Head and Neck
Scott H. Grindel
Injuries to the head, face and neck in athletics are relatively common and the leading cause of morbidity and mortality in athletes. Approximately 12% of all craniomaxillofacial injuries seen in trauma centers are attributable to sports participation (36). Since 1945, a total of 497 deaths have been attributed to football in the United States, 69% of which were due to brain injury and 19% due to spinal cord injuries (26). Significant declines in the severity and incidence of head injuries were seen from 1983 to 1999 (19% and 4%, respectively) thought to be due to improved helmet design and rule changes (25). These statistics are testimony of our constant vigilance of these injuries, use of current treatment recommendations, and continued epidemiological monitoring concerning the need for improved equipment, and changes in or increased enforcement of the rules of play.
Section A Head Injuries
Head injuries, and the fear of them, remain one of the most powerful motivating forces for policy changes in sports. Advances in the technology of protective equipment improved the safety of sports, but may have instilled a degree of invincibility in some athletes. For instance, as shown in Table 24A.1, a significant increase in severe head and neck injuries seen in football in the 1970s sharply declined after the institution of rules outlawing “spearing” (35). Present studies estimate that 17,008 head injuries present to the emergency room per year due to hockey (rates 7–13:10,000 participants), 86,697 due to soccer (rates 6–10:10,000 participants), and 204,802 due to football (rates 9–14:10,000 participants). Concussion, skull fracture, and intracranial injuries due to hockey account for 9,883 of these visits (rates 4–9:10,000 participants), 50,035 due to soccer (rates 3–7:10,000 participants), and 128,968 due to football (rates 5–10:10,000 participants) (15).
Head injury includes trauma to the scalp, soft tissue, bone, or brain. These injuries are typically classified to reflect their acute and long-term clinical significance. Severe head injuries are those with obvious potential for chronic neurological damage or death. Mild head injuries are those that involve the soft tissue and bone of the head (excluding cranial vault fractures) and clinically reversible brain damage. On the basis of the potential for infection and injury severity, injuries may also be classified as open or closed head injuries. See Table 24A.2 for an outline. This chapter will deal primarily with injuries to the head, face, and neck; brain injuries are covered more thoroughly in other chapters in this book.
TABLE 24A.1 Mortality Rates Due to Football Head and Neck Injuries for 1977-1986 Presented in Incidence Per 100,000 Participants | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
TABLE 24A.2 Organizational Outline for Head Injuries | |||
|---|---|---|---|
|
Anatomy
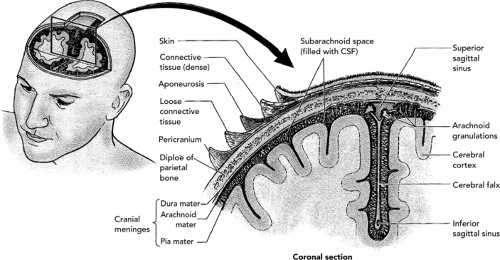
There are five distinct layers of the scalp (see Figure 24.1):
Epidermis and dermis. They are the most superficial layers of the scalp. The scalp is a common area for lacerations in sports not requiring a helmet and are often seen in some helmeted sports (i.e., ice hockey).
Superficial fascia. It contains an extracranial blood supply from the external carotid artery. There is no arterial supply from the bone to nourish the scalp. The venous system of the scalp, however, communicates with the cavernous, superior, sagittal, and lateral sinuses of the brain. As a result, scalp infections can potentially spread intracranially by means of the venous system.
Galea aponeurotica. It is a tough, dense layer of fibrous tissue separating the superficial layers of the scalp from the skull.
Subaponeurotic layer.
Pericranium. It acts as the periosteum or glia of the skull.
The skull consists of a bony vault made up of eight bones tightly joined at the suture lines. There are two parietal and temporal segments, and a single occipital, frontal, ethmoid, and sphenoid segment. The four distinct tissue layers between the skull and the brain are as follows (see Figure 24.1):
Epidural space. In actuality a potential space between the skull and the dura mater. Epidural hematomas develop in this tissue plane.
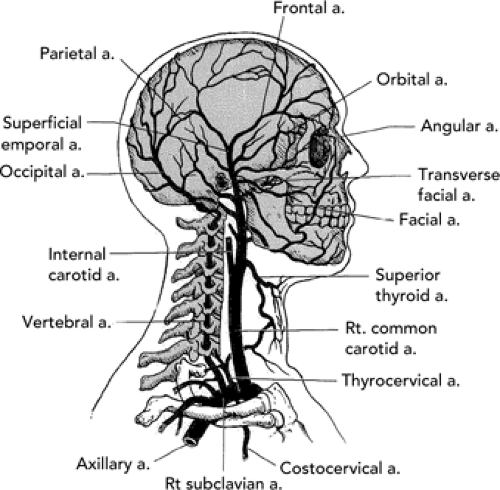
Dura mater. It contains the venous sinuses and three meningeal arteries and veins. This is the location of the middle meningeal artery, a terminal branch of the external carotid. Injury to this artery is the most frequent mechanism of epidural hematomas (see Figure 24.2).
Arachnoid. It is a narrow space between the dura and the pia mater containing the spinal fluid of the brain. Subdural hematomas can develop here following intracranial venous lacerations.
Pia mater. It is a layer closely adherent to the cerebral cortex and the site of potential subarachnoid hema- tomas.
The brain itself is unique because it is a fixed volume enclosed in a nonexpandable vault (the skull and dura mater). A significant increase in its mass (edema, hematomas, etc.) leads to an increase in intracranial pressure. This often leads to injury or death due to compression of brain tissue against bony prominences and herniation through the foramen magnum, neither of which is a welcome occurrence in the sports arena.
The brain is supplied by two arterial sources, the internal carotids anteriorly, and the vertebral arteries posteriorly. These two arterial sources reconnect within the cranial vault at the circle of Willis thereby providing some redundancy to protect from ischemia due to stroke or injury. The face and scalp are supplied by the external carotids, an important branch of which is the middle meningeal artery. Injury to the middle meningeal artery can result in significant intracranial bleeds. See Figure 24.2 for details of the blood supply to the head and neck.
Mechanisms of Head Injury
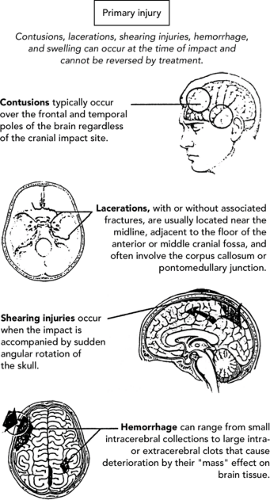
Any blow to the head can cause brain injury. Concussion and minor brain contusion have also been associated with blows to the body. In either case, injury is often due to the resultant sudden head movement and shifting of the brain within the skull. This is particularly true with rotational movements of the brain, which cause shearing forces and rotation of the brain over irregularities on the inner skull. This explains why many injuries involve brain tissue overlying the frontal lobe, temporal lobe, and the base of the brain. Even minor impacts can cause tearing of small vessels and the formation of petecchiae (38). Following a concussion, there may be a reduction in the brain’s ability to process information, which typically resolves within 5 to 7 days (1,13,28). As the number of past concussions grows, the more severe the concussions can become, often taking
only minor impacts to cause severe concussions. Repeated concussions may also lead to permanent damage and long-term symptoms. If a second concussion occurs before the first has resolved, massive swelling of the brain can occur resulting in death. This is the so-called “second impact syndrome” or “diffuse brain edema” (9).
only minor impacts to cause severe concussions. Repeated concussions may also lead to permanent damage and long-term symptoms. If a second concussion occurs before the first has resolved, massive swelling of the brain can occur resulting in death. This is the so-called “second impact syndrome” or “diffuse brain edema” (9).
Direct Injuries
Brain injury occurs most often by direct trauma to the head. This can occur with a moving object striking the head such as seen in boxing, baseball, field hockey, or ice hockey. These injuries typically cause damage at the site of impact or a “coup injury”. More often, injury occurs when a moving head impacts a fixed or slow moving object such as the turf, an opposing player, or a goal post as with football or hockey. This mechanism often results in injury on the opposite side of the brain as the impact referred to as a countercoup injury.
Indirect Injuries
Traumatic impact to another body part can be transferred to the cranium. For example, a fall on the coccyx while ice-skating can lead to an injury at the base of the brain. Impacts to the periphery that lead to a rotational force to the brain, such as a head-on check to the lateral shoulder as seen in ice hockey, can lead to concussions, contusions and hematomas of the brain, as well as neck injuries.
Biomechanics
The location and degree of head injury depends on the position of the head at the moment of impact, the magnitude and direction of impact, and the structural
features and integrity of the skull. It is the response to the force rather than the force alone, which causes these injuries (41). See Figure 24.3 for a delineation of the types of primary head injuries.
features and integrity of the skull. It is the response to the force rather than the force alone, which causes these injuries (41). See Figure 24.3 for a delineation of the types of primary head injuries.
Scalp Injuries
Lacerations
Lacerations should be treated as outlined elsewhere in this book; however, the increased vascularity of the superficial layer of the scalp make these lacerations prone to continued bleeding, in many cases hampering appropriate wound closure. Venous connections to intracranial structures heighten the concern for infections. Repair should be done under sterile conditions, after copious irrigation and shaving where necessary to clear the field (except the eye brow). Staples can be a quick repair in the heat of an event, but do not neglect to irrigate the wound and evaluate the athlete for brain or neck injury. Use prophylactic antibiotics in all human bite wounds. Double coverage is recommended such as amoxicillin/clavulanate 825/125 mg PO b.i.d. (pediatric patients use 22.5 mg/kg PO b.i.d.), or ciprofloxacin 500 mg PO b.i.d. (pediatric patients use TMP/SMX 5 mL suspension/10 kg PO b.i.d.), and clindamycin 125 mg PO q.i.d. (pediatric patients use 5 mg/kg PO q.i.d.) for 5 days. Testing protocols for hepatitis and HIV should be strongly considered in both individuals involved.
Subglial Hematoma
Blunt injury commonly causes blood to collect between the glia and the skull, sometimes called a goose egg. Initial treatment involves the application of ice as well as a skull x-ray to rule out fracture. If there is no skull fracture, pressure and ice over the area may minimize the size of the hematoma. Careful follow-up should take place to monitor for infection or neurological changes. Again, evaluating the patient for brain or neck injury should not be neglected.
Skull Fractures
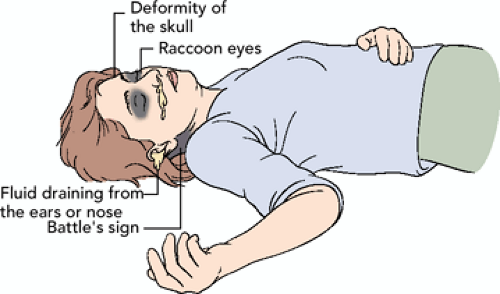
Skull fractures may be open or closed. Because the force of the blow may actually be absorbed during the fracturing process, the resultant intracranial damage may actually be lessened. Fracture lines crossing the grooves of meningeal arteries, particularly the middle meningeal arteries, should arouse suspicion for epidural hematoma. Battle’s sign (ecchymosis behind the ear) and “raccoon eyes” (ecchymosis under the eye[s]) may be the result of a basilar skull fracture (see Figure 24.4). Hemotympanum (see Figure 24.5) or cerebrospinal fluid (CSF) leaking
from the nose or ears (CSF rhinorrhea/otorrhea) may also be a clue to this type of fracture. In a mixture of CSF and blood, CSF separates when placed on filter paper and forms a characteristic “double ring sign” or “halo sign.” Although this test is sensitive, false positives are possible.
from the nose or ears (CSF rhinorrhea/otorrhea) may also be a clue to this type of fracture. In a mixture of CSF and blood, CSF separates when placed on filter paper and forms a characteristic “double ring sign” or “halo sign.” Although this test is sensitive, false positives are possible.
Skull Fracture Classification
Linear-hairline separation fractures may cause loss of the curvature of the skull. These are typically produced by blunt impact and represent 70% of all skull fractures.
Comminuted fractures typically entail a small impact area causing indentation and fragmentation of the underlying bone.
Depressed-skull fractures are displaced inwardly, the depression increasing with the pointedness of the object (baseball vs. javelin). Complications may arise if the fracture has entrapped brain or meninges or if an intracranial hematoma develops.
Blowout fractures of the orbit are caused by direct blunt impact to the floor or roof of the orbit or the eye itself. This may entrap the inferior or superior oblique muscle causing loss of extraoccular movements. See section on Eye Injuries in this chapter.
TABLE 24A.3 Observations on Examination That Would Suggest That Further Workup with Plain Film, Computed Tomography, or Magnetic Resonance Imaging may be Necessary | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
See Table 24A.3 for observations supporting radiological workup for skull fracture.
Brain Injury
The best way to prevent the sequelae of serious head injury is to be prepared for it and diagnose it rapidly. The team physician should carry the necessary supplies or have them at the event site. See Appendix 24.1 for a checklist. In determining the seriousness of the injury, a brief neurological examination and a tentative diagnosis should be made. The neurological examination should include an assessment as outlined in Table 24A.4 and in Appendix 24.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree