Peripheral Neuropathy
Philip Dean Zaneteas
Injuries to the peripheral nervous system remain an important area of pathology for the sports medicine physician. It may be difficult to diagnose these lesions and even more difficult to fully delineate their severity and type. Electromyography (EMG) remains the singular procedure for diagnosing neurological injuries. The following discussion, involving brachial plexus injury as well as trauma to its peripheral nerve branches, will proceed with this notion in mind.
Brachial Plexus Injuries
The brachial plexus is vulnerable to injury from a number of etiologies. The clinical manifestations additionally can be protean. Delineating the correct diagnosis, the degree of severity and the optimal treatment are dependant upon detailed knowledge of the neuroanatomy of the region as well as a comprehensive electrodiagnostic examination (EMG). Care must be taken to distinguish between a brachial plexus lesion (which may affect more than one portion of the plexus), a cervical radiculopathy, or a peripheral nerve injury. Often, this is difficult in that the clinical presentation may be similar or identical. The task, although difficult, is crucial as the treatment and ultimate prognosis remain dependant on this distinction.
Brachial Plexus—Anatomy (C5-8, T1)
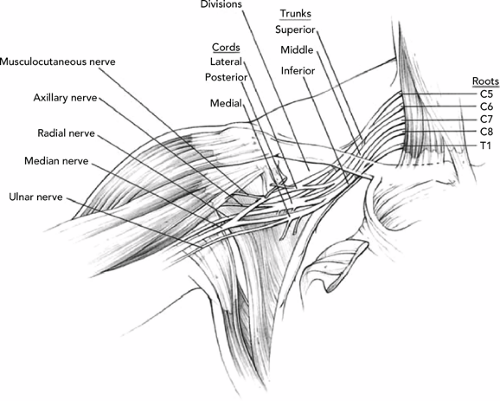
The brachial plexus is initially formed by the ventral or anterior primary rami of C5-T1. The anterior rami of the C5–6 roots join to form the upper trunk. The anterior ramus from C7 becomes the middle trunk. The anterior rami from C8 and T1 join to form the lower trunk. Anatomical variants may occur with contributions from C2–4 and T2 (i.e., prefixed and postfixed plexuses correspondingly). At the clavicle, the trunks bifurcate into their anterior and posterior divisions. The anterior divisions of the upper and middle trunk coalesce to form the lateral cord. The medial cord is formed by the anterior component of the lower trunk. The posterior divisions of all three trunks form the posterior cord. The cords themselves extend from the midpoint of the clavicle to the inferomedial portion of the coracoid process of the scapula. At this point, the cords give rise to their respective peripheral nerve branches (see Figure 15.1).
From the standpoint of clinical conceptualization of brachial plexus injuries, one approach is to separate injuries as occurring either proximal or distal to the clavicle. Supraclavicular and infraclavicular injuries often have different biomechanical mechanisms of injury with different prognoses. Within this paradigm, the electromyographer-sports medicine physician can expect characteristic electrodiagnostic findings, specific and typical of the site of injury.
Mechanisms of Injury
Mechanisms of injury to the brachial plexus include blunt and penetrating trauma, traction injuries, compression, and inflammatory/autoimmune (e.g., Parsonage-Turner syndrome/brachial plexitis) conditions. Nerve injury classification systems continue to be delineated in the electrodiagnostic literature. For our purposes, three general categories of nerve injury can be cited. Neuropraxic injuries are consistent with demyelination of the axon sheath. The axon itself remains intact. Conduction block may occur at the site of injury. Nerve repair occurs with remyelination. Axonotmesis is characterized by trauma to the axon itself along with the myelin sheath. Wallerian degeneration occurs in variable degrees depending on the severity of the injury. An intact epineurium implies the capacity for nerve regeneration. Electrodiagnostic findings on needle examination are notable for the presence of spontaneous axonal loss findings in the form of fibrillation potentials and positive sharp waves. Moreover, motor unit dropout may occur with decreased motor unit recruitment characterized by large amplitude, increased duration motor units. Neurotmesis occurs with more serious nerve injuries
where the endoneurium is disrupted. The nerve and its fibrous sheath are transected, rendering axonal regeneration unlikely. Denervation patterns on electrodiagnostic examination predominate.
where the endoneurium is disrupted. The nerve and its fibrous sheath are transected, rendering axonal regeneration unlikely. Denervation patterns on electrodiagnostic examination predominate.
Physical Examination
Observation of the patient’s anatomy at rest should focus on the shoulder girdle musculature as well as the distal upper extremities to discern the presence or absence of atrophy, skeletal deformity, scapular winging, and posture (see Table 15.1). Palpation of the patient should include regions of discomfort to assess for fracture, masses, swelling, and possible signs of inflammation. Range of motion, both actively and passively in all of the upper extremity joints including the cervical spine, may reveal evidence of contractures (both fixed and variable), spasticity, and instability. The motor-sensory examination may also help differentiate between root, trunk, cord, and peripheral nerve lesions. Finally, the examination of reflexes and upper motor neuron testing should be included.
Specific Brachial Plexus Injuries
The “Burner/Stinger” Syndrome
The burner/stinger syndrome represents a trauma-induced symptom complex involving the shoulder girdle region. It is generally characterized by a sharp, burning pain radiating from the supraclavicular region extending distally down the arm. It is associated with generalized paresthesias and/or anesthesia (nondermatomal) that tend to resolve within minutes. Shoulder girdle motor weakness may subsequently develop either immediately or within a few days. Associated signs and symptoms include muscle spasm and neck pain. In severe brachial plexus injuries of this type, the athlete (commonly a linebacker or defensive back in football) will come off the field holding his involved upper extremity in an internally rotated, adducted position.
The physical examination of the patient should include a detailed neuromuscular examination not only of the shoulder girdle region (i.e., all three heads of the deltoid, supraspinatus, infraspinatus, rhomboids, teres major/minor) but also of the cervical spine, the serratus anterior (scapular “winging” must be ruled out), and the more distal musculature of the upper extremity (e.g., those muscles innervated by the radial, median and ulnar nerves). It is important to note that motor testing immediately after the injury may be normal or minimally compromised. For this reason, given the potential of evolving neurological pathology, the athlete should be followed up closely over the following 2 to 3 weeks to determine if there are any residual motor or sensory deficits. Within this context, the delineation of the baseline motor-sensory status is
fundamental as a reference point to the later neuromuscular examinations.
fundamental as a reference point to the later neuromuscular examinations.
TABLE 15.1 Upper Extremity Motor Innervation: Root, Trunk, and Cord Localization | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Localization of the site of injury may be related to the mechanism of injury. Supraclavicular injuries tend to be secondary to traction mechanisms with involvement at both root and trunk levels. The upper and middle trunks tend to be more commonly involved. Infraclavicular injuries tend to be secondary to shoulder abduction/extension biomechanics, which involve cords and terminal nerves generally, and the posterior cord and axillary nerve more specifically. In both types of injury, the suprascapular nerve is commonly involved. In such instances, the athletes develop weakness in shoulder abduction initiation (supraspinatus involvement) as well as shoulder external rotation (infraspinatus involvement). Distal peripheral nerves may also be involved at their origins including the musculocutaneous, radial, median, and ulnar nerves. With musculocutaneous nerve involvement, weakness of the biceps occurs with elbow flexion with the forearm fully supinated. Weakness of the brachialis may be tested with the forearm fully pronated. Both the biceps and the brachialis are innervated by the musculocutaneous nerve and testing of elbow flexion should be performed not only with the forearm fully supinated and pronated as described earlier but also in “neutral” in order to test the brachioradialis, which is innervated by the radial nerve. The physical examination, therefore, is an important precursor to the electrodiagnostic examination in performing a preliminary delineation of areas of weakness and involvement in the injured upper extremity.
From the standpoint of further evaluation of brachial plexus “stinger/burner” injuries, the sports medicine physician should always be cognizant of the differential diagnoses in such a clinical milieu.
Simultaneous injuries to adjacent or contiguous neuromuscular structures should be entertained when clinically indicated. The more common differential diagnostic concerns in the “burner/stinger” syndrome include cervical spine injury as well as potential shoulder, clavicular, and scapular bony trauma. For this reason, radiographic studies of all of these regions may be clinically indicated. From a neurological standpoint, it is important to remember in cases where there is any question of cervical spine instability or spinal cord trauma, continued radiographic workup is clearly indicated. Initially, a standard cervical radiographic series including anteroposterior (AP, including open mouth view), lateral, and oblique views may be obtained. If the findings are normal and the athlete is neurologically intact, flexion–extension lateral views may be obtained if there is a question of instability.
In the presence of symptoms and physical examination findings suggesting a cervical radiculopathy, magnetic resonance imaging (MRI) of the cervical spine may be considered. Bony lesions such as fractures are better demonstrated by cervical computed tomography (CT). Although uncommon, one must also be alert to any symptoms or findings that may suggest bony trauma to the shoulder girdle region (including the clavicle, glenohumeral joint, and scapula). Radiographic evaluation is generally sufficient to rule out any bony abnormalities. Finally, in severe shoulder girdle injuries of which the “singer/burner” presentation may be just one component, the possibility of a rotator cuff tear (full or partial thickness) may be ruled out by means of an MRI study.
In considering the neurophysiological status of the patient, an electrodiagnostic examination may be necessary to further delineate the extent and severity of the athlete’s neurological injury. The electrodiagnostic and sports medicine literature historically has debated the relative distinctions concerning potential trauma at the cervical root, trunk, cord, and peripheral nerve levels. At this time, the only means to evaluate the neurophysiology of the brachial plexus and its cervical root origins is EMG. Acute, traumatic brachial plexus injuries (burners/stingers) may have several potential biomechanical causes involving different levels of the neuroaxis in the neck and upper extremity. To delineate this pathology physiologically, the patient must be studied with an EMG examination. The term “burner/stinger” has probably caused more confusion and uncertainty in both diagnosis and treatment in that it remains nonspecific. Clinically, what exists rather is a varied spectrum of potential pathology that has been classified as the “stinger syndrome.” An alternative approach would be to incorporate the use of a paradigm utilizing the following differential diagnoses: spinal cord contusion, cervical radiculopathy, trunk/cord (brachial plexus) injury, peripheral nerve injury, or any combination of the above. Any of the above lesions may exist either singly or in some combination. The clinical imperative does not exist that would require that they exist in a mutually exclusive presentation.
An important point for the clinician to remember is to distinguish between a spinal cord injury and root injury as well as between an intraspinal and extraspinal injury. Chronic root scarring (especially at C5, C6) along with compression by musculature (e.g., scalene muscle compression) can result in repetitive numbness/weakness. Distinguishing between preganglionic and postganglionic lesions at the root level is also important in that the prognosis can be significantly different. What exists then is an “extraspinal nerve injury syndrome” that may occur anywhere from the cervical roots (either pre or postganglionic) to the trunk or possibly at the cord level of the brachial plexus. In attempting to simplify the “stinger phenomenon,” the diagnostic waters have been muddied by attributing the “stinger” to a single etiology.
Return to Play
There remains the issue of return to activity. First, a clear diagnosis must be made electrodiagnostically distinguishing the presumed from the actual site of the lesion(s). Second, EMG findings may remain abnormal for years with findings consistent with residual, chronic axonal loss and demyelinative pathology. This should not remain the determining criterion for return to play or activity as some have argued. Rather, the electrodiagnostic findings should be utilized in the overall evaluation of the patient once a comprehensive rehabilitation program has been utilized. Recommendations in the sports medicine literature urge the development of relative symmetry in both strength and flexibility parameters with symptom-free status before returning to play or activity. Finally, variables that would seem to predispose the athlete to injuries of this type should be targeted and addressed, such as improper biomechanics specific to the sport, relative muscle and flexibility imbalances, and return to play before sufficient healing occurs. Athletes who complain of repeated episodes of “burning” or paresthesias appear to be at particular risk and probably should be withheld temporarily from active participation in contact sports. In this capacity, the sports medicine physician performs a preventative role in avoiding further nerve injury while rehabilitation continues.
Suprascapular Nerve Injury
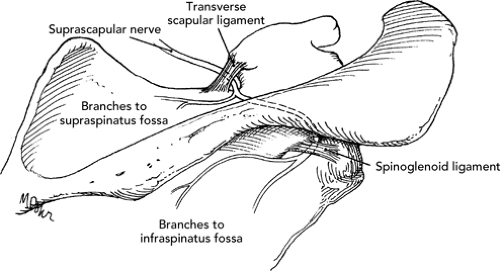
The suprascapular nerve originates from the upper trunk with C5–6 (C4) root innervation. It is relatively susceptible to injury during its course (see Figure 15.2). It crosses the posterior triangle of the neck to the superior border of the scapula where it passes through the suprascapular notch and supplies the supraspinatus. It then passes around the spinoglenoid notch and terminates in the infraspinatus. Sensory branches innervate the posterior capsule of the glenohumeral joint and the acromioclavicular joint.
Suprascapular neuropathies may have a variable presentation depending on the location of injury along the course of the nerve as well as the inciting type of pathology. Traumatic injuries secondary to fractures of the scapula or blunt trauma rarely result in significant nerve damage. In contrast, compression injuries either at the suprascapular notch or the spinoglenoid notch have been well documented in the literature. Compression may occur secondary to ligamentous structures, callus formation, ganglions, or ossified bone. Traction injuries either secondary to athletic biomechanics or traumatic mechanisms are also possible etiologies. Additionally, the suprascapular nerve is commonly involved in patients experiencing acute brachial plexitis (Parsonage-Turner syndrome), but this exists as a generalized neuropathic condition with an autoimmune etiology, which can simultaneously involve multiple peripheral nerve branches as well as the supplying roots of the brachial plexus.
The clinical presentation of suprascapular neuropathy includes poorly localized pain in the shoulder girdle region, weakness in shoulder abduction initiation, as well as external rotation with intact sensation. Physical examination can reveal atrophy in both the supraspinatus and infraspinatus. If deltoid function is found to be abnormal, a more generalized process is likely. Electrodiagnostic evaluation is necessary to delineate the level, degree, and type of suprascapular nerve injury. The EMG needle examination is utilized to determine whether spontaneous axonal loss pathology is present. Motor unit recruitment should be assessed to rule out the possibility of a “neurogenic” (decreased) motor unit recruitment pattern secondary to motor unit dropout. Side-to-side suprascapular
motor nerve conduction studies with pickups on both the supraspinatus and infraspinatus can be of benefit in determining the presence of demyelination in the form of conduction block. When present, this would result in relatively lower motor amplitudes on the affected side. This in turn gives the clinician an approximate value of the percentage of elicitable motor units innervated by the involved suprascapular nerve. Within this electrodiagnostic and clinical context, it is important to remember that traction injuries involving the suprascapular nerve tend to occur at the nerve’s origin (Erb’s point), whereas kinking and compression of the nerve can occur both at the suprascapular notch as well as the spinoglenoid notch (an MRI of the spinoglenoid notch may reveal a surgically amenable ganglion cyst).
motor nerve conduction studies with pickups on both the supraspinatus and infraspinatus can be of benefit in determining the presence of demyelination in the form of conduction block. When present, this would result in relatively lower motor amplitudes on the affected side. This in turn gives the clinician an approximate value of the percentage of elicitable motor units innervated by the involved suprascapular nerve. Within this electrodiagnostic and clinical context, it is important to remember that traction injuries involving the suprascapular nerve tend to occur at the nerve’s origin (Erb’s point), whereas kinking and compression of the nerve can occur both at the suprascapular notch as well as the spinoglenoid notch (an MRI of the spinoglenoid notch may reveal a surgically amenable ganglion cyst).
Treatment options include conservative management, analgesics (both oral NSAIDs as well as a short course of a steroid taper), a comprehensive shoulder girdle rehabilitation program that focuses on strengthening and biomechanics, as well as correction of any sport/activity-specific biomechanical errors in technique utilizing the upper extremity. Surgical exploration and decompression of any compressive lesions may be required in more severe injuries.
Thoracic Outlet Syndrome
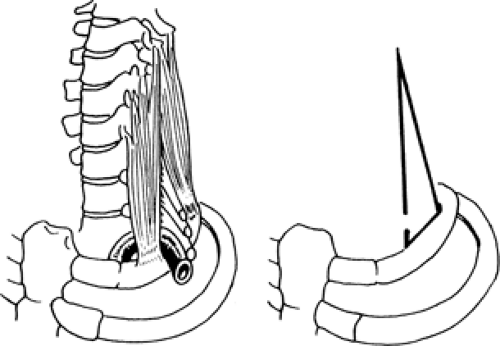
“Thoracic outlet syndrome” (TOS) (see Figure 15.3) refers to a symptom complex that occurs secondary to compression of the subclavian blood vessels (“vascular” TOS) as well as the brachial plexus (“neurogenic” TOS), although involvement of the former is exponentially much greater than the latter. TOS has been characterized as a neurovascular phenomenon in the surgical literature although its neurogenic form is rarely confirmed electrodiagnostically. Symptom presentation can be quite variable depending upon the neurological structures traumatized. Involvement of the lower trunk (C8-T1) of the brachial plexus can mimic carpal tunnel syndrome (CTS) with regard to weakness in the abductor pollicis brevis (APB). The patient may complain of pain or paresthesias along the medial aspect of the arm and ulnar aspect of the forearm. Symptoms can extend into the fourth and fifth digits with a decrease in intrinsic muscle strength. Upper trunk (C5-6) involvement is less frequent (unlike “acute brachial plexitis”—Parsonage-Turner syndrome). In this instance, shoulder girdle complaints may occur circumferentially (the differential diagnosis should also include C5 and/or C6 radiculopathies). Vascular compression may include venous obstruction (characterized by upper extremity edema, cyanosis with potential collateralization to the shoulder and thorax) as well as arterial obstruction (typified by numbness diffusely, coolness to touch, decreased pulses, and exertional fatigue).
Etiologies of TOS include congenital and structural anomalies (e.g., cervical ribs, fibrous bands, anomalous fibrous bands in the scalene musculature), trauma, dysfunctional upper extremity, and shoulder biomechanics that may all cause narrowing of the costoclavicular outlet. Potential sites of compression include the interscalene triangle (where the brachial plexus and subclavian artery
pass between the anterior and middle scalene muscles and over the first rib), the costoclavicular outlet, and proximal to the axilla (compression under the pectoralis minor insertion on the coracoid process, which may occur in hyperabduction activities, e.g., swimming, throwing, and the tennis serve).
pass between the anterior and middle scalene muscles and over the first rib), the costoclavicular outlet, and proximal to the axilla (compression under the pectoralis minor insertion on the coracoid process, which may occur in hyperabduction activities, e.g., swimming, throwing, and the tennis serve).
From a diagnostic standpoint, classic tests on physical examination have been shown to be equivocal at best with a high rate of false positives (e.g., Adson’s test, Wright’s maneuver, overhead exercise test). Radiographs of the cervical spine and medial clavicle may rule out a cervical rib as a potential etiology. Electrodiagnostic evaluation remains the centerpiece to evaluation of the “neurogenic” form of TOS. The amplitude of the compound motor action potential (CMAP) of the median nerve is the parameter most commonly affected. The ulnar sensory nerve action potential (SNAP) is less than 10 uV in 50% of patients. Needle examination most often reveals findings localized to the lower trunk musculature (especially the APB and first dorsal interosseous). A detailed needle study is required to rule out other pathologies such as distal entrapment neuropathies and cervical radiculopathy. Most patients referred for evaluation of possible TOS that manifest abnormal findings on EMG turn out to have CTS. With regard to “vascular” TOS, a venogram and/or arteriogram are generally required to determine the presence of venous obstruction, aneurysms, or regions of arterial insufficiency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree