Penetrating Pulmonary Injuries
Juan A. Asensio
Luis M. García-Núñez
Patrizio Petrone
“War surgery has rendered surgery of the lung easy and without any particular danger. It is our earnest hope that the new field opened by the horrors of war may be utilized for the benefit of mankind.”
—Pierre Duval, MD
France 1919
France 1919
Thoracic trauma accounts for approximately 20% to 25% of all trauma deaths; however, most of the thoracic injuries can be managed nonoperatively with insertion of chest tubes. Approximately 10% to 15% will require operative intervention to control life-threatening hemorrhage. What is not known is the true incidence of pulmonary injuries requiring operative intervention. Most of the thoracic injuries requiring surgical intervention will be due to penetrating mechanisms of injury such as gunshot wounds (GSW), stabwounds (SW), and shotgun wounds (SGW). Much less common are blunt thoracic injuries requiring operative intervention. Similarly, a significant number of pulmonary injuries occur in association with injuries to thoracic vascular structures or the heart. Thoracoabdominal injuries represent a difficult dilemma for the trauma surgeon in deciding which cavity to access and when.
Factors associated with survival for penetrating pulmonary injuries requiring surgical intervention include the type of wounding agents, that is, GSW versus SW or SGW, prehospital transport time, presence of shock at the scene or upon arrival, loss of the airway, and number of associated injuries. Patients sustaining penetrating pulmonary injuries arriving in cardiopulmonary arrest at a trauma center which require emergency department thoracotomy (EDT) have an extremely poor prognosis.
CLINICAL DIAGNOSIS
The clinical presentation of patients sustaining penetrating pulmonary injuries ranges from hemodynamic stability to cardiopulmonary arrest. Patients with penetrating pulmonary injuries may present with symptoms and signs of pneumohemothorax or an open pneumothorax with a partial loss of the chest wall; or may also present with a tension pneumothorax or hemothorax.
Patients with penetrating pulmonary injuries may rarely present with a pneumomediastinum upon auscultation. The Hamman crunch—a systolic crunch may be detected upon auscultation in these patients. Similarly, they may also present with a pneumopericardium, detected by auscultating Brichiteau’s windmill bruit (bruit de moulin). Patients with penetrating pulmonary injuries may rarely present with true hemoptysis; they may also present with symptoms and signs of associated cardiac injuries.
During the evaluation of these patients, the trauma surgeon must be cognizant that the thoracic cavity is composed of both a right and left hemithoracic cavity as well as an anterior, posterior, and superior mediastinum because missiles or other wounding agents may often traverse one or more of these cavities. Similarly, missile trajectories are often unpredictable and frequently
create secondary missiles if they impact on hard bony structures such as the ribs, spine, and sternum thereby creating the potential for associated injuries and greater damage.
create secondary missiles if they impact on hard bony structures such as the ribs, spine, and sternum thereby creating the potential for associated injuries and greater damage.
CLINICAL INVESTIGATIONS
Patients presenting with penetrating thoracic trauma may be studied by invasive and noninvasive means.
Noninvasive Techniques
Noninvasive techniques include:
Trauma ultrasonography (focused assessment with sonography for trauma [FAST])—will reliably diagnose and exclude an associated cardiac injury and can also diagnose the presence of a hemothorax
Chestx-ray—will provide an assessment of the following:
Both hemithoracic cavities
Mediastinum
Pericardium
Extra-anatomic air: peneumomediastinum, pneumopericardium, or subcutaneous air
Electrocardiogram (ECG)
Invasive Techniques
Invasive techniques can be both diagnostic and therapeutic.
Insertion of chest tubes in one or both hemithoracic cavities will serve to:
Evacuate air
Evacuate and quantify blood, evaluate whether it is arterial or venous
Detect massive air leaks
Establish an indication for thoracotomy
SURGICAL DECISIONS IN THE EMERGENCY DEPARTMENT
For patients that present in cardiopulmonary arrest, it will be necessary to proceed to EDT. With the simultaneous insertion of a large-bore chest tube in the right hemithoracic cavity, the left anterolateral thoracotomy may be extended into bilateral anterolateral thoracotomies if required. For patients who present with systolic blood pressure (BP) ≤80 mm Hg, insert bilateral chest tubes and resuscitate per Advanced Trauma Life Support (ATLS) protocol. If patient remains unstable, transport immediately to the operating room (OR). If patient stabilizes, institute an investigative workup. For patients presenting with thoracoabdominal injury, insert chest tube or tubes. Transfer expediently to OR for abdominal exploration and reassess the need for thoracotomy.
OPERATIVE MANAGEMENT
Indications
Indications for thoracotomy in patients sustaining penetrating thoracic injuries include the following:
Cardiopulmonary arrest
Impending cardiopulmonary arrest upon arrival in the emergency department (ED)
Evacuation of 1,000 to 1,500 mL of blood upon initial placement of chest tube
Evacuation of ≥ 1,000 mL of blood upon placement of chest tube and ongoing blood loss
Tension hemothorax
Large retained hemothorax
Massive air leak from chest tube
Settings
Thoracotomy may be performed in the ED or in the OR. For patients presenting with cardiopulmonary arrest proceed immediately to EDT. The objectives of EDT include the following:
Resuscitation of agonal patients with penetrating cardiothoracic injuries
Evacuation of pericardial tamponade if there is an associated cardiac injury
Direct repair of cardiac injuries, if there is an associated cardiac injury
Control of thoracic hemorrhage
Prevention of air embolism
Perform cardiopulmonary resuscitation, which may produce up to 60% of the normal ejection fraction (EF)
Control pulmonary hemorrhage
Crossclamp pulmonary hilum
Crossclamp descending thoracic aorta
Adjunct Surgical Maneuvers
The trauma surgeon must be cognizant of the physiologic effects of some of the adjunct surgical techniques employed to deal with cardiopulmonary injuries. Each of these maneuvers may be instituted in the ED or in the OR. Each has both positive and negative effects.
Pulmonary Hilar Crossclamping
The positive effects of pulmonary hilar crossclamping include the following:
Preservation and redistribution of remaining blood volume
Improvement in perfusion to contralateral uninjured lung
Control of hilar hemorrhage
Prevention of air emboli
The negative effects of pulmonary hilar crossclamping include the following:
Rendering crossclamped lung ischemic
Imposing a great afterload onto the right ventricle (RV)
Decreasing oxygenation and ventilation to crossclamped lung
The unknown effects of pulmonary hilar crossclamping include the following:
Length of safe crossclamp time
Incidence of pulmonary reperfusion injury to both the injured and uninjured lung
Thoracic Aortic Crossclamping
The positive effects of thoracic aortic crossclamping include the following:
Preservation and redistribution of remaining blood volume
Improvement of coronary/carotid arterial perfusion
Reduction of subdiaphragmatic blood flow
Increases in the left ventricular stroke work index (LVSWI)
Increased myocardial contractility
The negative effects of thoracic aortic crossclamping include the following:
Decreasing blood flow to the abdominal viscera to approximately 10%
Decreasing renal blood flow to approximately 10%
Decreasing blood flow to the spinal cord to approximately 10%
Inducing anaerobic metabolism
Inducing hypoxia/lactic acidosis
Imposing a great afterload onto the left ventricle (LV)
May rarely cause paraplegia
The unknown effects of thoracic aortic crossclamping include the following:
Length of safe crossclamp time
Incidence of reperfusion injury
Emergency Department Thoracotomy
The technique for EDT may be used for patients sustaining penetrating pulmonary injuries arriving in cardiopulmonary arrest. This technique is outside of the scope of this chapter and is described in another chapter in the textbook.
Operating Room
The trauma surgeon must be familiar with the use of these special instruments that are needed to access the thoracic cavity as well as to retract, manipulate, and surgically intervene in the thoracic structures and lung (see Fig. 1). These instruments include the following:
Doyen costal elevators (right and left) (see Fig. 2)
Alexander periostotome (see Fig. 2)
Cameron-Haight periosteal elevator (see Fig. 2)
Bethune rib shears (see Fig. 3)
Stille-Horsley bone cutting rongeurs (see Fig. 3)
Lebsche knife and mallet (see Fig. 3)
Rib raspatory
Finochietto retractor
Davidson scapular retractor (see Fig. 4)
Allison lung retractors (see Fig. 4)
Semb lung retractors
Nelson lung dissecting lobectomy scissors (see Fig. 5)
Metzenbaum long dissecting scissors (see Fig. 5)
Tuttle thoracic tissue forceps (see Fig. 5)
Duval lung forceps (see Fig. 6)
Davidson pulmonary vessel clamps
Sarot bronchus clamps (right and left)
Bailey rib approximator (see Fig. 7)
Berry sternal needle holder
Vascular clamps
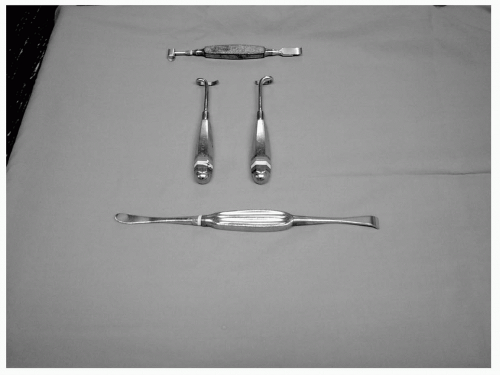 Figure 2 Alexander periostotome. Right and left Doyen costal elevators and Cameron-Haight periosteal elevator. |
Adjuncts
Double-Lumen Tubes
Double-lumen tubes are invaluable adjuncts in the management of penetrating pulmonary injuries. Although more difficult to insert by the anesthesiologists, double-lumen tubes are designed to ventilate either the right or left lung selectively. There are two types of double-lumen tubes, one designed for the left and one designed for the right mainstem bronchus (see Fig. 8). By inflating the balloon that occludes either the right or left mainstem bronchus, the lung can be collapsed, thereby allowing the trauma surgeon to operate on a collapsed and still lung.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










