson et al 2006).
Additionally, electrical stimulation is responsible for releasing chemical mediators (e.g. encephalins), which have a morphine type inhibitory effect on the C- fibre (nociceptor) system. Furthermore, activation of the A delta fibres may provoke impulses in the mid brain which inhibit the neurons at the original site via stimulation of the descending inhibitory pathways (Galea 2002). Thus, by changing the sensory input the perception of pain may be altered but not the underlying cause of the pain.
TRANSCUTANEOUS ELECTRICAL NERVE STIMULATION
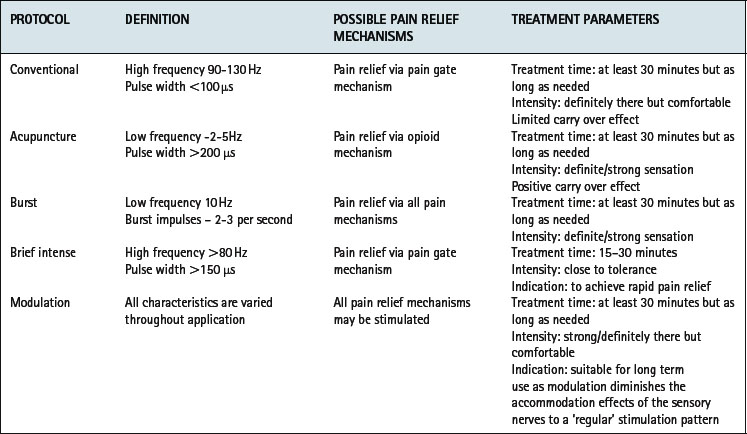
Transcutaneous electrical nerve stimulation (TENS) is an easily applied, non-invasive modality with relatively few contraindications (Fox & Sharp 2007, Robertson et al 2006) which can be readily adopted as a pain management strategy for patients with rheumatic conditions. Small battery operated TENS machines deliver an electrical impulse via surface skin electrodes (Fig. 8.1). Five parameters can be adjusted to achieve most effective pain relief – waveform, pulse duration and frequency, intensity and electrode position. Therapeutic methods of applying TENS are categorized into conventional, ‘acupuncture-like’, burst, brief intense and modulation (Watson 2007). Selection is based on the underlying condition, severity and duration of symptoms (Brosseau et al 2004) (Table 8.1). Recent meta-analyses of six randomised controlled trials (RCT) involving 268 patients with lower limb osteoarthritis (OA) suggest all modes of TENS improve pain, but not range of movement, function or strength regardless of the treatment protocol (Brosseau et al 2004). In patients with knee OA, longer courses of treatment (> 4 weeks) and greater intensity protocols (high burst or low frequency) may produce greatest pain relief (Osiri et al 2000). In people with inflammatory disease, acupuncture-like TENS reduces pain and increases muscle power, whilst conventional TENS improves self reported disease activity but not pain (Brosseau et al 2003a).
Clinical guidelines recommend acupuncture-like TENS for improving pain, oedema and power in patients with RA, (Brosseau et al 2004) as a relatively safe adjunct therapy for the relief of pain in patients with OA (Philadelphia Panel 2001) and for osteoporotic (OP) patients with intractable pain especially those with chronic low back pain and recent vertebral factures (Chartered Society of Physiotherapy 1999).
INTERFERENTIAL THERAPY
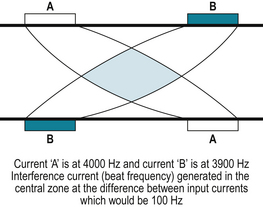
Interferential therapy (IFT) is an alternative method of sensory nerve stimulation, which applies two alternating currents of slightly different frequencies (kHz) at right angles to each other in a continuous stream. Theoretically, where the currents intersect an area of maximum stimulation is produced. However, as the spread of the current reduces the intensity in deep tissues the superimposed current may be less effective than immediately under electrodes and therefore may not achieve the desired therapeutic response (Robertson et al 2006). Clinically, medium frequency currents are applied which pass through the skin more comfortably than a typical low frequency current (due to skin resistance). At the intersection of the currents a beat frequency produces an effect similar to a low frequency current (Fig. 8.2). Using appropriate frequencies, sensory nerve stimulation can be achieved, activating the pain gate mechanism (between 80–130Hz) and opioid mechanisms (< 10Hz) associated with pain relief.
Evidence for the effectiveness of IFT in rheumatic disease is limited but it may reduce pain in patients with psoriatic arthritis (Walker et al 2006) and when combined with ultrasound may reduce pain and improve sleep in patients with fibromyalgia (Almeida et al 2003). However, due to the size of the apparatus, application of IFT is limited to use within the healthcare setting and therefore encourages reliance on healthcare practitioners rather than promoting self-management. Whilst there is some evidence to support the efficacy of sensory stimulation for pain relief no studies directly compare the clinical effectiveness of TENS and IFT. Without evidence of superior efficacy of one form of sensory stimulation, the small, battery operated TENS machine offers a relatively safe, inexpensive, easily self administered method of symptom control in patients with rheumatic diseases.
MOTOR STIMULATION OF INNERVATED MUSCLE
Motor stimulation is the production of a muscle contraction by electrical stimulation of the motor nerves. It is used for; increasing muscle strength and endurance, re-education of motor control, oedema reduction, increasing joint and soft tissue mobility and altering muscle structure and function (trophic changes). Therapeutically it can be used as a sole treatment, (Bircan et al 2002) superimposed over an active muscle contraction (Strojnik 1998) or as an adjunct to an exercise regimen (Fitzgerald et al 2003).
Gradual onset short duration pulses may be selected at frequencies between 30-100 Hz with on-off times and rate of ramping (progression) varying with clinical considerations. The number of repetitions is defined by the training response required and the amplitude is set at maximum individual tolerance. A two second pulse, followed by four second rest with a one second ramp, mimics physiological muscle contraction although the complexity of normal muscle group activity cannot be simulated (Robertson et al 2006).
In patients with rheumatoid arthritis (RA) with secondary disuse atrophy of the first dorsal interosseous of the hand, muscle stimulation improves hand function, strength and fatigue resistance of the first dorsal interosseus muscle (Oldham & Stanley 1989). Similarly, functional performance and quadriceps muscle torque improved by 10% in people with OA knee following muscle stimulation (Talbot et al 2003).
LOW LEVEL LASER THERAPY
Low level laser therapy (LLLT) utilises a pencil-like beam of electromagnetic waves of a single frequency and defined wavelength to promote tissue healing and pain relief in a broad spectrum of soft tissue injuries and diseases. The effects of LLLT are not thermal but photochemical reactions in cells, termed photobioactivation. LLLT produces its physiological and therapeutic effects by applying enough energy to disturb local electron orbits, initiate chemical change, disrupt molecular bonds and produce free radicals at the cell membrane to control the inflammatory response, promote healing and pain relief (Box 8.1) (Robertson et al 2006, Watson 2000).
BOX 8.1 The potential photobioactivation effects of low level laser therapy
Activation & proliferation of fibroblasts
Alteration of cell membrane potentials
Stimulation of immune responses
Alteration of action potentials
Altered prostaglandin production
Altered endogenous opioid production
In patients with rheumatic disease the evidence for the use of LLLT is mixed. In patients with OA, LLLT is ineffective for pain relief (Brosseau et al 2005). However, LLLT is recommended in clinical practice guidelines for patients with RA as it improves pain and morning stiffness, but not function, range of movement, joint tenderness or swelling (Brosseau et al 2004).
ULTRASOUND THERAPY
In the management of rheumatic diseases, ultrasound therapy (US) is commonly used as an adjunctive therapy for its proposed effects on inflammation as well as for pain relief. It uses sound waves at very high frequencies (0.5-5 MHz) to produce mechanical vibration within the tissues. If applied in high doses absorption of US results in heating, which decreases pain and fluid viscosity, increases metabolic rate and blood flow (thermal effects) (Nussbaum 1997). At lower doses of US or following pulsed US non thermal, mechanical effects such as stable cavitation (formation of gas bubbles in tissues), standing waves (reflected waves superimposed on incident waves) and acoustic streaming (fluid movement which exerts pressure changes on a cell) occur (Maxwell 1992) which cause membrane distortion, increased permeability, increased nutrient transfer and facilitation of tissue repair (Mortimer & Dyson 1988). When applied to acutely inflamed tissues it encourages the inflammatory process to progress to the proliferation stage (Watson 2000).
Whilst there is evidence to support the physiological effects of US in laboratory or animal studies, (Mortimer & Dyson 1988) evidence for its clinical effectiveness in people with rheumatic conditions is limited (Brosseau et al 2004, Zhang et al 2007) and it is only recommended for those with arthritis of the hand (Casimiro et al 2002, Welch et al 2001). Moreover, a recent review concludes US may only be effective for people with carpal tunnel syndrome and those with calcific tendonitis of the shoulder (Roberston & Baker 2001) despite being a frequently used electrophysical modality in musculoskeletal conditions (Kitchen & Partridge 1996).
SHORT WAVE THERAPY
Short wave diathermy (SWD) produces its physiological and therapeutic effects by rapidly alternating electrical and magnetic currents at short wave frequencies (27.12 MHz). Continuous SWD is applied to tissues either inductively (metal cable, covered in insulating rubber, which is wrapped around the part to be treated) or capacitively (plate or malleable electrodes placed next to the area to be treated), usually for 20–30 minutes. It increases skin temperature by 3-7°C, muscle temperature by 2-6°C (Robertson et al 2006) and intra-articular heating has also been demonstrated (Oosterveld et al 1992).
Pulsed short wave diathermy (PSWD) or pulsed electromagnetic energy (PEME) is an intermittent oscillating high frequency (27.12MHz) output. The mean power depends on the peak (pulse) power, duration and frequency of the pulse. As a thermal effect is only produced with outputs above 7 Watts, the non thermal physiological effects of PSWD are postulated to occur due to agitation of ions, molecules, membranes and perhaps cells which accelerates membrane transport, phagocytic, and enzymatic activity (Kitchen & Partridge 1992, Low 1995, Robertson et al 2006).
Brief, high intensity bursts of electromagnetic energy:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree