Periprosthetic Fractures
TOTAL HIP ARTHROPLASTY
Femoral Shaft Fractures
Epidemiology
Intraoperative: There is a 0.3% up to 5% incidence overall, including cemented and uncemented components.
Postoperative: There is a 0.1% incidence.
They occur more frequently with noncemented components, with an incidence of 2.6% to 5% to as high as 21% for noncemented revisions.
Mortality associated with age >70 years and male sex (men 2.1% vs. 1.2% in women).
Risk Factors
Osteopenia: Osteoporosis or bone loss secondary to osteolysis
Rheumatoid arthritis
Total hip arthroplasty (THA) following failed open reduction and internal fixation (ORIF)
Stress risers secondary to cortical defects
Revision surgery
Inadequate implant site preparation: Large implant with inadequate reaming or broaching may be responsible.
Pericapsular pathology: A scarred capsule with inadequate release may result in intraoperative fracture.
Loose components: Loose femoral components are responsible for up to 33% of periprosthetic femur fractures.
Surgical Considerations (to Avoid Periprosthetic Fracture During Revision Surgery)
Use longer stem prosthesis, spanning twice the bone diameter beyond the defect.
Consider bone grafting the defect.
Consider strut allograft or plate support.
Place cortical windows in an anterolateral location on the femur in line with the neutral bending axis.
Leave cortical windows <30% of the bone diameter.
Choose the correct starting point for reaming and broaching.
Classification
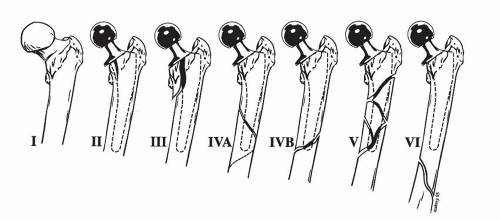
American Academy of Orthopaedic Surgeons Classification (Fig. 6.1) This divides the femur into three separate regions:
Level I: Proximal femur distally to the lower extent of the lesser trochanter
Level II: 10 cm of the femur distal to level I
Level III: Covers remainder of femur distal to level II
Type I: Fracture proximal to the intertrochanteric line that usually occurs during dislocation of the hip
Type II: Vertical or spiral split that does not extend past the lower extent of the lesser trochanter
Type III: Vertical or spiral split that extends past the lower extent of the lesser trochanter but not beyond level II, usually at the junction of the middle and distal thirds of the femoral stem
Type IV: Fractures that traverse or lie within the area of the femoral stem in level III, with type IVA being a spiral fracture around the tip and type IVB being a simple transverse or short oblique fracture
Type V: Severely comminuted fractures around the stem in level III
Type VI: Fractures distal to the stem tip, also in level III
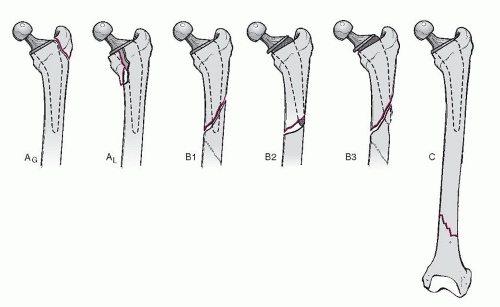
Vancouver Classification (Fig. 6.2)
Type A: Fracture in the trochanteric region
AG: Greater trochanteric region
AL: Lesser trochanteric region
Type B: Around or just distal to the stem
B1: Stable prosthesis
B2: Unstable prosthesis
B3: Unstable prosthesis plus inadequate bone stock
Type C: Well below the stem
Treatment Principles
Treatment depends on:
Location of the fracture
Stability of the prosthesis
A loose stem should be revised.
Bone stock
Age and medical condition of the patient
Accurate reduction and secure fixation
Options include:
Nonoperative treatment: limited weight bearing, brace, cast, or traction
ORIF (with plate and screws or cable and/or strut allograft)
Revision plus ORIF
Vancouver Type A Fractures
These are usually stable and minimally displaced.
ORIF is used to maintain abductor function with wide displacement.
Revision of acetabular component is indicated with severe polyethylene wear.
Vancouver Type B1 Fractures
These are usually treated with internal fixation.
Options for fixation include:
Wires or cables
Plate and screws and/or cables
Open versus percutaneous plate placement
Cortical onlay allograft—may or may not incorporate
Combination
Long-term results depend on:
Implant alignment
Preservation of the periosteal blood supply
Adequacy of stress riser augmentation
Vancouver Type B2 Fractures
Revision arthroplasty and ORIF are used.
Choice of implant includes:
Uncemented prosthesis
Extensive coated long-stem curved prosthesis
Fluted long-stem prosthesis
Modular implants
Cemented prosthesis
Vancouver Type B3 Fractures
No sufficient bone stock supports the revision prosthesis.
Options include:
Proximal femoral reconstruction
Composite allograft
Scaffold technique
Proximal femoral replacement
Treatment depends on:
The age of the patient
The severity of the bone defect
The functional class of the patient
Vancouver Type C Fractures
Treat independently of the arthroplasty.
Use a plate and screws and/or cables, usually without a strut allograft.
Do not create any new stress riser—bypass stemmed implant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree