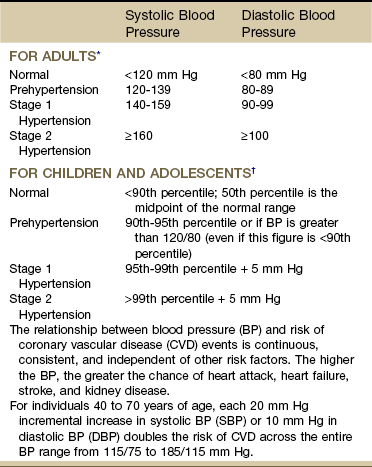
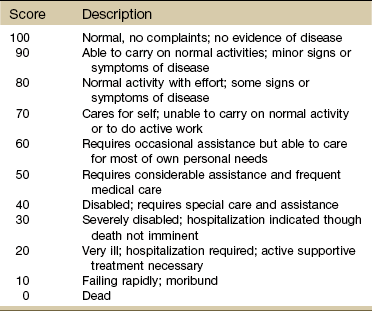
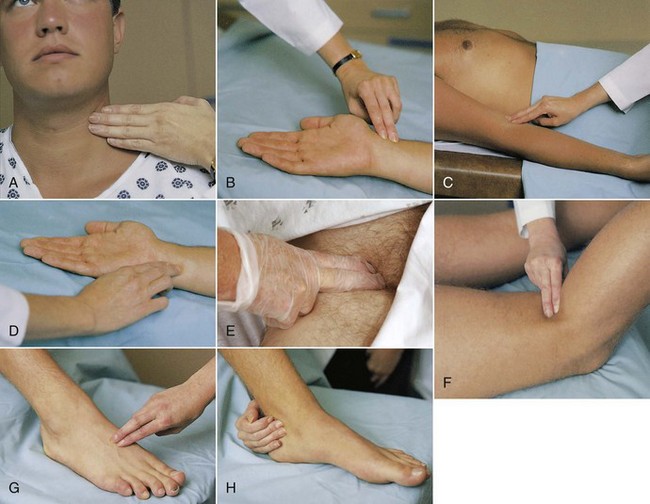
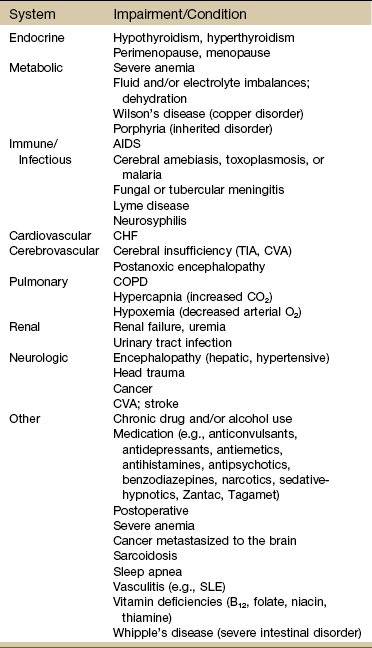
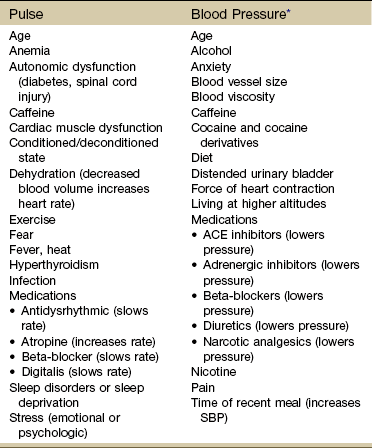
Chapter 4 In most situations, it is advised to assess one system above and below the area of complaint based on evidence supporting a regional-interdependence model of musculoskeletal impairments (i.e., symptoms present may be caused by musculoskeletal impairments proximal or distal to the site of presenting symptoms distinct from the phenomenon of referred pain).1 Documentation of physical findings is important. From a legal standpoint, if you did not document it, you did not assess it. Look for changes from the expected norm, as well as changes for the client’s baseline measurements. Use simple and clear documentation that can be understood and used by others. As much as possible, record both normal and abnormal findings for each client.2 Keep in mind that the client’s cultural and educational background, beliefs, values, and previous experiences can influence his or her response to questions. The use of quick and easy screening tools such as the Physical Therapist Community Screening Form for Aging Adults can help therapists identify limitations to optimal heath, wellness, and fitness in any of seven areas (e.g., posture, flexibility, strength, balance, cardiovascular fitness) for adults aged 65 and older. With the 2007 House of Delegates position statement recommending that all individuals visit a physical therapist at least once a year to promote optimal health and wellness, evidence-based tests of this type will become increasingly available.3 Physical assessment begins the moment you meet the client as you observe body size and type, facial expressions, evaluate self-care, and note anything unusual in appearance or presentation. Keep in mind (as discussed in Chapter 2) that cultural factors may dictate how the client presents himself (e.g., avoiding eye contact when answering questions, hiding or exaggerating signs of pain). A few pieces of equipment in a small kit within easy reach can make the screening exam faster and easier (Box 4-1). Using the same pattern in screening each time will help the therapist avoid missing important screening clues. The therapist must be aware of any factor that can affect a client’s current mental status. Shock, head injury, stroke, hospitalization, surgery (use of anesthesia), medications, age, and the use of substances and/or alcohol (see discussion, Chapter 2) can cause impaired consciousness. Other factors affecting mental status may include malnutrition, exposure to chemicals, and hypothermia or hyperthermia. Depression and anxiety (see discussion, Chapter 3) also can affect a client’s functioning, mood, memory, ability to concentrate, judgment, and thought processes. Educational and socioeconomic background along with communication skills (e.g., English as a second language, aphasia) can affect mental status and function. The cause of deterioration in mental ability is unknown. In some cases, delirium/dementia appears to be triggered by the shock to the body from anesthesia and surgery.4 It may be a passing phase with complete recovery by the client, although this can take weeks to months. The likelihood of delirium associated with hospitalization is much higher with hip fractures and hip and knee joint replacements,5,6 possibly attributed to older age, slower metabolism, and polypharmacy (more than four prescribed drugs at admission).7 The therapist should pay attention to risk factors (Box 4-2) and watch out for any of the signs or symptoms of delirium. Physical exam should include vital signs with oxygen concentration measured, neurologic screening exam, and surveillance for signs of infection. A medical diagnosis is needed to make the distinction between postoperative delirium, baseline dementia, depression, and withdrawal from drugs and alcohol.5 Several scales are used to assess level of consciousness, performance, and disability. The Confusion Assessment Method (CAM) is a bedside rating scale physical therapists can use to assess hospitalized or institutionalized individuals for delirium. This tool has been adapted for use with patients who are ventilated and in an intensive care unit (CAM-ICU).8 There are two parts to the assessment instrument: part one screens for overall cognitive impairment. Part two includes four features that have the greatest ability to distinguish delirium or reversible confusion from other types of cognitive impairment. The tool identifies the presence of delirium but does not assess the severity of the condition.9 As a screening tool, the CAM has been validated for use by physicians and nurses in palliative care and intensive care settings (sensitivity of 94% to 100% and specificity of 90% to 95%). Values for positive predictive accuracy were 91% to 94%, and values for negative predictive accuracy were 100% and 90% for the two populations assessed (general medicine, outpatient geriatric center).9 The Glasgow Outcome Scale10,11 describes patients/clients on a 5-point scale from good recovery (1) to death (5). Vegetative state, severe disability, and moderate disability are included in the continuum. This and other scales and clinical assessment tools are not part of the screening assessment but are available online for use by health care professionals.12 The Karnofsky Performance Scale (KPS) in Table 4-1 is used widely to quantify functional status in a wide variety of individuals, but especially among those with cancer. It can be used to compare effectiveness of intervention and to assess individual prognosis. The lower the Karnofsky score, the worse the prognosis for survival. The most practical performance scale for use in any rehabilitation setting for most clients is the Eastern Cooperative Oncology Group (ECOG) Performance Status Scale (Table 4-2). Researchers and health care professionals use these scales and criteria to assess how an individual’s disease is progressing, to assess how the disease affects the daily living abilities of the client, and to determine appropriate treatment and prognosis. TABLE 4-2 ECOG, Eastern Cooperative Oncology Group. From Oken MM, Creech RH, Tormey DC, et al: Toxicity and response criteria of the Eastern Cooperative Oncology Group, Am J Clin Oncol 5:649-655, 1982. Available at www.ecog.org/general/perf_stat.html. Confusion is not a normal change with aging and must be reported and documented. Confusion is often associated with various systemic conditions (Table 4-3). Increased confusion in a client with any form of dementia can be a symptom of infection (e.g., pneumonia, urinary tract infection), electrolyte imbalance, or delirium. Likewise, a sudden change in muscle tone (usually increased tone) in the client with a neurologic disorder (adult or child) can signal an infectious process. TABLE 4-3 Systemic Conditions Associated with Confusional States Modified from Dains JE, Baumann LC, Scheibel P: Advanced health assessment & clinical diagnosis in primary care, ed 2, St. Louis, 2003, Mosby; p 425. Be aware in the health history of any risk factors for nutritional deficiencies (Box 4-3). Remember that some medications can cause appetite changes and that psychosocial factors such as depression, eating disorders, drug or alcohol addictions, and economic variables can affect nutritional status. It may be necessary to determine the client’s ideal body weight by calculating the body mass index (BMI).13,14 Several websites are available to help anyone make this calculation. There is a separate website for children and teens sponsored by the National Center for Chronic Disease Prevention and Health Promotion.15 The need for therapists to assess vital signs, especially pulse and blood pressure is increasing.16 Without the benefit of laboratory values, physical assessment becomes much more important. Vital signs, observations, and reported associated signs and symptoms are among the best screening tools available to the therapist. Vital sign assessment is an important tool because high blood pressure is a serious concern in the United States. Many people are unaware they have high blood pressure. Often primary orthopedic clients have secondary cardiovascular disease.17 Physical therapists practicing in a primary care setting will especially need to know when and how to assess vital signs. The Guide to Physical Therapist Practice18 recommends that heart rate (pulse) and blood pressure measurements be included in the examination of new clients. Exercise professionals are strongly encouraged to measure blood pressure during each visit.19 Taking a client’s vital signs remains the single easiest, most economic, and fastest way to screen for many systemic illnesses. All the vital signs are important (Box 4-4); temperature and blood pressure have the greatest utility as early screening tools for systemic illness or disease, while pulse, blood pressure, and oxygen (O2) saturation level offer valuable information about the cardiovascular/pulmonary systems. Normal ranges of values for the vital signs are provided for the therapist’s convenience. However, these ranges can be exceeded by a client and still represent normal for that person. Keep in mind that many factors can affect vital signs, especially pulse and blood pressure (Table 4-4). Substances such as alcohol, caffeine, nicotine, and cocaine/cocaine derivatives as well as pain and stress/anxiety can cause fluctuations in blood pressure. Adults who monitor their own blood pressure may report wide fluctuations without making the association between these and other factors listed. It is the unusual vital sign in combination with other signs and symptoms, medications, and medical status that gives clinical meaning to the pulse rate, blood pressure, and temperature. TABLE 4-4 Factors Affecting Pulse and Blood Pressure SBP, Systolic blood pressure; ACE, angiotensin-converting enzyme. *Conditions, such as chronic kidney disease, renovascular disorders, primary aldosteronism, and coarctation of the aorta, are identifiable causes of elevated blood pressure. Chronic overtraining in athletes, use of steroids and/or nonsteroidal antiinflammatory drugs (NSAIDs), and large increases in muscle mass can also contribute to hypertension.38 Treatment for hypertension, dehydration, heart failure, heart attack, arrhythmias, anaphylaxis, shock (from severe infection, stroke, anaphylaxis, major trauma), and advanced diabetes can cause low blood pressure. From Goodman CC, Fuller K: Pathology: implications for the physical therapist, ed 3, Philadelphia, 2009, WB Saunders. Do not rely on pulse oximeter devices for pulse rate because these units often take a sample pulse rate that reflects a mean average and may not reveal dysrhythmias (e.g., a regular irregular pulse rate associated with atrial fibrillation). It is recommended that the pulse always be checked in two places in older adults and in anyone with diabetes (Fig. 4-1). Pulse strength (amplitude) can be graded as Keep in mind that taking the pulse measures the peripheral arterial wave propagation generated by the heart’s contraction—it is not the same as measuring the true heart rate (and should not be recorded as heart rate when measured by palpation). A true measure of heart rate requires auscultation or electrocardiographic recording of the electrical impulses of the heart. The distinction between pulse rate and heart rate becomes a matter of concern in documentation liability and even greater importance for individuals with dysrhythmias. In such cases, the output of blood by some beats may be insufficient to produce a detectable pulse wave that would be discernible with an electrocardiogram.20 Pulse amplitude that fades with inspiration instead of strengthening and strengthens with expiration instead of fading is paradoxic and should be reported to the physician. Paradoxic pulse occurs most commonly in clients with chronic obstructive pulmonary disease (COPD) but is also observed in clients with constrictive pericarditis.21 A pulse increase with activity of more than 20 bpm lasting for more than 3 minutes after rest or changing position should also be reported. Other pulse abnormalities are listed in Box 4-5. When taking the resting pulse or pulse during exercise, some clinicians measure the pulse for 15 seconds and multiply by 4 to get the rate per minute. For a quick assessment, measure for 6 seconds and add a zero. A 6-second pulse count can result in an error of 10 bpm if a 1-beat error is made in counting. For screening purposes, it is always best to palpate the pulse for a full minute. Longer pulse counts give greater accuracy and provide more time for detection of some dysrhythmias (Box 4-6).19 Pulse assessment following vascular injuries (especially dislocation of the knee) should not be relied upon as the only diagnostic testing procedure as occult arterial injuries can be present even when pulses are normal. A meta-analysis of 284 dislocated knees concluded that abnormal pulse examinations have a sensitivity of .79 and specificity of .91 for detection of arterial injuries.22,23 On the other hand, there are reports of normal pulse examinations at the time of the initial knee injury in people who later developed ischemia leading to amputation.24,25 Any condition that restricts blood flow (including cold hands) can result in inaccurate SaO2 readings. Relaxation and physiologic quieting techniques can be used to help restore more normal temperatures in the distal extremities. A handheld device such as the PhysioQ26 can be used by the client to improve peripheral circulation. Do not apply a pulse oximetry sensor to an extremity with an automatic blood pressure cuff.27 SaO2 levels can be affected also by positioning because positioning can impact a person’s ability to breathe. Upright sitting in individuals with low muscle tone or kyphosis can cause forward flexion of the thoracic spine compromising oxygen intake. Tilting the person back slightly can open the trunk, ease ventilation, and improve SaO2 levels.28 Using SaO2 levels may be a good way to document outcomes of positioning programs for clients with impaired ventilation. Other factors affecting pulse oximeter readings can include nail polish and nail coverings, irregular heart rhythms, hyperemia (increased blood flow to the area), motion artifact, pressure on the sensor, electrical interference, and venous congestion.20 BP depends on many factors; the normal range differs slightly with age and varies greatly among individuals (see Table 4-4). Normal systolic BP (SBP) ranges from 100 to 120 mm Hg, and diastolic BP (DBP) ranges from 60 to 80 mm Hg. Highly trained athletes may have much lower values. Target ranges for BP are listed in Table 4-5 and Box 4-7. TABLE 4-5 Classification of Blood Pressure *From The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH Publication No. 03-5233, May 2003. National Heart, Lung, and Blood Institute (NHLBI) www.nhlbi.nih.gov/. †From National Heart, Lung, and Blood Institute (NHLBI): Fourth Report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents, Pediatrics 114(2):555-576, August 2004. Assessing Blood Pressure: BP should be taken in the same arm and in the same position (supine or sitting) each time it is measured. The baseline BP values can be recorded on the Family/Personal History form (see Fig. 2-2). Cuff size is important and requires the bladder width-to-length be at least 1 : 2. The cuff bladder should encircle at least 80% of the arm. BP measurements are overestimated with a cuff that is too small; if a cuff is too small, go to the next size up. Keep in mind that if the cuff is too large, falsely lower BPs may be recorded.29 Although it is often recommended that anyone who has had bilateral axillary node dissection should have BP measurements taken in the leg, this is not standard clinical practice across the United States.30 Leg pressures can be difficult to assess and inaccurate. Some oncology staff advise taking BP in the arm with the least amount of nodal dissection. Technique in measuring BP is a key factor in all clients, especially those with ALND (Box 4-8). A common mistake is to pump the BP cuff up until the systolic measurement is 200 mm Hg and then take too long to lower the pressure or to repeat the measurement a second time without waiting. Repeating the BP without a 1-minute wait time may damage the blood vessel and set up an inflammatory response.31 This poor technique is to be avoided, especially in clients at risk for lymphedema or who already have lymphedema. Take the BP twice at least a minute apart in both arms. If both measurements are within 5 mm Hg of each other, record this as the resting (baseline) measurement. If not, wait 1 minute and take the BP a third time. Monitor the BP in the arm with the highest measurements.21 Record measurements exactly; do not round numbers up or down as this can result in inaccuracies.32 For clients who have had a mastectomy without ALND (i.e., prophylactic mastectomy), BP can be measured in either arm. These recommendations are to be followed for life.33 Until automated BP devices are improved enough to ensure valid and reliable measurements, the BP response to exercise in all clients should be taken manually with a BP cuff (sphygmomanometer) and a stethoscope.33 It is advised to invest in the purchase of a well-made, reliable stethoscope. Older models with tubing long enough to put the earpieces in your ears and still place the bell in a lab coat pocket should be replaced. Tubing should be no more than 50 to 60 cm (12 to 15 inches) and 4 mm in diameter. Longer and wider tubing can distort transmitted sounds.34 For the student or clinician learning to take vital signs, it may be easier to hear the BP (tapping, Korotkoff) sounds in adults using the left arm because of the closer proximity to the left ventricle. Arm position does make a difference in BP readings. BP measurements are up to 10% higher when the elbow is at a right angle to the body with the elbow flexed at heart level. The preferred position is seated with the arms parallel and extended in a forward direction (if supine, then parallel to the body).35 Pulse Pressure: The difference between the systolic and diastolic pressure readings (SBP − DBP) is called pulse pressure normally around 40 mm Hg. Pulse pressure is an index of vascular aging (i.e., loss of arterial compliance and indication of how stiff the arteries are). A widened resting pulse pressure often results from stiffening of the aorta secondary to atherosclerosis. Resting pulse pressure consistently greater than 60 to 80 mm Hg is a yellow (caution) flag and is a risk factor for new onset of atrial fibrillation.36 Widening of the pulse pressure is linked to a significantly higher risk of stroke and heart failure after the sixth decade. Some BP medications increase resting pulse pressure width by lowering diastolic pressure more than systolic while others (e.g., angiotensin-converting enzyme [ACE] inhibitors) can lower pulse pressure.37 In a normal, healthy adult, the pulse pressure generally increases in direct proportion to the intensity of exercise as the SBP increases and DBP stays about the same.38 A difference of more than 80 to 100 mm Hg taken during or right after exercise should be evaluated carefully. In a healthy adult, pulse pressure will return to normal within 3 to 10 minutes following moderate exercise. The key is to watch for pulse pressures that are not accommodating during exercise. Expect to see the systolic rise slightly while diastolic stays the same. If diastolic drops while systolic rises or if the pulse width exceeds 100 mm Hg, further assessment and evaluation is needed. Depending on all other parameters (e.g., general health of the client, past medical history, medications, concomitant associated signs and symptoms), the therapist may monitor pulse pressures over a few sessions and look for a pattern (or lack of pattern) to report if/when generating a medical consult.39 Variations in Blood Pressure: There can be some normal variation in SBP from side to side (right extremity compared to left extremity). This is usually no more than 5 to 10 mm Hg DBP or SBP (arms) and 10 to 40 mm Hg SBP (legs). A difference of 10 mm Hg or more in either systolic or diastolic measurements from one extremity to the other may be an indication of vascular problems (look for associated symptoms; in the upper extremity test for thoracic outlet syndrome). Normally the SBP in the legs is 10% to 20% higher than the brachial artery pressure in the arms. BP readings that are lower in the legs as compared with the arms are considered abnormal and should prompt a medical referral for assessment of peripheral vascular disease.33 On the other hand, women of reproductive age taking birth control pills may be at increased risk for hypertension, heart attack, or stroke. The risk of a cardiovascular event is very low with today’s low-dose oral contraceptives. However, smoking, hypertension, obesity, undiagnosed cardiac anomalies, and diabetes are factors that increase a woman’s risk for cardiovascular events. Any woman using oral contraceptives who presents with consistently elevated BP values must be advised to see her physician for close monitoring and follow-up.40,41 Blood Pressure Changes with Exercise: As mentioned, the SBP increases with increasing levels of activity and exercise in a linear fashion. In a healthy adult under conditions of minimal to moderate exercise, look for normal change (increase) in SBP of 20 mm Hg or more. Diastolic should be the same side to side with less than 10 mm Hg difference observed. DBP generally remains the same or decreases slightly during progressive exercise.38 In an exercise-testing situation, the ACSM recommends stopping the test if the SBP exceeds 260 mm Hg.38 In a clinical setting without the benefit of cardiac monitoring, exercise or activity should be reduced or stopped if the systolic pressure exceeds 200 mm Hg. This is a general (conservative) guideline when exercising a client without the benefit of cardiac testing (e.g., electrocardiogram [ECG]). This stop-point is based on the ACSM guideline to stop exercise testing at 115 mm Hg DBP. Other sources suggest activity should be decreased or stopped if the DBP exceeds 130 mm Hg.42 Hypertension (See Further Discussion on Hypertension in Chapter 6): In recent years, an unexpected increase in illness and death caused by hypertension has prompted the National Institutes of Health (NIH) to issue new guidelines for more effective BP control. More than one in four Americans has high blood pressure, increasing their risk for heart and kidney disease and stroke.43 In adults hypertension is a systolic pressure above 140 mm Hg or a diastolic pressure above 90 mm Hg. Consistent BP measurements between 120 and 139 (systolic) and between 80 and 89 diastolic is classified as pre-hypertensive. The overall goal of treating clients with hypertension is to prevent morbidity and mortality associated with high blood pressure. The specific objective is to achieve and maintain arterial blood pressure below 120/80 mm Hg, if possible (Box 4-9).34
Physical Assessment as a Screening Tool
General Survey
Mental Status
Risk Factors for Delirium
Grade
Level of Activity
0
Fully active, able to carry on all pre-disease performance without restriction (Karnofsky 90%-100%)
1
Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature (e.g., light house work, office work) (Karnofsky 70%-80%)
2
Ambulatory and capable of all self-care but unable to carry out any work activities. Up and about more than 50% of waking hours (Karnofsky 50%-60%)
3
Capable of only limited self-care, confined to bed or chair more than 50% of waking hours (Karnofsky 30%-40%)
4
Completely disabled. Cannot carry on any self-care. Totally confined to bed or chair (Karnofsky 10%-20%)
5
Dead (Karnofsky 0%)
Nutritional Status
Vital Signs
Pulse Rate
0
Absent, not palpable
1+
Pulse diminished, barely palpable
2+
Easily palpable, normal
3+
Full pulse, increased strength
4+
Bounding, too strong to obliterate
Pulse Oximetry
Blood Pressure