Percutaneous Ultrasound Tenotomy for Epicondylitis
Bernard F. Morrey
TRENDS IN THE TREATMENT OF CHRONIC TENDINOPATHY
Over the last several years, a number of common features have emerged as trends in the treatment of chronic tendinopathy. These trends are summarized in Table 26-1. A common feature is the goal to first more accurately isolate the lesion by ultrasound or MRI (1,2) and then to treat the process in a less invasive, percutaneous fashion that is well tolerated with minimal morbidity.
IMAGE-GUIDED PERCUTANEOUS TENOTOMY AS A TREATMENT FOR EPICONDYLITIS
Rationale
The utility of ultrasonic-guided intervention for musculoskeletal conditions has been recognized since the early 1980s with the description of assist draining an abscess (3). Ultrasound-guided percutaneous tenotomy was described as early as 1999 for the treatment of patella tendinopathy (4), and the utility of ultrasound-guided percutaneous tenotomy with a needle or knife blade has been subsequently documented (5,6,7 and 8).
Today, most cataracts are treated quickly, safely, and effectively as an outpatient with ultrasound ablation. The same rationale and concept have now been applied to the management of chronic tendinopathy. Ultrasound energy is imparted through a device, the TX1 (TenexHealth, Lake Forest, CA), which is roughly the size of a 16-gauge needle and hence is easily visualized using standard 5 to 10 MHz ultrasound imaging. This offers a safe and effective tool and process to perform percutaneous tenotomy.
INDICATIONS/CONTRAINDICATIONS
Indications
The ideal candidate is a patient who has had symptoms for approximately 3 months or longer and has failed nonoperative management with traditional treatment modalities. Patients in whom the lateral epicondylitis is interfering with their lives, particularly their employment, are considered candidates for earlier intervention. Because of the safety characteristics, this may also be used, in conjunction with ultrasound imaging, in the treatment of failed surgical procedures.
TABLE 26-1 Trends and Desirable Characteristics in the Procedural Management of Epicondylitis | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Contraindication
There are no absolute contraindications. When the process is improving with eccentric exercises, rest, splinting, etc., when the symptoms are more of a nuisance that can be tolerated, the intervention is deferred.
ULTRASOUND-IMAGING OF TENDINOPATHY
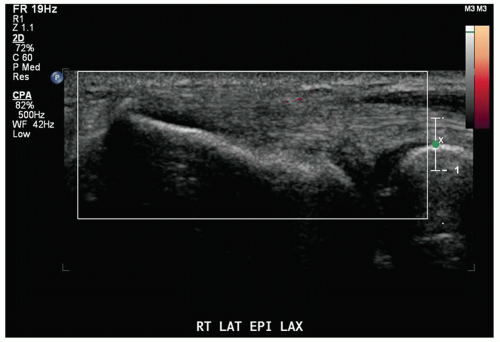
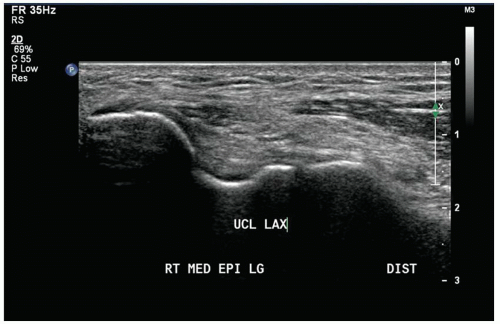
The pathology of a diseased tendon has been well characterized as loss of contour and edema and often the presence of an area of “hypoechogenicity,” which is felt to represent the portion of the process. Blinded studies have revealed a sensitivity of 90%, specificity of 89%, and a diagnostic accuracy of 94% (9). Extensive experience with ultrasound as a diagnostic tool is not required. The ability to visualize the lateral epicondyle and radial head is straightforward (Fig. 26-1). Similarly, the medial epicondyle and the ulnar nerve are readily identified medially (Fig. 26-2). The normal tendon
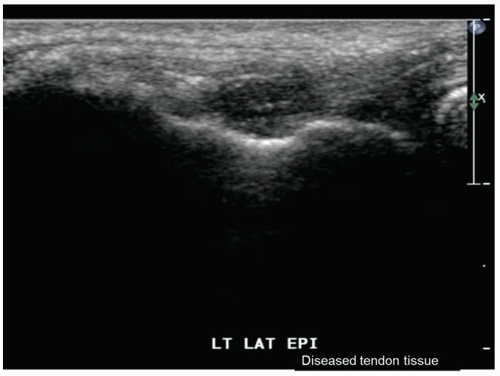
appears more homogenous and more uniform in appearance by ultrasound image. Tendinopathy exhibits a “hypoechoic” image that appears as a black defect in the tendon (Fig. 26-3). However, the possibility of a hypoechoic artifact due to lack of proper orientation of the sensor to the tissue to be imaged must be recognized (10).
appears more homogenous and more uniform in appearance by ultrasound image. Tendinopathy exhibits a “hypoechoic” image that appears as a black defect in the tendon (Fig. 26-3). However, the possibility of a hypoechoic artifact due to lack of proper orientation of the sensor to the tissue to be imaged must be recognized (10).
 Get Clinical Tree app for offline access 
|