Periprosthetic Femur and Tibia Fractures After Total Knee Arthroplasty
Richard Iorio
Robert Trousdale
William L. Healy
EPIDEMIOLOGY
The population of the United States is projected to increase 33% to 400 million people by 2043. The number of people over the age of 45 is expected to increase 37% to 150 million by 2030, and Americans over the age of 65 will increase 74% to 61 million people by 2025. (1) As the population ages and increases, more patients will develop painful arthritic knees, and the demand for surgical treatment of the knee will continue to increase. In 2005, the number of primary total knee arthroplasty (TKA) procedures reached 523,000, and the number of revision TKA procedures reached 37,000 (2). By 2030, the number of primary TKA procedures is expected to reach 3.48 million annually, an
increase of 565%, and the number of revision TKA procedures is expected to reach 268,000 annually, an increase of 601% (3).
increase of 565%, and the number of revision TKA procedures is expected to reach 268,000 annually, an increase of 601% (3).
Periprosthetic fractures above and below TKA are becoming more prevalent because of the aging population, the increasing number of TKA operations, and the increasing time in situ of the implant. Periprosthetic supracondylar fractures above a TKA occur in 0.3% to 2.5% of patients (4). Periprosthetic tibial fractures associated with TKA occur in 0.39% to 0.5% of patients. Periprosthetic fractures around TKA can occur both intraoperatively and postoperatively. Complication rates associated with the treatment of these injuries have been reported to be as high as 25% to 75% (6). Recognition and appropriate intervention are critical to the successful treatment of these injuries.
Risk factors commonly associated with intraoperative fractures complicating TKA include osteopenia, revision operation, the use of canal fitting, press fit, stemmed components, and inadequate removal of retained cement (7). Risk factors associated with periprosthetic fracture after TKA operation include osteopenic bone, osteolysis, inflammatory arthritis, female gender, increasing age, corticosteroid use, neurologic disorder, previous revision knee surgery, and constrained implants (6, 7, 8).
Minimal trauma can lead to postoperative fractures following TKA. Additionally, major trauma, seizure activity, and the manipulation of a TKA for inadequate motion can also lead to periprosthetic fractures. Anterior notching of the distal femur can be a predisposing factor to periprosthetic TKA fracture in osteopenic bone (4, 5, 6, 7, 8). It has been suggested that violation of the anterior cortex of the distal femur and osteopenic bone can predispose to perioperative fracture, and these deficiencies should be bypassed by a stemmed femoral component to avoid postoperative periprosthetic fractures (4).
PREOPERATIVE CLASSIFICATION AND PLANNING
Several classifications have been developed to aid in the treatment of periprosthetic fractures around TKA. The goal of fracture classification is to develop an algorithm for treatment that is reproducible and easily implemented. The classification system of Lewis and Rorabeck accomplishes these goals (Table 29-1) (9). The system can be applied equally to the femur and tibia. Preoperative planning requires methodical assessment of the fracture pattern, determination of whether the implant is stable or loose, and appraisal of the quality of bone. Ordering of appropriate fixation devices or implants is necessary beforehand to avoid being ill prepared for the challenges of fracture surgery, which are often unpredictable.
Type I fractures are nondisplaced, and the implant is stable. Successful treatment can be operative or nonoperative depending on the patient’s general health, prefracture ambulatory status, bone quality, fracture pattern, fracture stability, and type of implant. Although early motion and prevention of displacement or malunion are advantages of operative intervention with internal fixation, there are patients who may be better served with nonoperative treatment. Patients who may not be able to tolerate anesthesia, surgical blood loss, wound healing, infection, and loss of fixation may be candidates for nonoperative treatment. Nonoperative treatment options include skeletal traction (rarely used), casting, or bracing (4). When surgical intervention is not indicated, the fracture is usually immobilized in extension for 4 to 6 weeks, and weight bearing is protected.
Type II fractures are displaced, and the prosthesis is intact with no evidence of loosening. The goals of treatment are restoration of prefracture alignment, achievement of fracture stability with stable, internal fixation, and the restoration of early motion and function. There are many techniques available to achieve these goals. Advantages of surgical treatment include anatomic (or near anatomic) fracture reduction, early range of motion of the knee, and prevention of late fracture displacement.
TABLE 29-1. Total Knee Arthroplasty Periprosthetic Fracture Classification | ||||||||
|---|---|---|---|---|---|---|---|---|
| ||||||||
Type III fractures may or may not be displaced, but the implant is not stable and requires revision to achieve a functional knee. Bone quality and fracture pattern will determine how the bone stock is restored. If there is missing bone and structural integrity cannot be achieved with internal fixation combined with a revision TKA operation, then additional allograft bone may be necessary or a bonereplacing prosthesis may be used.
SURGICAL TECHNIQUES FOR PERIPROSTHETIC FEMORAL FRACTURES AROUND TKA
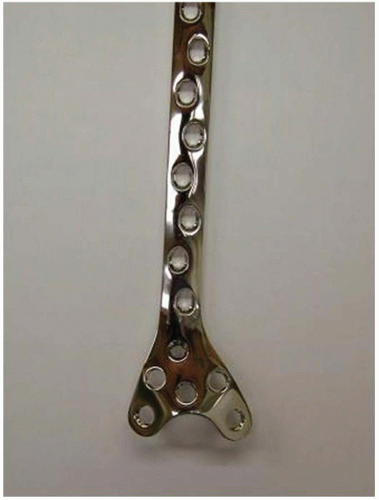
Operative treatment of displaced periprosthetic femur fractures around TKA has been shown to offer the best patient outcome as defined by a well-aligned, well-functioning, stable implant after fracture healing (4,10, 11, 12). There are five surgical treatment options for treating type II fractures including a distal condylar screw and side plate, a 95-degree blade plate, a condylar buttress plate, a locking periarticular plate (i.e., less-invasive stabilization system plating), and a retrograde supracondylar intramedullary nail (Figs. 29-1, 29-2, 29-3 and 29-4). Obstacles to obtaining stable fixation of these fractures include osteopenic bone, fracture comminution, the amount and quality of bone left in the distal condylar fragment attached to the implant, and the design of the femoral component.
FIXED-ANGLE PLATING
Open reduction with plate fixation using a 95-degree blade plate or distal condylar screw and side plate has provided predictable fixation when treating these fractures. It is imperative that radiographs identify the degree of comminution and any intercondylar extension of the fracture. Multiple oblique views of the distal femur along with true anterior-posterior and lateral projections are a must. Three-dimensional reconstructions of these injuries on computed tomography scan may be helpful in delineating fracture lines obscured by the implant. Depending on the geometry of the distal fragment and the quality of bone, stable fracture fixation can be obtained, which allows early motion and restoration of knee function. In severely osteopenic bone, polymethylmethacrylate or allograft bone can be used to augment fixation in the distal condylar fragment.
At times, the distal condylar fragment is too small to accommodate a distal condylar screw and side plate. A blade plate will preserve distal bone for fixation (Figs. 29-5, 29-6 and 29-7). If intercondylar extension is present, adjunct fixation with large screws can be added adjacent to the blade and may be placed prior to the seating chisel to prevent further fracture displacement. Orthogonal, anterior-posterior screws can provide a second plane of fixation to increase stability. Should fixation with the blade plate fail to provide a stable construct, then the distal condylar screw and side plate can be used if there is sufficient distal bone, or adjunctive polymethylmethacrylate can be added.
Advantages of traditional plate fixation include stable internal fixation and the restoration of alignment. Disadvantages of traditional distal plate fixation include the need for extensive soft tissue dissection and fracture exposure, potential loss of distal fixation, and varus collapse and difficulty with some posterior stabilized knee implant designs. The presence of the box that accommodates the post in a posterior stabilized knee design may limit the amount of bone available for distal fixation with plates. Measurement of construct stiffness has shown that the distal condylar screw, side plate, and the blade plate were more rigid than the condylar buttress plate for supracondylar fracture above TKA (13).
 FIGURE 29-5 Supracondylar periprosthetic femur fracture above a posterior cruciate-retaining implant. |
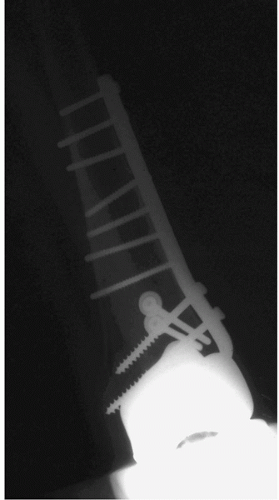 FIGURE 29-6 Anterior/posterior radiographs of a 95-degree angled blade plate fixing a supracondylar femur fracture. |
RETROGRADE SUPRACONDYLAR INTRAMEDULLARY NAIL
Intramedullary retrograde supracondylar femoral nails have been used to treat periprosthetic distal femur fractures. Retrograde nailing is an attractive concept because of limited soft tissue dissection and exposure and a theoretically rigid construct. If there is a sufficient distal fragment to allow two rigid distal interlocking screws (generally 2 to 3 cm of distal bone above the prosthesis), then a retrograde supracondylar intramedullary nail can be used. These retrograde nails can be placed through a relatively small medial parapatellar arthrotomy, if there is a posterior cruciate-retaining implant in place (Figs. 29-8 and 29-9). Most cruciate-retaining knee designs can accommodate rod diameters from 11 to 20 mm (4,6, 7, 8,11). Some cruciate-substituting designs have boxes with holes that allow access to the femoral canal. These holes can be opened and will allow small 8- to 10-mm nail diameters to pass. If the box is solid or the opening is too small to accommodate the nail, a diamondtip burr can be used to open the box. This approach generates a lot of metal debris, however, and may compromise the intra-articular integrity of the arthroplasty if care is not taken to remove all of the debris (4,6, 7, 8,11,14).
Disadvantages of retrograde intramedullary supracondylar femoral fixation include the limits of distal fixation if the distal fragment is not large enough to accommodate two rigid locking screws and the difficulties encountered with posterior-substituting designs. Additionally, controlling alignment with intramedullary fixation is difficult because of the limitation and sizes of the supracondylar nails as well as the large variability in the positions of the distal fragment in reference to the nail. Nonunion, locking-screw loosening, nail migration, valgus drift, and decreased range of motion are all reported complications. Although the union rate is high, maintenance of acceptable alignment can be difficult. Retrograde intramedullary supracondylar rod fixation should be reserved for fractures with 2 to 3 cm of bone above the prosthesis, relatively good distal bone stock that allows rigid fixation of at least two distal locking screws, and minimal proximal comminution to allow maintenance of alignment with a good diaphyseal fit (11,15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree