Periprosthetic Fractures of the Pelvis Associated with Hip Arthroplasty
Mihai H. Vioreanu
Donald S. Garbuz
Bassam A. Masri
Clive P. Duncan
Case Presentation
During a routine cementless total hip replacement in a healthy and active 65-year-old female, it is noted that the shell has seated too far medially and it is unstable. The shell is removed and evaluation reveals a displaced and unstable fracture of the floor and both columns of the acetabulum. It is concluded that overzealous reaming and/or excessive cup insertion force were responsible. The wound is closed and the case transferred to a more specialized center. A postoperative radiograph confirms the diagnosis (Fig. 87.1).
In this chapter we will present a historical review of this uncommon injury and introduce a new classification system that includes the pelvis as a whole, not just the acetabulum alone. Next we will cover the risk factors and methods of prevention. The principles of fracture evaluation and management will follow. Finally we will detail how the introductory case was treated.
Historical Review and Risk Factors
Periprosthetic fracture of the pelvis associated with hip replacement is a relatively rare event. The bulk of the literature up to now has focused on the acetabulum alone. Cemented fixation of the acetabular component is associated with a very low rate of this complication. In 1974, McElfresh and Coventry were first to report a displaced periprosthetic acetabular fracture associated with a failed cemented acetabular component. This was a late postoperative fracture and was associated with a deep periprosthetic joint infection. They had only one such fracture among 5,400 cemented hip replacements (a prevalence <0.02%) (1). In 1972, Miller described ischiopubic fractures following the insertion of a Ring component without cement in five hips (2).
Since then, the prevalence of periprosthetic acetabular fractures has increased with the evolution and widespread use of cementless, press-fit acetabular designs. The majority of these fractures occur intraoperatively during insertion of the acetabular component, and most are nondisplaced fractures with little or no effect on cup stability. In one series of 7,121 primary total hip arthroplasties an intraoperative acetabular fracture was identified during 21 of 5,359 (a prevalence of 0.4%) primary THA performed with an uncemented acetabular component. No acetabular fractures occurred during insertion of the 1,762 cemented acetabular components. Of the 21 fractures, 17 were stable and four were treated with supplemental screw fixation (3).
Sharkey et al. (4) published a series of 13 intraoperative acetabular fractures that occurred during the insertion of uncemented components. Only nine were diagnosed intraoperatively. No prevalence of intraoperative acetabular fractures was given in the article. Two other varieties of periprosthetic acetabular fractures, which occur much less commonly, are late fractures associated with severe pelvic bone loss (commonly referred to as pelvic discontinuity) and those that occur as a result of a traumatic injury. Late postoperative periprosthetic fractures of the acetabulum analyzed from the Mayo Clinic Total Joint Registry found only 16 fractures in 23,850 cases (a prevalence of 0.07%) (5).
Prevention of periprosthetic fractures associated with insertion of the acetabular cup includes accurate preoperative templating to anticipate the likely size of the acetabular component and avoid overreaming of the acetabulum. Overzealous reaming of the acetabulum will weaken the host bone, predisposing it to intraoperative fracture. At the time of surgery, clear identification of the medial wall of the acetabulum by clearing soft tissue from the cotyloid fossa is critical (Fig. 87.2). Reaming beyond this point is discouraged. If there is a question regarding the depth of reaming a short drill can be used to penetrate the medial wall or an intraoperative radiograph can be obtained.
Historically, a variety of techniques and cup designs have been developed to improve the initial stability of fixation and to reduce the amount of micromotion at the bone–implant
interface, allowing rigid bone ingrowth to occur. Spikes, lugs, and screws through the dome of the component or around the periphery of the socket have been shown to augment initial fixation of porous-coated acetabular components (6,7,8,9,10,11). Concerns over fretting associated with the use of screws and accelerated polyethylene wear (12), have led to the development of other methods of improving initial stability. One technique that has been suggested for enhancing initial stability is the use of an oversized component, press-fitted into an underreamed acetabulum (13,14,15,16). Too great a discrepancy between reamed size and cup size may cause excessive hoop stresses that lead to intraoperative fracture. In an in vitro study of acetabular components inserted into human cadaveric specimens, Kim et al. reported fractures in 4 of 30 acetabula that had been underreamed by 2 mm, and 14 of 30 that had been underreamed by 4 mm. They reported high forces (2,000 N) were required to seat acetabular components that are oversized (17). Our preference for reaming when inserting hemispherical acetabular cups is for the last reamer to be 1 to 2 mm smaller than the outside diameter of the planned cup. Further, it is important to recognize that when inserting a cementless cup into a larger acetabulum (e.g., 60 mm or more) the same 1 to 2 mm of underreaming may be more easily tolerated than in a smaller acetabulum (smaller than 50 mm) where this same difference a much larger proportional press-fit.
interface, allowing rigid bone ingrowth to occur. Spikes, lugs, and screws through the dome of the component or around the periphery of the socket have been shown to augment initial fixation of porous-coated acetabular components (6,7,8,9,10,11). Concerns over fretting associated with the use of screws and accelerated polyethylene wear (12), have led to the development of other methods of improving initial stability. One technique that has been suggested for enhancing initial stability is the use of an oversized component, press-fitted into an underreamed acetabulum (13,14,15,16). Too great a discrepancy between reamed size and cup size may cause excessive hoop stresses that lead to intraoperative fracture. In an in vitro study of acetabular components inserted into human cadaveric specimens, Kim et al. reported fractures in 4 of 30 acetabula that had been underreamed by 2 mm, and 14 of 30 that had been underreamed by 4 mm. They reported high forces (2,000 N) were required to seat acetabular components that are oversized (17). Our preference for reaming when inserting hemispherical acetabular cups is for the last reamer to be 1 to 2 mm smaller than the outside diameter of the planned cup. Further, it is important to recognize that when inserting a cementless cup into a larger acetabulum (e.g., 60 mm or more) the same 1 to 2 mm of underreaming may be more easily tolerated than in a smaller acetabulum (smaller than 50 mm) where this same difference a much larger proportional press-fit.
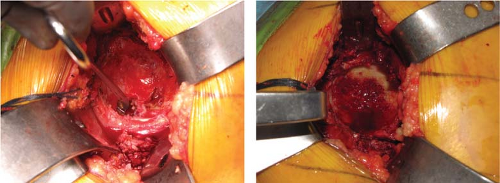 Figure 87.2. Intraoperative pictures showing identification of the medial acetabular wall before and after reaming. (Courtesy of Craig J. Della Valle, MD.) |
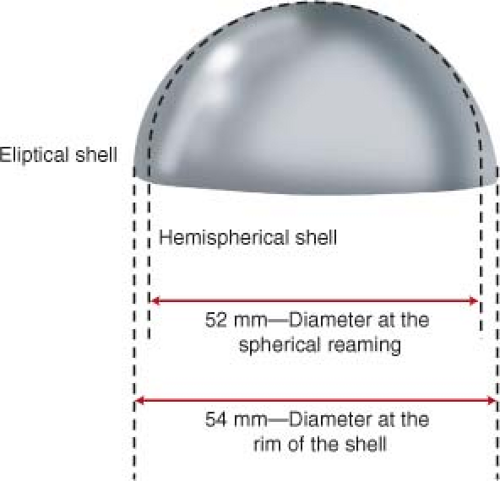
Care must be taken to understand the true outside diameter of the socket in use as the difference between the implant label and implant size can vary between manufacturers. One design, the modular trabecular metal (MTM) shell, (Zimmer, Warsaw, Indiana) has a nominal size designation which is 2 mm smaller than the true diameter of the rim of that elliptical design. Therefore a 60-mm MTM shell is in fact 62 mm in diameter at its mouth or rim. The practice of routinely reaming the acetabulum 2 mm smaller than the “size” of the shell would result in a 4-mm true difference and increase the likelihood of an insertional fracture, especially in the revision setting, in which this cup design is most commonly used (Fig. 87.3).
Haidukewych et al. reported on 21 intraoperative fractures of the acetabulum during total hip arthroplasty. They categorized cup designs into three general types: elliptical monoblock (Implex; Zimmer, Warsaw, Indiana), elliptical modular (reflection [Smith and Nephew, Memphis, Tennessee],
peripheral self-locking [PSL; Stryker Howmedica Osteonics, Mahwah, New Jersey]), and hemispherical modular (Trilogy [Zimmer] and Harris-Galante II [HG-II; Zimmer]). Elliptical shells have a peripheral flare (an increase in diameter) at the periphery to theoretically improve rim press-fit (Fig. 87.3). The study documented significantly higher fracture rates (19 of 21) in association with an elliptical monoblock component fabricated from tantalum that was inserted into a bed that had been prepared with a hemispherical reamer. Porous tantalum has a much higher coefficient of friction than a beaded or fiber-mesh surface does, and acetabular components that are made from this material can require substantially more force to seat. They recommend that surgeons using elliptical designs should match the diameter of the last reamer used to the real diameter of the acetabular component prior to impaction aiming for a difference of 1 to 2 mm, regardless of the cup design used. They postulate that the high (3.5%) fracture rate associated with the Implex design was due to a combination of the rim flare, the increased frictional coefficient of the tantalum, the younger age of the patients for whom these components were typically chosen because their bone is stiffer, and most importantly the monoblock design, which does not allow visual confirmation of complete component seating (3). Surgeons using such designs should be cognizant of the increased risk of fracture associated with this type of implant.
peripheral self-locking [PSL; Stryker Howmedica Osteonics, Mahwah, New Jersey]), and hemispherical modular (Trilogy [Zimmer] and Harris-Galante II [HG-II; Zimmer]). Elliptical shells have a peripheral flare (an increase in diameter) at the periphery to theoretically improve rim press-fit (Fig. 87.3). The study documented significantly higher fracture rates (19 of 21) in association with an elliptical monoblock component fabricated from tantalum that was inserted into a bed that had been prepared with a hemispherical reamer. Porous tantalum has a much higher coefficient of friction than a beaded or fiber-mesh surface does, and acetabular components that are made from this material can require substantially more force to seat. They recommend that surgeons using elliptical designs should match the diameter of the last reamer used to the real diameter of the acetabular component prior to impaction aiming for a difference of 1 to 2 mm, regardless of the cup design used. They postulate that the high (3.5%) fracture rate associated with the Implex design was due to a combination of the rim flare, the increased frictional coefficient of the tantalum, the younger age of the patients for whom these components were typically chosen because their bone is stiffer, and most importantly the monoblock design, which does not allow visual confirmation of complete component seating (3). Surgeons using such designs should be cognizant of the increased risk of fracture associated with this type of implant.
Classification
A number of classification systems have been proposed to assist in the preoperative analysis and management of these injuries, both early and late. Intraoperative acetabular fractures were classified by Callaghan et al. (18,19) on the basis of in vitro investigation. Their system identified four types of fracture on the basis of the anatomic location: anterior wall, transverse, inferior lip, and posterior wall.
Based on 11 cases, Peterson and Lewallen (5) classified postoperative periprosthetic acetabular fractures into type I with a radiologically and clinically stable acetabular component and type II with an unstable acetabular component.
Della Valle et al. (20) classified acetabular fractures, including both intraoperative and postoperative types. Type I fractures occur intraoperatively at the time of insertion of the acetabular component and are subclassified as type A if they are diagnosed intraoperatively, are undisplaced, and are associated with a stable component; as type B if they are diagnosed intraoperatively but are associated with a displaced fracture; and as type C if they are diagnosed postoperatively. Type II injuries occur at the time of component removal and are further classified as type A if there is <50% loss of acetabular bone stock and as type B if it is greater than 50%.
Our group proposed the following addition to the original Vancouver classification system (VCS) of periprosthetic fractures (21,22), as it applies to the acetabulum intraoperatively (23): Type I—an undisplaced fracture that does not compromise the stability of the component; Type II—an undisplaced fracture that potentially compromises the stability of the reconstruction, such as a transverse fracture of the acetabulum (with pelvic discontinuity or dissociation) or an oblique fracture that separates the anterior column and dome from the posterior column (a much less common injury); and Type III—a displaced fracture. By definition, if there is substantial displacement, the fixation of the cup will be compromised unless the fracture is stabilized. It has been useful in the assessment and management of intraoperative acetabular fractures at our center.
THE UNIFIED CLASSIFICATION SYSTEM
The most recent classification system, which has been applied to the pelvis as a whole, not the acetabulum alone, has been proposed by Duncan and Haddad (24) and endorsed by the AO/OTA Organization. This unified classification system (UCS) is an extension of the VCS (21). It has expanded the VCS to include uncommon but distinct fracture types which are slowly increasing in prevalence, and it applies the principles of diagnosis and treatment to periprosthetic fractures following replacement of the hip (pelvis and femur), knee, ankle, shoulder, elbow, and wrist in a “unified” method, combining the biomechanical features common to all periprosthetic fractures, and emphasizing the influence of a loose implant on fracture union.
With reference to the pelvis, it defines three anatomic regions:
Type A: Fracture of an apophysis: avulsion of the ASIS, AIIS, or ischial tuberosity. This is similar to region A of the femur which includes the trochanteric apophyses (Fig. 87.4).
Type B: Fracture of the acetabulum proper. Subdivided into three types based on implant stability and bone stock. This is similar to type B of the femur.
Type C: Fracture of the ilium and/or rami. This is similar to type C of the femur, distant to the stem (Fig. 87.5).
Type D: Fracture between two arthroplasties (of the pelvis between a bilateral hip replacement).
Type E: Fracture of both the pelvis and femur after hip replacement (Fig. 87.6).

Figure 87.4. Anteroposterior drawing of the pelvis demonstrating fracture lines affecting the ASIS, AIIS, and ischial tuberosity. These are type A.
Type F: Fracture of the acetabulum following hemiarthroplasty (Fig. 87.7).
Similar to the exercise after fracture of the femur following hip replacement in the VCS, the type B is subdivided in the UCS into three types:
B1: Fracture of the acetabular wall or floor which does not affect the stability of the cup and the cup is well fixed (Figs. 87.8 and 87.9).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree