Knee Injuries
E. James Swenson Jr.
The most often injured joint in sports participation is the knee (1,2,3,4,5,6,7,8,9,10). The keys to diagnosis and management are the following: (a) knowledge of the functional anatomy, (b) understanding the mechanisms of injury in traumatic events, (c) identifying training errors in overuse injuries, (d) familiarity with the more common knee injuries in sport, (e) knowledge of previous injury and rehabilitation of either knee, (f) a precise, thorough physical examination and (g) a meticulous and accurate evidence-based differential diagnosis.
This chapter begins with the diagnosis and management of traumatic and atraumatic knee emergencies. Sections on anatomy, history taking skills, physical examination skills, radiographic evaluation, and technique for aspiration/injection follow. The diagnosis and management of common traumatic and overuse injuries completes the chapter (see Table 31.1 for abbreviations used throughout this chapter).
Emergencies
Traumatic
Acute Knee Dislocation
This injury is uncommon, but with the potential for catastrophic consequences including loss of limb or limb function (11). An acute knee dislocation involves a complete separation of the femoral condyles from the tibial plateau with associated disruption of most of the knee ligaments that results in global laxity of the joint. The condition may present “dislocated” on the field or a spontaneous reduction may occur. An anterior dislocation is most common (40%) followed by posterior dislocation (33%). The most common mechanism for anterior knee dislocation is forced hyperextension. Associated vascular and neurological injury can occur and must be documented. The popliteal artery can be damaged by traction or direct trauma and occurs in up to 40% of injuries. The incidence of neurological injury is reported to be 16% to 40%. The peroneal nerve is more commonly injured than the posterior tibial nerve.
The role of the team physician is to appreciate the severity of the injury. If the injury is evaluated on the field, an anterior dislocation will present with a very prominent tibial plateau. The tibia may be rotated but the patella/patellar tendon will be in line with the tibial shaft in contrast to a frank patellar dislocation where the tibiofemoral joint is aligned but the patella is laterally displaced. In a posterior dislocation the patella is dislocated laterally and the tibia posteriorly, with the femoral condyles very prominent. To limit excessive, prolonged traction on the neurovascular structures, a reduction should be attempted. Reduction for an anterior dislocation is accomplished by gentle traction coupled with extension of the knee when a single “clunk” will be felt. A posterior dislocation is reduced by applying a gentle traction coupled with an “anterior drawer force” as the knee is gently extended. The first “clunk” will be the reduction of the tibiofemoral joint and the second “clunk” occurs with the reduction of the patellar into the femoral trochlea (groove). A displaced meniscus may prevent reduction of a knee dislocation (19). Vascular and neurological function must be evaluated and noted followed by immediate transfer for appropriate consultation. The orthopedic and vascular surgeon’s consultants will utilize imaging studies to document damage to capsule/ligaments (magnetic resonance imaging [MRI]) and vessels (magnetic resonance angiography [MRA] or arteriogram). To avoid confusion following the spontaneous reduction of a frank patellar dislocation, the examiner may note the presence of an immediate effusion, negative Lachman, negative collateral ligament testing but positive for a tender medial retinaculum coupled with a positive apprehension sign.
TABLE 31.1 Abbreviations Used Throughout This Chapter | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Nontraumatic
Septic Arthritis (20)
Clinical Features
Pyogenic arthritis is characterized by an atraumatic severe joint pain, with limited range of motion (ROM) and a warm, swollen and markedly tender joint. A septic joint may present without warmth and only a minor effusion early in the course. Involvement is most often monoarticular but can involve more than one joint. The most commonly involved joint is the knee followed by the hip. In the initial 24 to 72 hours there may be no systemic manifestations. Eventually, systemic signs include fever, chills and an elevated white blood cell (WBC) count. Septic arthritis most often results from direct hematogenous seeding of the synovium. An extra-articular focus of infection can be identified approximately 25% of the time and is useful in deciding on appropriate antibiotic therapy.
Diagnosis and identification of the organism is critical and is made by needle aspiration and examination of the synovial fluid. The leukocyte count is usually over 100,000 per mL with over 90% neutrophils. Approximately 75% of nongonococcal infections are due to gram-positive cocci. Cases involving methicillin resistant Staphylococcus aureus (MRSA) have been documented and must be considered (21). Gonococcal infections are common in young adults and a presumptive diagnosis can be made if Neisseria gonorrhoeae is isolated from a primary source.
Management
Prompt arthroscopic irrigation and drainage, and initiation of appropriate antibiotic therapy are essential to minimize destruction of the articular cartilage thereby avoiding significant permanent consequences.
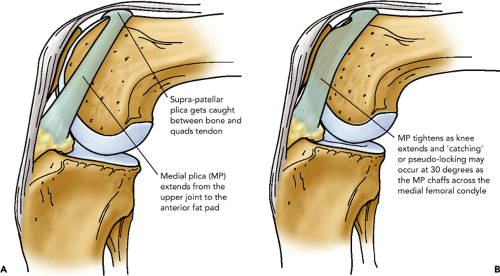
Anatomy
The knee anatomy relevant to the sports medicine physician is presented in Figure 31.1 and in other select diagrams throughout this chapter. The knee joint is supported by a muscular tripod; the quadriceps/patella/patellar tendon anteriorly and the hamstrings (HSs); semitendinosis, semimembranosis at the posteromedial corner and the biceps femoris at the posterolateral corner. This joint is further protected by a thick fibrous capsule and strong ligaments that prevent anterior (anterior cruciate ligament [ACL]), posterior (posterior cruciate ligament [PCL]), medial (medial collateral ligament [MCL]), lateral (lateral collateral ligament [LCL]), and rotatory displacement. In the immature skeleton, the distal femoral physis or the proximal tibial physis may be the weak links and subject to Salter-Harris fractures with sufficient varus and/or valgus force to the knee.
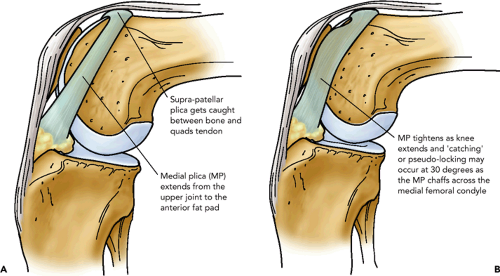
The thick fibrous capsule surrounds the joint and is well outlined when a major effusion is present (inverted U). There is a thin synovial lining inside of the capsule. Multiple compartments are present during the embryonic development of the knee. The compartments join together but with incomplete reabsorption of the connecting walls. The remaining “walls” are known as plica (a shelf). The clinically relevant medial plica originates from the suprapatellar plica (that extends in a transverse plane proximal to the superior pole of the patella) and extends medially to the anterior fat pad (see Figure 31.2).
The cruciate ligaments cross one another from their point of origin on the femur to the point of insertion on the tibial plateau. The MCL is a broad, long ligament extending from the medial femoral condyle to the medial tibia plateau at the level of the tibial tubercle. The shorter LCL originates from the lateral femoral condyle and inserts onto the head of the fibula. Significant injury to any of these ligaments may result in laxity and clinical instability.
The patellofemoral (PF) joint is the most common site for anterior knee pain among all ages, fitness levels and sporting activities. The quadriceps control patellar tracking keeping the patella centered within the femoral trochlea with knee flexion and extension. Quadricep fatigue or inhibition may disrupt PF joint mechanics.
The iliotibial band (ITB) acts to provide dynamic lateral stability as the band crosses the joint line and inserts
into Gerdy’s tubercle. A group of three muscles, the semitendinosis, gracilis, and sartorius insert medial to the tibia tubercle, and are collectively known as the pes anserine tendons. Both the ITB and the pes anserine tendons are common sites of overuse injury. The popliteus muscle originates from the posteriomedial tibia, forms a tendon that crosses underneath the LCL and inserts into the lateral femoral condyle anterior to the LCL. This tendon is an infrequent site of overuse injury or rupture.
into Gerdy’s tubercle. A group of three muscles, the semitendinosis, gracilis, and sartorius insert medial to the tibia tubercle, and are collectively known as the pes anserine tendons. Both the ITB and the pes anserine tendons are common sites of overuse injury. The popliteus muscle originates from the posteriomedial tibia, forms a tendon that crosses underneath the LCL and inserts into the lateral femoral condyle anterior to the LCL. This tendon is an infrequent site of overuse injury or rupture.
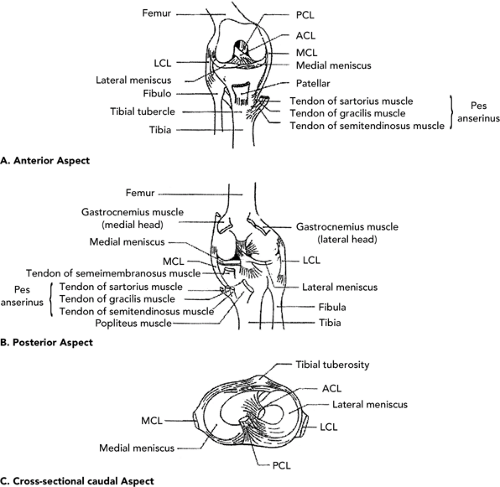 Figure 31.1 Anatomy of the knee. PCL = posterior cruciate ligament; ACL = anterior cruciate ligament; MCL = medial cruciate ligament; LCL = lateral cruciate ligament |
There are many bursae that surround the knee. The prepatellar bursa located directly over the patella and the suprapatellar bursa located superior to the suprapatellar pouch of the capsule can become inflamed and swollen following blunt trauma. Bursae associated with the ITB, pes anserine tendons, patellar tendon, LCL, MCL, and semimembranosis muscle may become inflamed as a result of overuse injury.
The menisci (22,23) are composed of a C-shaped (medial meniscus) and an O-shaped (lateral meniscus) that act as shock absorbers and distribute body weight evenly through the femoral condyles onto the articular surface of the tibia. Complete removal of a meniscus will in time result in severe degenerative arthritis due to an asymmetrical redistribution of forces. The medial meniscus is attached to the MCL and joint capsule and is sometimes involved in knee injury involving a valgus force. The lateral meniscus is not attached to the LCL and is less frequently torn. Wrestling is the only sport where an equal number of injuries to both menisci occur (24,25).
History (26)
A precise and accurate history is essential to formulate a thorough differential diagnosis. Site of pain diagrams correlate the anatomical site with the most likely sources of pain in traumatic (see Figure 31.3) and overuse injury (see Figure 31.4). It is not uncommon to identify incomplete rehabilitation as a factor in a knee injury. The mechanism of injury (MOI) provides insight into the
anatomical structures at risk as a result of the trauma and the physical examination confirms the extent of injury. Table 31.2 identifies the direction of force and the supporting ligaments and other structures at risk. Most overuse injuries result from training errors that must be identified and modified in order to prevent recurrence.
anatomical structures at risk as a result of the trauma and the physical examination confirms the extent of injury. Table 31.2 identifies the direction of force and the supporting ligaments and other structures at risk. Most overuse injuries result from training errors that must be identified and modified in order to prevent recurrence.
Take the opportunity to gather precise information and direct the conversation as needed by asking specific questions about the following: (a) MOI or training errors; (b) site and nature of pain felt and determine the current limitations to participation (often a 10-point pain scale can be effective in quantifying the pain); (c) previous injury, surgery, and rehabilitation to date; (d) upcoming events and how important it is for the athlete patient. (For the in-season athlete the goal will be symptoms control, strength maintenance, and return to play [RTP], whereas for the out of season athlete or a low priority sport, the goal will be to control symptoms by limiting activity with a major emphasis on strengthening to expedite full recovery), and (e) ask the athlete if there is anything else that should be noted.
Presenting knee problems may be atraumatic, with the absence of any known trauma or overuse, a result of a traumatic event, or the result of overuse. Different information is needed to form a differential diagnosis for each category.
Atraumatic
Describe for me what happened to your knee(s)?
Where do you feel the pain or discomfort? (See Figure 31.4)
When was the first time you felt the pain? If there is no history of trauma or overuse, it is still important to assume there may be an overuse component. Consider asking questions related to overuse.
Have you experienced any swelling? If yes ask, How much swelling is there at this time compared to what there has been? (This question is asked without looking at the knee, it is nonjudgmental and allows you to gain insight as to the point of reference of the athlete.) If the athlete answers yes to swelling ask, Has there been any recurrent swelling? If yes find out how much and how often. Have you noticed swelling, redness or stiffness in any other joints? Do you have any family history of arthritis? If yes ask about which family member, age and type and severity of arthritis. If index of suspicion is present, follow an arthritis work-up (osteoarthritis [OA], gout, pseudogout, rheumatoid arthritis [RA], juvenile rheumatoid arthritis [JRA], etc.) (see Table 31.3)
How intense is the pain? If the pain is moderate to severe at rest and the patient states that any movement of the knee causes intense pain, one must consider a septic joint (see section Emergencies)
Anything else you would like me to write down?
Traumatic (see Table 31.4)
Describe for me what happened to your knee(s)? Make sure you have a clear understanding of the MOI.
Was there a “pop” felt or heard? If yes, think ACL until proved otherwise, but realize there may also be a patellar instability issue. With a frank patellar dislocation, there is a “pop” felt when the patella relocates over the lateral femoral condyle. Less often,
there is a “pop” with a nondisplaced tibial plateau fracture or an osteochondral fracture. Rarely a torn meniscus will result in a “pop.” All of the above will most often result in an immediate swelling because of the bleeding into the joint.
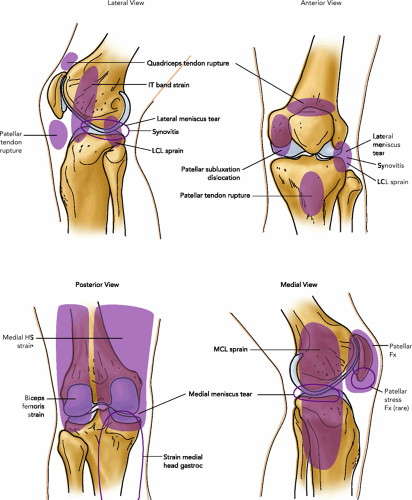
Figure 31.4 Differential diagnosis based on site of pain following overuse injury. HS = hamstring; PFP = patellofemoral pain; IT = iliotibial; LCL = lateral cruciate ligament.
TABLE 31.2 Predicting Knee Injury Using Traumatic Mechanism of Injury
Contact vs. Noncontact
Example in Sport
Structures Injured
Differential Diagnosis
Contact: Foot Planted
Valgus stress (force from outside knee that results in knee bent inward)
“Clip” in football
Soft tissue
Bone: immature skeleton
Bone: mature skeleton
MCL
Medial meniscus
ACL
Contusion
Saltar Harris fracture (distal femoral epiphysis)
Fracture distal tibia or avulsion MCL MCL sprain grade I–III
Possible torn meniscus
Possible ACL sprain grade I-III
Varus stress (uncommon, force directed from inside of the knee toward the outside)
Player “blind sided” and unaware that opponent was coming; hit on the inside of the knee
Soft tissue
LCL
ITB
Contusion
LCL sprain grade I–III
ITB strain
Hyperextension force
Blow to anterior knee
Soft tissue
Posterior capsule
ACL
Possible PCL if force persists
Contusion
Posterior capsular sprain
ACL sprain
PCL sprain
Forced flexion
Landing in flexed position; skiing
PCL
PCL sprain grade I-III
Posterolateral directed force in extended knee
Football
Soft tissue
Popliteal tendon
Contusion
Popliteal tendon rupture
Anterior force at the level of tibial tubercle or anterior tibia.
Catcher blocking the plate in baseball or softball
Soft tissue
PCL
Contusion
PCL Sprain grade I-III
Anterior, medial or lateral force directed at quadriceps
Soccer or rugby knee to quadriceps
Soft tissue
Quadriceps contusion, mild to severe, myositis ossificans
Noncontact Foot Planted
Weight bearing, rotation toward planted foot
ACL deficient knee
Ackward movement, but may occur in soccer, basketball, and football
ACL
Possible meniscus
Chondral surface
Possible meniscus
Chondral surface
ACL sprain Gr I–III
Torn meniscus 50% in acute injury grade III ACL, 4:1 ratio lateral to medial 4:1 ratio, medial to lateral
Osteochondral or chondral fracture
Weight bearing, rotation away from planted foot
Common movement in many agility sports
Patellar instability
Chondral surface
Patellar dislocation or subluxation
Osteochondral or chondral fracture
Any weight bearing with rotation
Common movement in many agility sports
Meniscus
Chondral surface
Torn medial or lateral meniscus
Osteochondral or chondral fracture
Jumping or landing
Jump shot in basketball
Quadriceps or patellar tendon
Complete rupture of quadriceps or patellar tendon
Falling with knee flexed landing on tibial tubercle
Soccer, football
PCL
PCL sprain grade I-III
MCL = medial collateral ligament; ACL = anterior cruciate ligament; LCL = lateral collateral ligament;
ITB = iliotibial band; PCL = posterior cruciate ligament.
TABLE 31.3 Evaluation and Significance of Knee Swelling
Effusion/Swelling
Timing
Anatomical Structures
Differential Diagnosis
Intra-articular swelling = effusion (see Table 31.5)
Most often post traumatic and associated with “pop”
Immediate (onset 2–6 hr)
Hemarthrosis
Most often 3–4+ effusion
Ligament injury, patellar instability, fracture, meniscus, synovial lining
ACL, patellar dislocation, osteochondral or tibial plateau fracture, tear in vascular portion of the meniscus, synovial contusion (if multiple ligaments are involved, suspect knee dislocation [emergencies])
Atraumatic effusion
Delayed
Capsule/synovial lining
Pigmented villonodular synovitis If pain is excessive, consider septic joint (emergencies)
Posttraumatic Effusion
Delayed (over 24 h)
Synovial fluid
Most often minor 1–2+ effusion
Meniscus, synovial lining, patellar instability, arthritis,
Torn Meniscus, reactive synovitis, patellar subluxation, OA
Most often activity related
Recurrent
Most often minor
Arthritis, meniscus, chondral surface
Degenerative meniscus, OA, chondromalacia patellae, possible old ligament injury
Extra-articular swelling
Post-traumatic
Immediate quadriceps trauma
Valgus stress
Result of trauma to quadriceps
MCL
Quadriceps contusion (may be difficult initially to distinguish from a major effusion)
MCL grade II-III
Extra-articular swelling; may be post-traumatic
Delayed
Difficult to distinguish outline of patella
Prepatellar bursitis
Extra-articular swelling
Overuse
Delayed
Various bursa
Site specific
Pes anserine, ITP, deep infrapatellar, stress fracture medial tibial plateau
Extra-articular swelling
Posterior knee
Delayed
Posterior capsule, bursa
Bakers cyst, lipoma, ganglion, semimembranosis bursitis
ACL = anterior cruciate ligament; OA = osteoarthritis; MCL = medial collateral ligament; ITP =.
Was there any swelling? How long was it before it began to swell? Any immediate swelling represents a hemarthrosis with consideration of the differential in B. Was there swelling by the next morning? A delayed swelling (over 24 hours) represents synovial fluid and may represent a torn meniscus, synovitis, OA, or a true chondromalacia patella. How much swelling is there at this time compared to what there has been? (This question is asked without looking at the knee, it is nonjudgmental and allows you to gain insight as to the point of reference of the athlete.) Also, when there is swelling, it may be intra-articular (effusion) or extra-articular such as with a Grade II MCL sprain (see Table 31.3).
Have you had any limitations in motion? (Your ability to fully bend and straighten out the knee.)
Have you experienced any catching, locking up or giving way of the knee (mechanical symptoms)? Catching or locking up (inability to fully extend the knee) suggest a loose body or unstable meniscus. If the athlete is currently unable to extend the knee ask, Have you been able to straighten your knee even once since the injury? If the answer is no, suspect a displaced bucket-handle tear of the medial meniscus. If the athlete has experienced any giving way episodes, it is important to ask, How many times has the knee given way? Did you experience any giving way episodes before the injury? If yes, suspect a previous injury. Also ask, When your knee gives way, is the sequence giving way followed by pain or is there pain felt before a giving way episode? If it is the former, suspect a chronic ligamentous injury. If the latter suspect a patellofemoral pain (PFP), iliotibial band syndrome (ITBS), medial plica, meniscus, tendonitis, or any overuse injury that can cause pain with quadriceps muscle inhibition and giving way.
Where are you feeling the pain? (See Figure 31.3)
Have you experienced any prior significant injury to either knee? What type of treatment did you have? Was your rehabilitation complete?
TABLE 31.4 Differential Diagnosis to Consider in Seated Position
Palpation
Numbers 1–10 should be considered in most examinations as it will provide information on PFP, medial plica syndrome, ITBS and patellar tendonitis, the most common overuse injuries. An effusion can be better identified in the supine position. Begin will less symptomatic or asymptomatic knee. It is helpful to consider a differential diagnosis as the examination is performed. The following is a suggested sequence to follow.
- (a) Tibial tubercle (immature skeleton; Osgood Schlatter’s disease, mature skeleton; ossicle within tendon, insertional patellar tendonitis, stress fracture of tibial tubercle.
- (b) Patellar tendon mid-body (superficial or deep infrapatellar bursitis)
- (c) Anterior joint lines (anterior synovitis found in 50% severe PFP, fat pad inflammation)
- (d) Medial joint line distal 2/3 (medial meniscus, reactive synovitis, MCL sprain, tibial collateral bursitis, DJD medial compartment)
- (e) Lateral joint line distal 2/3 (lateral meniscus, reactive synovitis, DJD lateral compartment)
- (f) Medial plica (medial plica syndrome)
- (g) Medial femoral condyle (friction rub from medial plica syndrome)
- (h) Lateral femoral epicondyle (ITB syndrome friction rub)
- (i) Medial and lateral patellar facets (PFP, patellar subluxation)
- (j) Inferior pole of the patella (patellar tendonitis, Sinding-Larsen-Johansson syndrome, patellar stress fracture if involves distal 25%) The following structures to be palpated as appropriate based on history
- (k) Patella (symptomatic bipartite patella, stress fracture, prepatellar bursitis)
- (l) Superior pole of patella (quadriceps tendonitis)
- (m) MCL (mid portion–same as no. 4, distal portion–same as no. 11)
- (n) LCL isolated by placing patient’s foot on opposite knee (figure 31.4 position) and palpating ligament (LCL sprain, popliteus tendonitis; insertion anterior to LCL)
- (o) Head of fibula (biceps femoris insertional tendonitis)
- (p) Neck of fibula (Common peroneal nerve injury, sprain of proximal tibiofibular joint)
- (q) Pes anserine insertion (tendonitis, bursitis, stress fracture of medial tibial plateau)
- (r) Posterior knee (capsular sprain, Bakers cyst vs. semimembranosis bursitis, hamstring strain, head of gastro strain)
- (s) Superior pole of patella (quadriceps tendonitis)
PFP = patellofemoral pain; MCL = medial collateral ligament; DJD = degenerative joint disease;
ITB = iliotibial band; LCL = lateral collateral ligament.
- (a) Tibial tubercle (immature skeleton; Osgood Schlatter’s disease, mature skeleton; ossicle within tendon, insertional patellar tendonitis, stress fracture of tibial tubercle.
Anything else you would like me to write down?
Overuse Injury
When did you first feel any pain? At what point did it become a disabling pain with activity that interfered with your ability to practice, participate in games or even in routine daily activities? Has there been any change in the character of the pain over time? The pain may begin as a shin splint but progress to a tibial stress fracture.
Where they any changes in your training 4 to 6 weeks before the onset of your pain? Any change in the duration or intensity of workouts? More interval workouts or hills? Any change in shoes or surface? Do you always run on the same side of the road? Down leg will supinate and up leg will pronate leading to ITBS or PFP.
Have you noticed any swelling? (See Table 31.3)
Please point out where you are feeling your pain? (See Figure 31.4)
Is your pain felt during and/or following activity? If pain is felt with activity ask, Is there a disabling pain with activity that prevents full participation? If there is only pain felt following activity with or without a nondisabling pain felt with activity, it will respond much differently that a disabling pain felt with and following activity.
Have you had any treatments to date? Have you made any modifications in your training? Important to document response or lack there of to any treatments to date.
What is on your schedule for the next 2 weeks? Important to find out about any upcoming events that the athlete is preparing for.
Describe a typical day for me? What do you feel like when you first wake up in the morning? How about
going up or down stairs at school? Do you feel any symptoms by lunchtime? Are symptoms related to how active you are on a given day? These questions can be helpful in defining the extant and severity of the symptoms.
Anything else you would like me to write down?
Physical Examination (27)
A variety of techniques and sequences are used to examine the knee. Each examiner may choose those techniques and sequences that fit one’s style. It is important to be thorough and realize that competence results from practice. Never be afraid to adopt a new or different technique if it will improve your ability as a clinician. Never be afraid to leave something out if it is redundant. The following are some techniques that have been proved to have clinical value.
The knee examination should be modified to accommodate the patient’s clinical presentation. For an acute severe injury, the examination should be carried out with the patient in the supine position; otherwise, if the sitting position is comfortable for the patient, identification of relevant landmarks will be facilitated for the examiner.
Many traumatic injuries and overuse syndromes affect very localized structures, which emphasizes the importance of knowing the functional anatomy and performing a precise examination (see Figures 31.3 and 31.4).
The biomechanical alignment and Q angle (if desired) can be noted in the standing position and throughout the examination as needed.
Biomechanical alignment. Note gait, genu varum or valgus, tibia varum, femoral anteversion, tibial torsion, arch type and heel forefoot alignment (forefoot varus or valgus). All of these factors may impact on knee mechanics.
Q angle. This is represented by the angle formed from the anterior superior iliac spine (ASIS) to the center of the patella from above, transected with a second line originating from the tibial tubercle to the center of the patella from below. Those individuals with an increased Q angle (females) or with the so-called miserable malalignment syndrome (femoral anteversion, tibial torsion, genu valgum, pes planus with a significant forefoot varus) are theoretically at higher risk for developing PFP. In clinical practice however, there are many other variables that contribute so that the role that an increased Q angle plays, is not a major predictive factor. The risk suggested by the Q angle, can be used to motivate compliance with rehabilitation. As opposed to PFP, the Q angle is more critical in the evaluation of patellar instability.
The knee examination in the seated position will include the following: (a) inspection looking for any bony or soft tissue swelling, bruising or muscle atrophy and (b) palpation (see Table 31.4).
TABLE 31.5 Evaluation of Effusion | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Steps included in the supine position include: (a) inspection, (b) palpation, (c) ligament testing, (d) apprehension testing, (e) meniscal testing, (f) muscle testing, and (g) functional testing.
Inspection in supine position. Note effusion (see Table 31.5), swelling, soft tissue or bony deformity, muscle atrophy, ecchymosis, erythema, abrasion, or surgical scares.
Bony and Soft Tissue Palpation
Examination in Supine Position allows for evaluation of thigh muscle atrophy or swelling.
Thigh Muscle Atrophy or Swelling
Pen marks can be placed mid thigh 5 and 15 cm above superior pole of patella to measure thigh circumference. The measurement is most accurate when thigh muscles contract. Ask the athlete to tighten the quadriceps and lift the leg off the table. An atrophy or swelling that is equal to or greater than 1 to 2 cm is felt to be relevant.
Ligamentous Evaluation
Table 31.6 gives the details of the evaluation of the laxity of ligaments.
Anterior/Posterior Stability Evaluation
ACL evaluation/Lachman (28). The ACL can be evaluated with the Lachman, Pivot Shift Test and the Anterior Drawer. The Lachman is the most reliable test for isolated ACL tears. It is performed by grasping the distal femur and proximal tibia (see Figure 31.5). With the knee in 15 to 20 degrees flexion, gently increase the anterior force applied to the tibia while
stabilizing the femur. The force is directed in a pure anteroposterior (AP) plane. It is important to encourage the athlete to relax the HSs or the Lachman cannot be effectively done. The amount of anterior excursion, as well as the quality of the end point, should be noted. Any movement more than 3.5 to 5 mm (1–2+) is consistent with a complete rupture of the ACL. A “soft end-point” even without excessive excursion is consistent with a complete rupture of the ACL (HSs must be relaxed). Following the Lachman test and before additional testing, it can be very effective to perform the Apprehension test.
TABLE 31.6 Ligamentous Laxity Assessment
mm Movementa
Grade
5
1+
10
2+
>10
3+
aLaxity is relative, based on the laxity found in the control knee (i.e., control 6-mm movement compared with 10-mm movement on the injured side). Difference would be 4mm = 1+ laxity. While there may be a difference in the laxity of ligaments between individuals, comparing the same ligament in knees of the same individual should be symmetrical.
Patellar stability testing (the Apprehension test). To test for patella instability, the examiner following Lachman testing can make a slight adjustment of both thumbs. They are placed along the medial patellar border at the 1:30/4:30 positions for the right knee and 10:30/7:30 for the left knee (see Figure 31.6). A direct lateral force is applied and the knee is gently flexed from 0 to 30 degrees while continuing the lateral force to the medial border. At 30 degrees, the lateral femoral condyle is at its shallowest point. A positive apprehension sign occurs when the patient senses impending subluxation and simultaneously contracts the quadriceps, sits up, grasps the knee and has eyes the size of baseballs staring at you.
ACL evaluation/pivot shift. The Pivot Shift Test identifies anterolateral rotary instability, only present in the ACL deficient knee. The test reproduces the exact mechanism of instability that the patient experiences with giving way episodes. This test is performed by internally rotating the tibia (to keep the tibia in a reduced position), placing a valgus stress and an axial load on the knee (to accentuate subluxation) (see Figure 31.7). The knee begins in full extension
and is gently flexed. Anterolateral subluxation of the lateral tibial plateau is documented by the examiner and recognized by the patient as what happens when the knee gives way. The Pivot Shift is technically more difficult to master and is recommended only for sports medicine physicians. Primary care physicians should focus on the Lachman test.
PCL evaluation/posterior drawer. There may be a negative reverse Lachman test (the Lachman test can seem to be completely normal with solid end points in both anterior and posterior directions), hence the gold standard for a PCL sprain is the posterior drawer test. In a chronic injury with excessive laxity, it can be difficult to distinguish between PCL and ACL involvement. In both instances, there is a significant amount of anterior excursion. The PCL-deficient knee begins from an abnormal posterior position and moves forward to the normal position whereas the opposite is true with a chronic ACL starting in a normal position and moving to an abnormal forward position. The MOI if known may help indicate which ligament is involved but a careful physical examination is the key to diagnosis.
Drawer testing. The Anterior Drawer is much less sensitive than the Lachman or Pivot Shift test for confirming the diagnosis of an acute or chronic ACL injury. The Posterior Drawer as mentioned earlier is the gold standard for PCL evaluation and is performed with the patient in the supine position, with the hip flexed to 45 degrees and the knee to 90 degrees and the examiner sitting on the patient’s foot to stabilize the tibia (see Figure 31.8). A view from the side may demonstrate a “posterior sag sign” with a posterior sagging of the tibial tubercle on the injured side. The hands are placed behind the proximal tibia and the tibia is pulled toward the examiner. It is important to check for relaxation of the HS muscles, as the examination is difficult to perform in the presence of contracting HSs. The test is performed with the foot pointing straight ahead. The thumbs are placed over the anterior tibial shelf and amount of shelf is appreciated. Forward movement is consistent with ACL laxity (comparison is relative to the uninjured knee). Backward movement, loss of tibial shelf (anterior tibia becomes flush with the femoral condyles) is consistent with PCL laxity. The technique for evaluation of the posterolateral corner at times associated with a PCL injury is discussed in the section on PCL Injuries.
Medial/Lateral Stability Evaluation
Medial stability. Valgus stress is applied to the knee in full extension to test the integrity of the MCL and cruciate ligaments. Valgus stress applied to the knee at 30 degrees flexion (see Figure 31.10) isolates the MCL as cruciate ligaments are relaxed. Laxity greater than that of the control knee indicates a sprain of the MCL. It is important to identify the quality of the end point when stressing the knee. Increased laxity but with a solid, abrupt end point indicates a partial tear of the MCL, while a soft, mushy end point and 3+ laxity indicates a complete rupture of the MCL. Splinting by contraction of the HSs or adductors may make the examination difficult. It is also important to note the presence of pain during the examination. Absence of pain may indicate laxity from a previous injury or a complete rupture of the MCL. Isolated Grade III sprains of the MCL are uncommon but may be less painful than the common Grade II sprains.
Lateral stability. A varus stress is applied to the knee in full extension to test the integrity of the LCL, ITB, popliteus muscle, lateral capsule, and cruciate ligaments. As in the preceding text, increased laxity as compared to the uninjured knee indicates injury. Varus stress applied to the knee at 30 degrees flexion isolates the LCL (see Figure 31.11). It is important to note that most people have a degree of physiological laxity in this position. By gently placing the lateral
ankle of the injured knee onto the opposite knee, “Figure of 4 position” (see Figure 31.12), the LCL can be readily palpated.
Meniscal Evaluation
Meniscus evaluation. A simple yet very effective way to assess a knee for a possible meniscal injury is to fully flex the knee (see Figure 31.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree